Diabetes teaches, if we’re ready to learn
Guest post from Terry O’Rourke
Companion to episode 349 of the Juicebox Podcast
Thank you for clicking on this companion piece that accompanies my interview on The Juicebox Podcast. I realized soon after the interview that I left the listener with an incomplete view of me and my diabetes management philosophy. I hope this fills in missing information and corrects anything that may have left the wrong impression.
I’d like to take this opportunity to further describe who I am, my diabetes history, how I eat, my thoughts on doctors, what I’ve learned from my diabetes, my thoughts on the “your diabetes may vary” adage, and finally, automated insulin dosing.
Let me start by saying that I don’t consider myself special and my perspective is certainly not the only way to think about and manage diabetes. It is simply one way — a way that works for me.
My diabetes background
Norm is Terry's hypoglycemia alert service dog, companion and friend
I am a 66 year-old man who has lived with type 1 diabetes for 36+ years. While I consider my blood glucose management today as excellent, it has not always been this way, far from it. I wish I could say that when it comes to diabetes, that I’m a quick learner and I’ve avoided learning things the hard way.
In fact, I spent decades making almost every diabetes mistake one can make. I am human and still make diabetes mistakes every day. One thing diabetes teaches is humility!
It wasn’t until year-28 of my diabetes journey that I finally resolved to take comprehensive action and set out to gather the information I needed to pivot to a more effective and satisfying management style.
I’m sorry to admit that my current management style came about primarily due to the onset of secondary complications. A gastroparesis diagnosis found me in 2012 and coronary artery disease followed in 2018. Diabetes has scarred me and I used those set-backs to fuel my motivation and hopefully lessen the effect those complications might take on the remainder of my life. Writing about this journey and sharing my experience with the diabetes community is one of the things that brings meaning to my life.
Disclosure of my current management numbers is done with some trepidation. I am not here to brag and I know that reporting nearer-to- normal blood glucose levels with T1D can irritate some and intimidate others — I don’t intend that. I also know that managing T1D is hard and complex — not everyone can reproduce what I do with their unique situation and I understand that.
I don’t see any way around this disclosure dilemma, however. I want you to know that my tactics lead me to good glucose management and I don’t want to just paint my outcomes in an ambiguous way. So here goes.
I much prefer % time in range, % time hypo, glucose variability and average glucose as the definitive measures of my glucose management. I use a continuous glucose monitor or CGM data for these measures. My A1c number interests me but I don’t use it to provide essential feedback since I realize that it is inherently an average number that can hide unacceptable variability as well as glucose values too far out of range.
My time in range (65-130 mg/dL) is usually > 90% with time low (<65 mg/ dL) < 5%. Standard deviation serves as my stand-in for glucose variability and is often =< 20 mg/dL. My average glucose hovers between 92 and 102 mg/dL. Meeting these personal standards rewards me with a better quality of life sustained by more energy and clearer thinking.
Own your diabetes
Now that you know the metrics that steer my diabetes management, I want to share one philosophical point that guides me. The “own your diabetes” philosophy drives my diabetes management. Your doctor does not live with your diabetes. Neither does your spouse, friend, child, parent, teacher, coworker or boss. Your diabetes is your diabetes! It is unique to you and directly impacts the quality of your life.
Having said that, I see parents of children with diabetes as an exception to this philosophy. I consider parents of children with diabetes, especially young children, as close to diabetes as a person can be without actually being diabetic. I suspect the close and empathic bond that parents and children enjoy is what makes this possible.
If you’re new to diabetes, you may go through a phase of bargaining as you adjust to this daunting reality. That’s fine for some short time and it does serve as way to cope with the shock that a diabetes diagnosis can leave in its wake. But don’t let that bargaining turn into a chronic affair. Bargaining delays and can prevent diabetes ownership. It took me 28 years to learn this hard lesson; it needn’t take so long.
Diabetes is as much a part of you as your profile, smile, and the way you move. It’s inherent and inseparable from your nature.
By owning diabetes, you will give it what it requires at the time it requires it. In return, it can reward you with metabolic peace and inject your life with energy, optimism, and possibility.
I realize that the above statement is an ideal view of things and tempering with pragmatic choices will be necessary. But I think targeting optimal goals motivates better than shooting for tepid uninspiring goals.
