Having a Happy Thanksgiving with Insulin
What do you think about when I say the words mashed potatoes, stuffing or pumpkin pie?
Most people hear those words and think "mmmmmm, it must be Thanksgiving" but some of us immediately begin to wonder how many carbohydrates are in stuffing. Many of the people who live with or care for someone who lives with diabetes, begin to panic. Instead of family and football they begin to think about Thanksgiving as a day that is trying to defeat them, they immediately feel stress and either decide to, sort of just give up and "do their best" or search for the measuring cups focused on getting the carb counts of every tasty Thanksgiving treat exactly right. In my opinion; there is a better response.
When I'm giving my daughter Arden insulin at a meal I focus on two things - How insulin works in her body and about how many carbs are in the food she is eating. In an effort to keep this, if you'll pardon the pun, digestible... I'm going to break this post into individual thoughts on subjects.
Questions I ask myself before I begin...
Is it more important to know A. exactly how many carbs are in a scoop of potatoes or B. how long it takes for insulin to begin to effect the blood sugar and how long it lasts in the body? - Answer is B
Will the day include a lot of grazing, am I planning for set meal times or is it both?
Do I have a reasonable understanding of the amount of carbs in the foods that will be consumed?
Am I afraid of insulin? - Be honest with yourself
My Goals...
My blood glucose goals for Arden are simple, yours should be too...
I am trying to maintain the steadiest blood sugars as I possible can. I want to avoid spikes and significant lows.
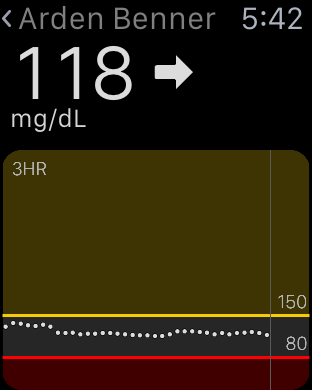
I consider a BG over 150 (after food) a high blood sugar.
I do not want Arden's BG to fall below 75 but steady at that number is a huge win, especially today.
For CGM users: I don't want to see arrows pointing straight up or straight down. If I do, I've mistimed insulin, miscalculated carbs or (for pump users) would have benefited from extending my bolus. When we were non CGM users: If Arden's BG is above 150-160 forty-five minutes after your mealtime bolus, you probably didn't use enough insulin. More insulin, more testing.
I want to create a stress free, carefree and happy day without frying my brain.
Insulin...
I have two steadfast rules about managing my daughter's type 1 diabetes. Read them, memorize them, live by them.
1. It is far easier to stop a low or falling blood glucose then it is to return a high blood sugar to a safe range. In my experience most low or falling BGs can be stopped and steadied in a short amount of time, maybe 15 minutes. A high BG can take 3 to 5 hours to return to a safe place. I'll say it again. It is easier to stop a fall or a low then it is to effect a high. This thought guides everything I do with insulin.
2. If Arden's BG is high any time after a meal (140-150), I did not use enough insulin at the correct time. Two VERY important considerations in this sentence, they are AMOUNT of insulin and the TIMING of the bolus relating to when food consumption begins.
Before we move on I want to say this, these are my rules but you know as well as I do that diabetes will, on some random day, act in no way like you expect. That is a fact of living with manmade insulin. I refuse however to allow the fear of that random day to make me except high BGs on all of the other days. I would rather battle a low a few times a month then live with a daily average BG that is any higher than it needs to be. Bold with insulin!
Lets talk about giving insulin for a meal...
There are generally one of three situations I experience before a meal. 1. A higher BG then I want, 2. A lower BG then I want, 3. A BG in our comfort range. All of these may be steady, rising or falling.
Let’s have some examples:
Step one for each possible situation is to pre-plan. Don’t start thinking about insulin at 4:55 if dinner is at 5, if that’s what you are doing... I’m willing to bet you see a lot of high BGs after food.
If our dinner is at 5 pm, I want to find out what Arden's BG is at 4 pm.