Let me recognize here that my situation as a retired single man makes it easier for me than people in other circumstances. I realize that other demands like family and work responsibilities can make doing this tough, but I’m expressing an ideal here, one that hopefully can provide a sentiment to power stretching toward better, realistically conceding that perfect is impossible.
I realize that even diligently acting on this philosophy of owning your diabetes will not turn your life into a continuous series of rainbows and unicorns, but it can set the stage for happiness that gluco-normals take for granted.
Listen to Terry on the Juicebox Podcast - June 2020
Your eating style matters
Food choices are a sensitive topic for everyone, including non-diabetics. Very few people take pleasure in seriously considering a change to their eating habits. Considering a change in diet ranks right up there with changing your religion or politics. It’s not a popular topic of discussion.
I choose to limit carbohydrates in my diet. Carbohydrates are the main driver in the need for insulin to metabolize glucose. Fewer carbs means less insulin is needed and therefore means smaller dosing errors — Bernsteins’s law of small numbers.
Limiting carbs in my diet has allowed me to lose significant weight and move me from the overweight to normal weight category. I cut my total daily dose of insulin to less than half and my blood sugar control markedly improved.
I do believe that too much insulin often leads to negative long-term health consequences. For my first 28 years with diabetes, my main glucose management tactic involved deliberate overdosing for meals followed by strategic snacking later to avert imminent hypos. This led to slow yet consistent weight gain and some scary hypos when life distracted me from my strategic follow-on snack.
There are more ways to eat successfully with diabetes than the path I’ve chosen. My way is not the only way but it’s a way that works for me. Others may choose to eat a high-carb and low-fat diet and still maintain good glucose management. Sugar-surfers, for example, can eat many more carbs than me and by paying attention and responding in a timely way with dynamic insulin dosing can keep their glucose in a good range.
If you consider limiting carbs to help with your glucose control, personally experiment to discover which foods and how many carbs work for you. You may be able to consume more carbs than me and still keep your blood sugars in check. “Eat to your meter” is a viable and potent tactic.
Processed carbs, I believe, are bad for everyone’s health. If it has a long ingredient list and you don’t recognize some of the items, you should consider avoiding that food. A once-in-a-while treat or convenience is one thing, eating that treat everyday may harm you.
A low-carb, high-fat diet as well as a high-carb, low fat diet can both be made to work with good glucose control but the Standard American Diet (SAD) of high-carb and high-fat is often the source of obesity, metabolic syndrome, and overall poor metabolic and immune health.
As I said in the podcast, no food tastes as good as a normal in-range blood glucose level feels.
Listen to Terry’s first appearance on the Juicebox Podcast - March 2016
Your doctor is on your side, but not completely
While eating choices play a crucial role in our diabetes health, our doctors also influence our diabetes perspective. Most of us visit our doctors regularly. I’ve been seeing doctors for diabetes about four times per year for 36 years. For the most part, I view my doctor as an ally in my daily struggle with diabetes but I’ve learned that their agenda and values are not completely congruent with mine. And that’s OK - just realize that you are the ultimate authority about your health choices since you are the only one who will directly live with the outcomes of those choices.
It’s best to recognize this so that you can manage that divergence of interest and keep conflict from undermining important facets of the patient/doctor relationship.
Please accept that I speak in a general way about doctors and your experience with your doctor may be better than the personal observations I make here. I’m well aware that great doctor/patient relationships exist. I wish I had a better history with my diabetes doctors and I maintain hope that I may yet grow into one.
Let me start by saying that doctors are on our side. They chose their profession to help others - they’re usually in their job for the right reasons. They can help us manage our blood sugars and navigate the complexity that is T1D.
Their ability to take on the mundane task of keeping all our prescriptions straight is monumental. Pharmacy benefit managers can make their lives as frustrating as ours on that point.
The biggest concern I have with my diabetes docs is that they can be overly fearful of insulin. This distracted fear of hypoglycemia will usually provide guidance that nudges you towards higher overall blood sugar averages in the hope that you manage to stay well away from any hypoglycemia.
Now I realize why doctors see hypoglycemia in this way; severe hypoglycemia kills some of us every year. It is a tragedy and a fact that we should all keep in mind as we make management decisions.
But modern technology and newer management styles can allow many of us to maintain lower glycemia without undue hypoglycemia. Notice that I didn’t say “zero hypoglycemia.” I think that any T1D who manages to remain near normal glucose for a high percentage of time with low glucose variability will experience some hypoglycemia. It goes with the territory.