If Arden’s BG is 160 at 4 pm I would bolus for the 160 with the goal in mind of getting it as close to 90 as I could by 4:45 pm because (in this example) at 4:45 pm, I am bolusing for dinner. Here’s me counting carbs. Scoop of potatoes… eh 30. turkey 0, gravy, let’s call that 7, probably have two dinner rolls… I’ll call that 30, corn lets say 10, green veggies nothing. Okay that’s about 80, how much insulin is 80 carbs? Last thing I do is ask myself if the amount of insulin that 80 carbs indicates sounds like enough or too much? “Sounds like” means based on my past experiences with similar meals. If it doesn’t, I adjust it manually. One way or the other I’m hoping to have a 90 BG 15 minutes before the meal begins and I am bolusing with the thought that the mealtime insulin (In Arden) won’t begin to work for at least 15 minutes. The goal is for her BG to be 80ish when two things happen. 1. Her mealtime insulin begins to work and 2. The carbs from the food begin to have an effect on her BG. I want these things to happen at the same time when her BG is around 80. Then I watch the struggle between insulin and carbs play out on her Dexcom CGM. Most times this results in no spike and a steady BG for the next two hours. Adjustments (In Arden) may be needed around the two hour mark. More insulin, some carbs… one never quite knows.
A steady and in range BG gets the same pre bolus. Again, I want the struggle between the carbs and insulin (insulin pulling the BG down, carbs pulling it up) to happen as close to the 70-80 range as possible.
If Arden’s BG is low or falling an hour before dinner I only want to bump it ever so slightly. I don’t want it rising or high at 4:45. On the lower side is a great way to approach a meal - But you still have to pre bolus. I can’t say to myself, “her BG is 80 at 4:45 pm so I can’t pre bolus”. I have to trust the process, I have to trust that new insulin won’t cause a low for at least the amount of time that I believe it takes for the pre bolus insulin to begin working.
In the end, I can count the amount of times on one hand that a meal has gone well without a significant and well timed pre bolus. Only you know how long it takes for insulin to begin working in you or your child, so adjust accordingly with great deference to how long it takes the food to begin to effect the BG.
Remember, it is easier to effect a low than it is to correct a high....
I know there is a ton of other variables that I haven’t discussed. What if my child is too young to properly assume how much they will eat… in that situation I'd pre bolus half and then get the rest of the insulin in as soon as I could confirm that the food will be eaten. Easier with a pump sure, but even when you are injecting... it’s either two shots at dinner or one shot at dinner and another an hour later while you are battling a 300 BG. Which sounds better to you?
Arden has a CGM which makes all of this so much easier. I can see when she’s falling 5 minutes before we eat and hand her a roll. I can see the speed and direction that her BG is moving. No doubt what I am talking about is easier with a CGM but it is not impossible without one. Pre bolus (or inject), test 45 minutes later, test again 2 hours later. Stay on top of the BG.
Don’t fall prey to the drama! Don't ell yourself that, “I did what the endo told me” or “I counted the carbs, what else can I do”. That's all bull%$#&. You can do plenty with a positive attitude and a calm reaction to the things that don’t go as planned. Keep it easy in your mind; BG too high, need more insulin. Too low, need more carbs.
Is it a grazing day? Try using a temp basal rate. Perhaps an increase of (maybe) 30% to start, then adjust as needed. Don’t be afraid to let it run all day and don’t forget that the effects of a new basal rate may not be visible on a BG for 30 minutes to an hour. Also, when you stop a temp basal, it will take that much time to return to a level that you are accustom to.
I won’t let a BG that has gotten crazy high ruin Arden’s day... I crush it with insulin. Then test often or watch my CGM closely - sometimes both. If it falls too far or too fast, I catch the fall with a fast acting liquid carb. I give myself enough time to treat the fall without having to over treat - stay off the rollercoaster! Sometimes the hardest thing to do is to just wait and retest, I know, but that is how you will avoid chasing highs and lows all day. At some point you have to say to yourself, "we need to find a plateau and start over".
Last things and this is important. Lots of insulin is going to be used today. Watch your overnight BGs closely. Look for lows, unexpected falls and even high BGs from those carbs that just won’t digest and be gone. No telling which reality you’ll experience over night. Best to be on the look out. Give yourself a chance to battle on a level playing field, don't begin Thanksgiving with a pump site that is failing or on it's way out. Get your tech going and stable before the stuffing hits the table.
Wishing your family a very Happy Thanksgiving… don’t forget my disclaimer nothing you read here today is to be taken as advice, medical or otherwise. I’m just telling the story of how I manage my daughter’s BGs. Okay, thats enough diabetes talk for me today, I have to got make the stuffing!