Doctors can often fail to distinguish between patients with swinging blood sugars and a low average and others with much smaller variability and a closer to normal average. It’s something they should be able to see with today’s CGM charts but many docs reflexively act fearful at the first sight of a normal A1c (< 5.7%) or average blood glucose.
They’re worried about legal exposure and moral responsibility; I get that. The fact that this mindset is more than willing to trade hypoglycemia for hyperglycemia and ultimately greater risk of long-term complications is what bothers me.
It eases the practitioners’ legal and moral fears at the expense of our long- term health — not an acceptable trade for me. I know this doctor mindset is defensible with their average patient but I think doctors should be able to detect patients like me and still support my management choices appropriately.
Doctors are our allies but their position is not fully aligned with ours, a reality with which we should not lose sight.
Be a student of your diabetes
A good doctor can teach you about some important aspects of diabetes but a much larger body of knowledge is available to you, free to observe and learn. I discovered that observing my diabetes CGM data on a daily basis provided me with a potent method to improve my metabolic health. I never took a formal course in statistics but watching my CGM data has taught me important things about my glucose management.
I currently wear a Dexcom G4 continuous glucose monitor (CGM) but will soon transition to the Dexcom G6 shortly before the G4 goes dark on June 30, 2020.
I track four measures every day, listed in order of importance to me:
1. Percent time in range
2. Percent time in hypoglycemia
3. Glucose variability with standard deviation (SD) as the proxy
4. Average blood glucose
Note that the A1c number is not one of these metrics. I find the A1c interesting but not useful in daily management. We all know that an A1c can hide unhealthy glucose variability and excessive time in both hypo and hyper territory.
I set my time in range (TIR) bounds at 65-130 mg/dL to make me stretch and do not simply accept the much less challenging standard (70-180 mg/ dL) set by clinicians and the American Diabetes Association. But that standard may be perfect for you if it causes you to reach for better. If, however, you’re achieving 90-100% TIR with the ADA standard then perhaps tightening that range may be something to consider.
I find that the mere observance of my diabetes data on a daily basis engages my brain at a sub-conscious level and usually leads to better daily choices and performance.
I see a dark side to YDMV
Observation of your diabetes data often leads to the inevitable comparison against some standard or other’s data. This is often where Your diabetes may vary or YDMV comes into play. YDMV captures a generally accepted truth within the diabetes online community. It seems obvious on its face. Since my body differs from yours, it makes sense that my metabolism differs from yours.
When I first became aware of this commonly accepted “truth,” there was something about it that bothered me. While we do differ from each other along perfectly explainable distinctions, like male versus female, child versus mature adult, baby versus teenager, we still share the essential fact that we are all human beings. Our common humanity provides a shared biology that should not be minimized or dismissed altogether.
Certain facts of type 1 diabetes are true across all humans. Insulin metabolizes glucose. Too much insulin causes hypoglycemia. Not enough insulin can lead to diabetic keto-acidosis. Blood glucose in T1D is primarily a function of eating, exercising, insulin dose size and timing.
But, I observe a dark side of the YDMV aesthetic that I don’t think serves us well. A large part of treating diabetes well is determined by both knowledge and attitude.
If, for example, you observe that after every breakfast your glucose rises to 240 mg/dL (15 mmol/L) and instead of reasonable alarm that drives you to change something to improve your post-breakfast glucose, you instead take refuge in the YDMV axiom, then it permits you to dismiss the importance of your observation that your after-breakfast glucose is too high. YDMV may grant you permission to think that a high glucose after breakfast is simply your unique variation from the diabetic norm.
I don’t object to embracing YDMV to explain differences between us. But that explanation has limits and we must check ourselves to make sure we don’t use it to relieve us of responsibility and action to correct an unhealthy trend. My diabetes may vary from others but we should ask ourselves a critical question. Why does my diabetes vary in a certain aspect from others? Is it because of an unchangeable part of me or could it be due to something within my control? Am I doing everything I might to alter some part of my diabetes management and make it better?
For example, instead of concluding that your biology just doesn’t permit reasonable post-meal excursion and writing to off as YDMV, you could for example, experiment with pre-bolusing and discover much better control.
YDMV is true in that it can explain natural variability from one T1D to the next. We should, however, be honest with ourselves and examine whether any variation from the norm is really beyond our ability to manage or maybe we’re undermining good management because we don’t really want to do the work. An honest assessment might let us see a favored habit that is not really serving us well.
Automated insulin dosing is awesome
Overall philosophies like YDMV and becoming a student of your diabetes can help in the larger context of managing diabetes but technical treatment breakthroughs like automated insulin dosing can directly enable a better quality of life. On November 14, 2016, I went live with Loop and couldn’t believe my good fortune! My blood sugar management was already pretty decent at the time but Loop accomplished several things for me. For one, it immediately lightened the cognitive burden that good management of T1D entails.
Overnight, while sleeping, it kept my blood glucose or BGs in a tighter and more normal range. Prior to that, the only tools I had to influence a nice in- range BG while sleeping was a well-calibrated overnight basal profile and the discipline to avoid evening snacking.
Loop shines in the overnight hours. It can analyze and make a dispassionate math-based decision every five minutes, something that I couldn’t do even if I was awake. It’s common for me to wake up from a night with zero CGM alarms and in-range at 70-99 mg/dL. This is a huge quality-of-life boost.
While Loop is still a hybrid closed loop system and requires manual interventions around meals, it supports these decisions with a sophisticated algorithm. Loop also relieves the burden I felt with managing meals and exercise. It didn’t make things perfect but it significantly lightened my load. Loop allows me to boost my time in range, cut time hypo, while it reduces glucose variability and average BG. It enables better numbers with less conscious effort from me, a win-win solution.
I learned that a good fundamental understanding and fluency of basal rates and insulin sensitivity settings enabled me to make adjustments when things changed, as they always do. I still had to pay attention but the minute-to-minute burden was now gone.
Loop is not the only automated do-it-yourself (DIY) insulin dosing system. Other DIY systems include Open APS and Android APS.
We are also witnessing the emergence of commercial hybrid closed loop systems. The Medtronic 670G was introduced in 2016 but its abilities are more limited than the existing DIY systems, yet many people are happy with its performance. Tandem, with its X2 pump has brought forth its Basal-IQ and Control-IQ software upgrades, both highly effective and popular.
In the years ahead we can look forward to other refinements in automated insulin dosing. The BetaBionics iLet system will eventually make possible delivery of both insulin and glucagon, giving hormonal control to prevent both hypos and hypers.
I strongly encourage people with diabetes to consider experimenting with these systems. The ability to share the cognitive load with a machine can bring relief from this ceaseless burden.
I hope that sharing some about me and my diabetes history, how I eat, manage the doctor relationship, learn from my diabetes, a pitfall of YDMV, and automated insulin dosing systems may be useful to a few here. If you’ve made it to the end, I am humbled. I’ve learned much from my peers in the diabetes online community and I find it meaningful to pay forward what I’ve learned.
I see London, I see Florida, I see Arden's Dexcom CGM data
As our children get older our family is sometimes required to split up to accomplish everything on our calendar. You know, our son Cole my have a baseball game on one side of town while Arden has a game three towns over, stuff like that. Kelly and I never like to miss the kids stuff but it happens.
Last week presented us with a twist on that theme when Kelly's job took her to London the day before I was to leave for a Florida based college baseball recruiting weekend with Cole. Kelly left on Wednesday and was returning late on Friday night. I was leaving early Thursday morning and not returning until Sunday evening. Arden had school on Thursday, she was off Friday - okay, you following the set up? Kelly in London, Scott in Florida, one day of school and a day off to cover before Kelly returned home... what ever should we do?
My first inclination was to take Arden to Florida but that would mean her missing a day of school and to be honest, I didn't want to buy her a plane ticket and drag her from one hot baseball field to another, she would not have enjoyed the trip and I wouldn't enjoy spending the money.
Too expensive + too boring + too much school missed = Arden stays home.