Go kick some carbs right in their ass! You can do it...
Judge: Medicare Must Cover CGM for T1D Patient
This article will be referenced in episode 39 of the Juicebox Podcast (to post at midnight 11/23/15). A conversation with Insulet's CCO Shacey Petrovich.
reposted from Medpage Today
by Parker Brown
Staff Writer, MedPage Today
A Medicare provider must cover a continuous blood glucose monitor (CGM) for one of its patients with type 1 diabetes, an administrative law judge has ruled.
The patient, Jill Whitcomb, had recently become eligible for Medicare, which does not cover continuous glucose monitoring devices, provided through United Healthcare of Wisconsin/Secure Horizons. Whitcomb has had type 1 diabetes for more than 35 years, with diabetic neuropathy and a history of hypoglycemia unawareness. A video of Whitcomb having a severe episode of hypoglycemia when she was not using a CGM because she lacked a Certificate of Medical Necessity from the doctor was used as evidence in a trial earlier this year.
United has not yet offered to cover the device and has until Dec. 14 to appeal the decision, said Dan Kraft, Whitcomb's caretaker.
Courts may be forcing CMS' hand for coverage of continuous glucose monitors
George Grunberger, MD, president of the American Academy of Clinical Endocrinologists (AACE), said in an interview with MedPage Today that he has been following this case with interest for several years. The AACE has tried to convince the Centers for Medicare & Medicaid Services to cover CGM for patients with type 1 diabetes who age into Medicare coverage, he added.
"All of our meetings, petitions, and lobbying have met with rejections thus far in spite of uniform recommendations of all relevant professional societies," Grunberger said. "This ruling will hopefully re-energize the efforts to bring 21st century thinking into Medicare decisions. It's all about safety, not just better care for our insulin-requiring patients."
Since the ruling last month, other administrative law judges have cited Whitcomb's case and have ordered that CGMs be covered for the plaintiffs, Kraft said. He provided a document of a recent ruling in which the judge found that the Whitcomb decision was "well reasoned and on point" and that "coverage of a continuous glucose monitor should turn on whether or not the item is medically reasonable and necessary for the beneficiary."
The costs of the monitors and supplies can be substantial: the device alone can cost $400 to $2,000, and the associated consumables can add up to $300 a month. But Medicare considers the device to be "precautionary" and therefore not eligible for coverage.
The court disagreed, ruling that the CGM falls under what Medicare calls a Durable Medical Equipment statutory benefit and is eligible for coverage. The judge also concluded that the device is "medically reasonable and necessary" for Whitcomb, citing evidence by the American Diabetes Association that CGM, "in conjunction with intensive insulin regimen, is a useful tool to lower A1C in adults with type 1 diabetes mellitus, and for those with hypoglycemia unawareness and/or frequent hypoglycemic episodes."
The judge wrote in the final decision that it was clear that Whitcomb was a "brittle diabetic" and that the device is medically reasonable and necessary in her case.
Appealing Medicare decisions is a five-step process. In 2013, an administrative law judge concluded that United must cover the device for Whitcomb, but United filed a request for a review by the Medicare Appeals Council -- the fourth step. That council reversed the decision, according to court documents, and Whitcomb and her attorney filed a complaint in U.S. District Court in November of that year.
But in May 2015, the district court remanded the case to the Secretary of Health and Human Services, saying that the secretary had erred in one of her conclusions. The Medicare Appeals Council vacated its earlier decision and the case was sent to the Office of Medicare Hearings and Appeals, where the latest decision was issued and United was ordered to process Whitcomb's claim.
"As far as moving forward, it will take patients themselves, individually and through patient advocacy groups, to pressure their legislators to change the Medicare coverage language to recognize the tangible benefits this technology represents to their constituents' lives," Grunberger said. "The professional societies have done their part in incorporating the technology into their position statements and guidelines."
Have Questions for Dexcom? Ask them here!
Your questions for Dexcom on the Juicebox Podcast...
Soon I'll be interviewing Mike Mensinger from Dexcom for my podcast. Mike is the Director of Mobile and Cloud Services Software Development at Dexcom - in short, Mike knows all about the apps and software at Dexcom and we are going to get to pick his brain, ask questions and offer suggestions.