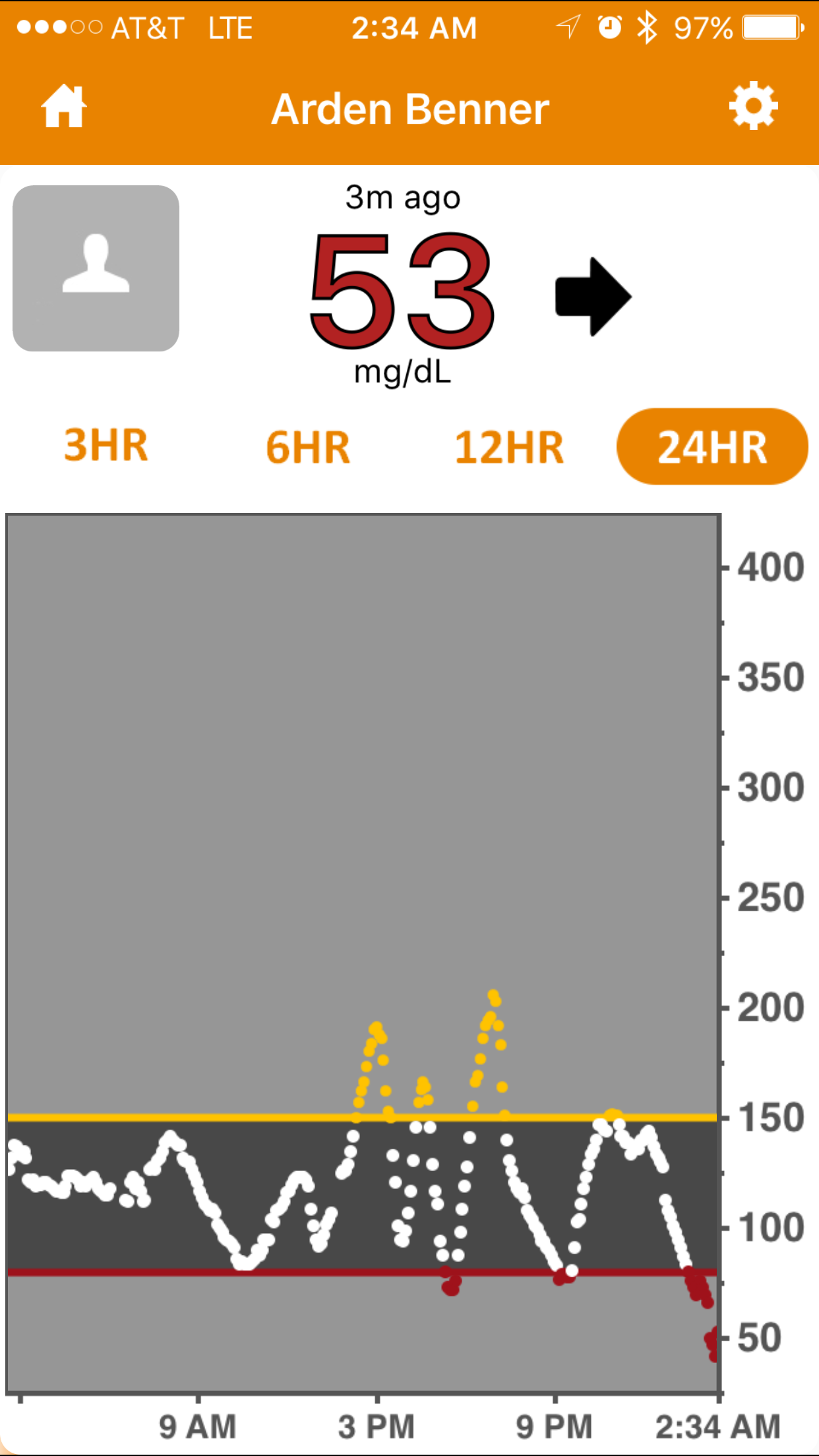
The only person available to stay with Arden at our home was my mother and she knows exactly zero about managing type 1 diabetes, but did it matter that she didn't know anything about the day-to-day of type 1? Not if I can see Arden's BG on my phone it doesn't.
I thought about all that could 'go wrong' while I was gone and wondered if I could control the variables remotely, the possible issues that I could image were:
Could Go Wrong
- OmniPod insulin pump could need to be changed (Arden can do this on her own.)
- Dexcom sensor could need to be changed (Arden has never done this but without the Dexcom, none of this works.)
- Overnight (Arden wouldn't wake up overnight if a tugboat crashed into our house.)
- School (I can run school remotely as we normally do... as long as my plane had WiFi)
Plan for Could Go Wrong
- If a pod needs to be swapped Arden will do it but we don't keep insulin at school so I sent Arden to school on Thursday with pods and insulin and wrote to the nurse explaining what was going on. CHECK!