At the moment we are in the middle of working out a time that works for us and will be recording this podcast episode either in the next few days or sometime next week. If you have something you'd like to add to the conversation don't hesitate. Leaving your thoughts as a comment on this post will help me to keep everything in one place but if you have something that you feel is private to add, feel free to email me.
Thanks in advance for participating! I'll do my best to get everyone's questions in during the time that Mike and I have together. In the meantime you may want to listen to my podcast episodes with Dexcom's CEO Kevin Sayer and their EVP Steve Pacelli.
The Juicebox Podcast is available online, at iTunes, with Stitcher and everywhere fine podcasts are heard.
You Can Help to Create CGM Medicare Coverage
If you speak up, things will change!
I am a huge proponent of continuous glucose monitoring and believe that everyone deserves it's benefits and protection if they want it. Please take a moment to help the JDRF give a friendly push to our legislators. Doing the right thing for older people who have type 1 diabetes is the least that should be done. Your participation only takes a few moments and I've seen the JDRF's actions help issues like this in the past. If you speak up, things will change! Thank you, Scott
One Voice Calling for Medicare Coverage of Continuous Glucose Monitors (CGMs)
We need your help. Ask the U.S. Senate and U.S. House of Representatives to cosponsor bipartisan bills to ensure people over 65, and who are Medicare-eligible, have access to life-saving CGMs!
The Co-Chairs of the Senate Diabetes Caucus have reintroduced important bipartisan legislation (S. 804)
—the “Medicare CGM Access Act of 2015”—that would facilitate Medicare coverage for continuous glucose monitors (CGMs) and help pave the way for the next generation of CGM-related technologies, such as artificial pancreas (AP) systems.
This legislation now joins a bipartisan companion bill, (H.R. 1427), the “Medicare CGM Access Act of 2015,” introduced in the U.S. House by the leadership of the Congressional Diabetes Caucus.
But we still need your help! Please take a few minutes to:
- Email your Representatives and ask them to support H.R. 1427, the “Medicare CGM Access Act of 2015.”
- Email your Senators and ask that they support S. 804, the “Medicare CGM Access Act of 2015.”
After you complete these two simple action steps, please ask your friends, family, neighbors and coworkers to do the same! And spread the word on your favorite social media pages using the hashtag #MedicareCoverCGM.
Why CGMS should be covered by Medicare
CGMs are FDA-approved, physician-prescribed devices that detect and display blood-glucose levels continuously—and reveal trends in these levels that often go unnoticed. A JDRF-funded CGM trial has shown that the rate of severe high blood-sugar (hypoglycemia) events among adults using a CGM fell by two-thirds over the first year of use. Not surprisingly, CGMs are recommended by national diabetes clinical guidelines—and they’re covered by nearly all private health plans.
Unfortunately, Medicare does not currently cover CGMs—despite the evidence of clinical benefit. The result? Millions of seniors with diabetes are left vulnerable to severe low blood-sugar (hyperglycemia) events that can lead to seizures, bouts of unconsciousness and hospitalization. And the costs are not just physical:
- Hypoglycemia inpatient admission rates are an average of $17,564 per visit.
- Diabetes is one of the costliest chronic diseases, accounting for $245 billion in economic losses in 2012, including $176 billion in direct medical costs.
- Of that $176 billion, 59 percent is attributed to those ages 65 and older.
- Overall, 42 percent of Medicare fee-for-service spending is attributed to people with diabetes.
JDRF has been working closely with other interested stakeholders to encourage Medicare to cover CGM devices—and we have made it one of our top national advocacy priorities. While we continue to work to resolve this issue quickly, we need your help to build support within Congress.
Please take action today!
Remember, all you have to do is:
I see London, I see Florida, I see Arden's Dexcom CGM data
As our children get older our family is sometimes required to split up to accomplish everything on our calendar. You know, our son Cole my have a baseball game on one side of town while Arden has a game three towns over, stuff like that. Kelly and I never like to miss the kids stuff but it happens.
Last week presented us with a twist on that theme when Kelly's job took her to London the day before I was to leave for a Florida based college baseball recruiting weekend with Cole. Kelly left on Wednesday and was returning late on Friday night. I was leaving early Thursday morning and not returning until Sunday evening. Arden had school on Thursday, she was off Friday - okay, you following the set up? Kelly in London, Scott in Florida, one day of school and a day off to cover before Kelly returned home... what ever should we do?