- Having a working Dexcom is the lynchpin to this entire plan and neither I or Kelly can come home if it stopped working. Arden has never changed a sensor by herself. Hmmm, wait... a boy in Cole's grade wears a Dexcom! I called his mother (who I know at best tangentially) and explained the situation. I told her that it was unlikely that Arden would let her try to put a sensor on her but asked if she could be there to oversee if necessary. She rocks and agreed to help if needed! CHECK!
- Overnight what I really needed was an adult to answer the phone and wake up Arden for me, my mom can handle that. CHECK!
- I booked a flight on an airline that has WiFi. Kelly was prepared in London to take over while I was in the air should I encountered a connection issue. CHECK!
Best laid plans and all, but how did it go in the real world?
During my flight
Everything worked out as planned. I woke up early for the plane, made Arden's lunch, counted carbs and packed up her pods and insulin. My mom woke Arden up in the morning, we texted while she was getting dressed to get her BG in place for the morning. The WiFi on the plane was great but we still maintained a multi-person text message thread so Kelly could watch what was happening from London and take over if I dropped out of the thread. We bolused once or twice while Arden was at school that morning, all from 35,000 feet.
I was on the ground for Arden's lunch time pre-bolus and on a ball field when it was time to talk about her pre-bus routine. My mom cooked dinner and I pre-boluses for it. On Friday I managed Arden's BGs and mealtime insulin from my phone while Cole made the catch you'll see below. Arden changed her OmniPod during a playdate late that afternoon without incident. Kelly returned to our house around midnight and took over the diabetes stuff. I slept that night like a baby.
My Take Away...
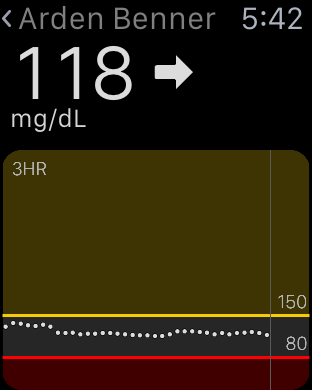
With a reasonable, but not heavy amount of pre-planning, we left our eleven year old daughter at home with a person who had almost no working knowledge of type 1 diabetes and everything was fine. Arden experienced a low BG (53 on Dex, 61 by finger stick) Thursday night around 2:30 am. My Dexcom Follow app alerted me, I called and woke up my mother who in turn woke up Arden and she drank juice as I instructed. I then waited up to make sure that the juice had the desired effect and when all was good about twenty minutes later, I went back to sleep confident that I would be alerted if something changed. In the twenty-four hour period that began at school and ended with that low, Arden's Bg was mostly stable, largely in range and only spiked to 200 twice. Two spikes and one low felt like a huge win to me.
Tomorrow night Arden goes to a sleepover at a friends house, no one in the home has the slightest idea about type 1. We will arrive ten minutes early to install the Dexcom Follow app on the mother's phone, I'll talk about how to handle emergencies and that'll be it.
Your Take Away...
Long run in centerfield. Cole saved a game while in Florida with this catch in the last inning of game 2.
I'm forever telling you that diabetes and fear do not have to go together and I wholeheartedly believe those words. Last week I put my money where my mouth is for two reasons. A. It was the right thing to do for my family and B. I wanted you to see that even in this completely odd and distant situation, things would work out.
I want to encourage you to take a chance too. Who knows, maybe you can move your life with diabetes a bit closer to where you want it to be.
I'll be talking more about this trip and other topics on next weeks episode (#34) of my podcast. If you haven't tried the Juicebox Podcast yet, it is available on this site, iTunes, Stitcher and everywhere else that podcasts are available. Subscribe today to be automatically notified when new episodes are online - It is 100% free.
Will Hauver
I would like to thank Lydall Hauver for her courage and for her desire to support the diabetes community. It speaks to the strength of our community that in the wake of what is undoubtably Lyndall's greatest personal tragedy, she would allow herself to be interviewed. I can promise you that if you have type 1 diabetes or love someone that does, this post and the podcast episode of my conversation with Lyndall will ultimately fill your heart with love, hope and a sincere desire to live well with type 1. So grab a tissue, read Lyndall's post and then listen to me chat with her and Will's good friend Paige, about his life and legacy. - My best, Scott
The tragic and devastating death of our son Will, a beautiful person on the inside, and a good-looking man on the outside, has taught me something very valuable.