My first inclination was to take Arden to Florida but that would mean her missing a day of school and to be honest, I didn't want to buy her a plane ticket and drag her from one hot baseball field to another, she would not have enjoyed the trip and I wouldn't enjoy spending the money.
Too expensive + too boring + too much school missed = Arden stays home.
The only person available to stay with Arden at our home was my mother and she knows exactly zero about managing type 1 diabetes, but did it matter that she didn't know anything about the day-to-day of type 1? Not if I can see Arden's BG on my phone it doesn't.
I thought about all that could 'go wrong' while I was gone and wondered if I could control the variables remotely, the possible issues that I could image were:
Could Go Wrong
- OmniPod insulin pump could need to be changed (Arden can do this on her own.)
- Dexcom sensor could need to be changed (Arden has never done this but without the Dexcom, none of this works.)
- Overnight (Arden wouldn't wake up overnight if a tugboat crashed into our house.)
- School (I can run school remotely as we normally do... as long as my plane had WiFi)
Plan for Could Go Wrong
- If a pod needs to be swapped Arden will do it but we don't keep insulin at school so I sent Arden to school on Thursday with pods and insulin and wrote to the nurse explaining what was going on. CHECK!
- Having a working Dexcom is the lynchpin to this entire plan and neither I or Kelly can come home if it stopped working. Arden has never changed a sensor by herself. Hmmm, wait... a boy in Cole's grade wears a Dexcom! I called his mother (who I know at best tangentially) and explained the situation. I told her that it was unlikely that Arden would let her try to put a sensor on her but asked if she could be there to oversee if necessary. She rocks and agreed to help if needed! CHECK!
- Overnight what I really needed was an adult to answer the phone and wake up Arden for me, my mom can handle that. CHECK!
- I booked a flight on an airline that has WiFi. Kelly was prepared in London to take over while I was in the air should I encountered a connection issue. CHECK!
Best laid plans and all, but how did it go in the real world?
During my flight
Everything worked out as planned. I woke up early for the plane, made Arden's lunch, counted carbs and packed up her pods and insulin. My mom woke Arden up in the morning, we texted while she was getting dressed to get her BG in place for the morning. The WiFi on the plane was great but we still maintained a multi-person text message thread so Kelly could watch what was happening from London and take over if I dropped out of the thread. We bolused once or twice while Arden was at school that morning, all from 35,000 feet.
I was on the ground for Arden's lunch time pre-bolus and on a ball field when it was time to talk about her pre-bus routine. My mom cooked dinner and I pre-boluses for it. On Friday I managed Arden's BGs and mealtime insulin from my phone while Cole made the catch you'll see below. Arden changed her OmniPod during a playdate late that afternoon without incident. Kelly returned to our house around midnight and took over the diabetes stuff. I slept that night like a baby.
My Take Away...
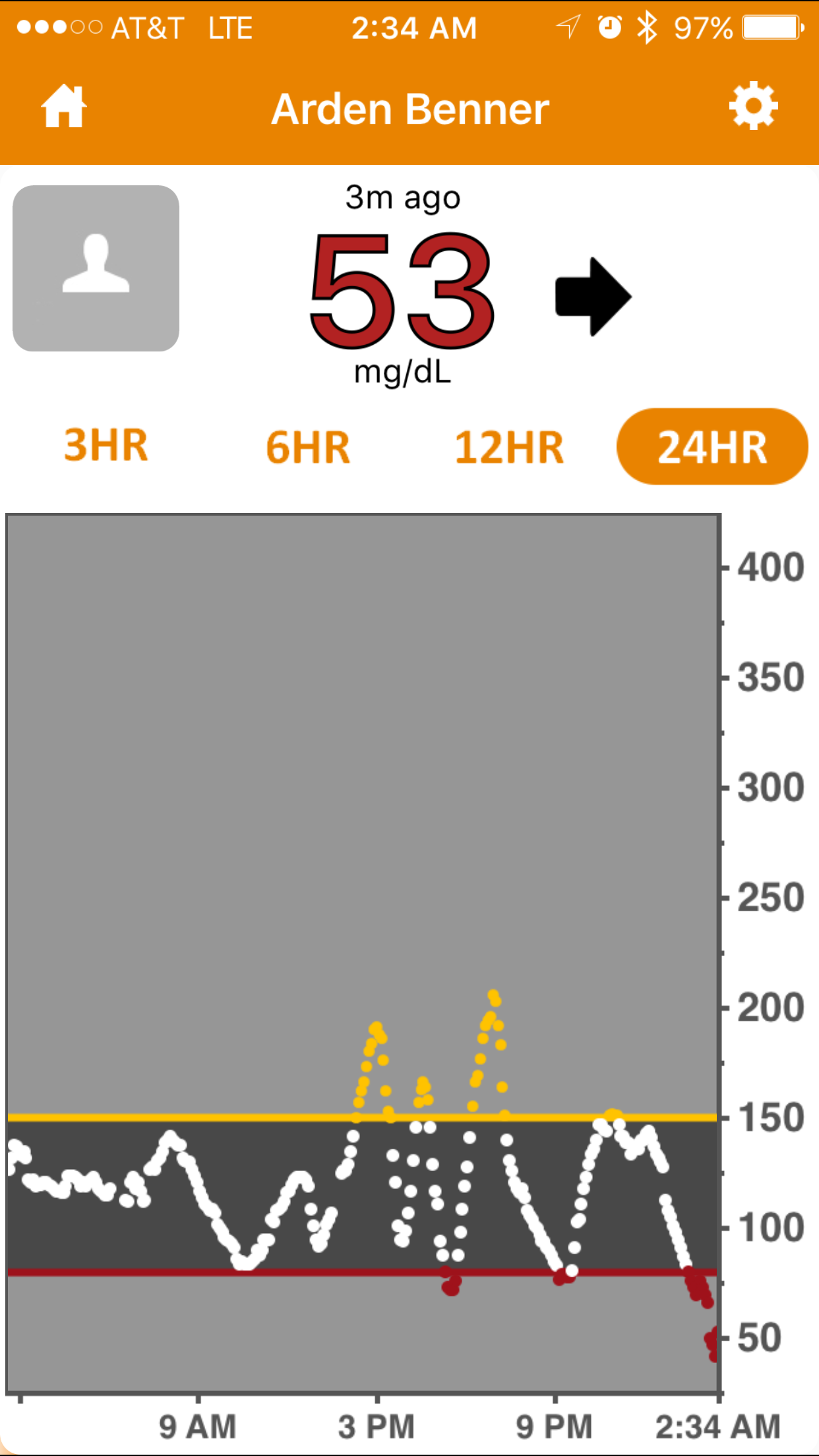
With a reasonable, but not heavy amount of pre-planning, we left our eleven year old daughter at home with a person who had almost no working knowledge of type 1 diabetes and everything was fine. Arden experienced a low BG (53 on Dex, 61 by finger stick) Thursday night around 2:30 am. My Dexcom Follow app alerted me, I called and woke up my mother who in turn woke up Arden and she drank juice as I instructed. I then waited up to make sure that the juice had the desired effect and when all was good about twenty minutes later, I went back to sleep confident that I would be alerted if something changed. In the twenty-four hour period that began at school and ended with that low, Arden's Bg was mostly stable, largely in range and only spiked to 200 twice. Two spikes and one low felt like a huge win to me.
Tomorrow night Arden goes to a sleepover at a friends house, no one in the home has the slightest idea about type 1. We will arrive ten minutes early to install the Dexcom Follow app on the mother's phone, I'll talk about how to handle emergencies and that'll be it.
Your Take Away...
Long run in centerfield. Cole saved a game while in Florida with this catch in the last inning of game 2.
I'm forever telling you that diabetes and fear do not have to go together and I wholeheartedly believe those words. Last week I put my money where my mouth is for two reasons. A. It was the right thing to do for my family and B. I wanted you to see that even in this completely odd and distant situation, things would work out.
I want to encourage you to take a chance too. Who knows, maybe you can move your life with diabetes a bit closer to where you want it to be.
I'll be talking more about this trip and other topics on next weeks episode (#34) of my podcast. If you haven't tried the Juicebox Podcast yet, it is available on this site, iTunes, Stitcher and everywhere else that podcasts are available. Subscribe today to be automatically notified when new episodes are online - It is 100% free.