One person has the ability to make a positive and significant impact on this world.
It has been made clear to our family that Will made a huge impact on many people in his 22 years. The quality of Will’s life, and what he did with those 22 years was incredible. Wherever he went, he made an impact. We have heard over and over again about how Will’s compassion, his way of including everyone, his friendship, ‘saved’ many a friend from transferring from college, from quitting a team, from not joining in a great event. Will had such a handle on the ‘big picture’ - what was important in life. He was often sought out by his friends for advice and help. Using his humor he could really relate his advice without being preachy and condescending. He had such an easy, approachable, welcoming way about him, with the confidence that others admired and respected.
One person has the ability to make a positive and significant impact on this world.
“It is not length of life, but depth of life.”
This past summer Will was nominated to complete the ice bucket challenge for ALS awareness and donations. While donating $48.25 to an ALS charity (to an ALS charity Brigance Brigade) he filmed a video, which is very funny, and created a challenge for the JDRF and “LIVEabetes”. After Will passed away, his good friend from high school, Paige, one person, galvanized behind this comic but meaningful video, and created a movement to raise funds for the JDRF. Through a lot of hard work, a lot of learning about different social media options and a lot of creativity, Paige created a great group of supporters, myself, and my family included, to create a worldwide challenge raising awareness and money for type 1 diabetes. Incredibly, to date, we have raised over $80,000 for the JDRF to fund a cure for this dreadful disease.
Paige and Will, two young people, have made such an impact on this world, simply by being good people. They chose to live their lives by these simple principles: be kind to others, be inclusive, help others, know who you are and do not compromise your morals to fit in and make deep and meaningful connections with people you encounter. After Will’s death people from around the world rallied behind the man he was, to support the Egg Crack Challenge Paige worked hard to promote and grow. We now have an amazing community of friends, new and old, who have banded together to raise awareness and funds for a cure for type 1 diabetes.
One person has the ability to make a positive and significant impact on this world.
Our daughter Megan and Tommy are like Will and Paige, two people who have a keen sense of self, who stay true to that self. Similar to Paige they have worked hard to promote the Egg Crack Challenge. Additionally they have created T-shirts, posters and other item to share the joy Will created as an artist to raise money for type 1 diabetes and for scholarships in Will’s name.
Will told his girlfriend weeks before his death, “Each day is a gift, that is why they call it the present.” His ability to use humor, and kindness to live each day to the fullest, to make an impact on each person he encountered, has rubbed off on me, and on our entire family. This attitude is why we get up each day and try to salvage what we can out of each day, no matter how hard and how sad we may feel. Knowing that one person has the ability to make a positive and huge impact on this world makes me move forward to create my own positive, impact, each day.
- Lyndall Hauver, Will's Mother
You can listen to my conversation with Lyndall and Paige with the player below, on Juicebox Podcast, iTunes, Stitcher or your favorite podcast app.
links you need:
Will's JDRF Donation Page
Egg Crack on Facebook
Will's Egg Crack Video on YouTube
Rollins College Memorial Service for Will
Egg Crack Homepage
Shop for gear and bracelets (Supports JDRF and scholorships)
Dealing with a Severe Adhesive Allergy
That’s Not Just Contact Dermatitis
This is a guest post from a D-mom named Rachel Morgan who was a recent guest on my podcast. At one point we spoke about her son Henry's severe adhesive allergy and I asked her if she would be interested in contributing a blog post on the subject. I think you'll agree that Henry's situation was dire and that his mother's insistence on finding an answer that would allow him to continue to use his diabetes technology, is nothing short of impressive.
Henry's back. Click to enlarge
Living with diabetes means you get gut punched several times a week, whether it’s a bad low, an out of control birthday party complete with grocery store cup cakes, chips, soda, and pizza, or simply watching your sleeping child hold out his finger for a 2 am BG check. Our three year old son, Henry, was diagnosed in March of 2014 and by late May he was on an Animas pump and Dexcom. With these tools in place, we felt some of the control diabetes had devoured starting to return. We could see what a long car ride did to Henry’s blood sugar, so we increased his basal by 30% and had perfect numbers on a 15 hour car ride. Double arrows down caught a scary low of 48 on a hot August day at the zoo. Then all the sudden, we were double and triple gut punched in October of 2014 when this happened.
Within 48 hours the reaction became systemic. Click to enlarge
Henry developed a tape and adhesive allergy and within 48 hours the reaction became systemic.
Click to enlarge
Type 1 is an autoimmune disease, and Henry also developed a severe tape and adhesive allergy. His primary care physician and Endo were worried about anaphylactic shock; he was given oral steroids (hello, high blood sugars!) and a horse load of Benadryl, and we were told to stop using devices with adhesive and go back to multiple daily injections (MDI). We took the Dexcom off but we wanted Henry to stay on the pump for the benefit of his long term health. I became that mom. I scoured the internet and made an insanely detailed power point, which I sent to every medical professional who would listen. I researched colostomy care because I felt we were really dealing with skin breakdowns and wound care.
I found a CDE through Children with Diabetes who lectures on tape and adhesive allergies, and she called me back that night, and a few days later some of her personal T1D supplies showed up in our mailbox, and with a few more phone calls, research, and a little trial and error, here’s what we do to prepare a pump site.
Click to enlarge
- Wash area with warm water and antibacterial soap— Do not use alcohol
- Completely dry the area
- Apply one puff of Flonase (sweet-talking or demanding this prescription from Endo or PCP is necessary)
- Apply thin layer of Cavilon barrier cream (Amazon)
- Apply a 6cm X 7cm layer or Tegaderm HP 9534HP (NOT Tegaderm!!) Check with your pump supplier— some insurances cover this and it’s shipped with pump supplies. You can also purchase Tegaderm HP from Amazon.
- Place inset through Tegaderm HP
- We place another layer of Tegaderm on top to secure the pump site and provide an extra layer or barrier for the adhesive of the detach inset
- When wet, blow dry site with hair-dyer on a cool setting
- Apply prescription Hydrocortisone after removing the Tegaderm HP and old site
- Remove any extra adhesive from the old site at bath time with calendula oil
A rashless, T1D strong Henry today!
The wounds eventually healed after six months. I’ve heard some people describe these wounds as burns, and the skin damage is extensive. Henry’s skin is finally healed, and we’re about to try Dexcom again, using the above preparation method, but with a hydrocolloid barrier, like Johnson & Johnson Tough Pads, sandwiched between the layers of Tegaderm HP. I’ve read about people successfully using Duoderm and blue tape, a kind of baby tape used in NICU’s, as a barrier and adhesive method, but we have yet to try these products.
Being a T1D parent is really difficult, so I’ve learned to find joy in the small victories, like staying on a pump. We’re taking it one number at a time and moving forward.
You can listen to my conversation with Rachel right here in this post, on iTunes, Stitcher, at JuiceboxPodcast.com or with your favorite podcast app.
The insulin bottles pictured in the header of this blog post are from the first eight months of Henry's life with type 1. Rachel knitted a heart for each... If you have questions about the process Rachel described in this post, you can contact her here.
2014 Year in Review
It's December 31st and I've been spending a lot of time recently thinking about how to make Arden's Day better for you. As we head into the eighth year of my little blog's life I'm looking at ways to make the blog more informative, social, easy to consume and worth coming back to. In the process I've been reading a lot of old post from 2014 and found a few that are worth revisiting before the ball drops. I hope you read to the end of this long post, I'd like to share something very personal to me before the calendar flips.
From January 2014
It baffles me, but one of the most popular things on the blog this year was a photo of me looking tired, How to Spot a D-Parent. It was even reposted on Diabetes Daily and become one of their most popular post of the year. Of all the things I wrote, shared and talked about this year, you liked seeing me looking ragged the best. Tells me we are all pretty damn tired.
From February 2014
Dexcom was approved for pediatric use, one of my non D storIes blew up on Huffington Post and Miss Manners was all the buzz but all you guys wanted to see was pictures of Kris Freeman's abs. Parents still read this post every day when they wonder if their child is too lean for pumps and a CGM. Kris's abs turned out to be quite the public service.
From March 2014
My blog titled, Pitstop Fail won Best of Betes Blogs for March - a huge thank you to the person who nominated it and voted!
From April 2014
A Forgotten Wallet Buys a BG of 25 and I got yelled at a little bit in the comments. BTW, Kris Freeman could have easily been mentioned here too, you guys sure love abs.
From May 2014
I changed my expectations for what 'in range' means and lowered Arden's a1c, Living Between the (Diabetes) Lines.
From June 2014
June brought the lowest A1c Arden has gotten to date, A1c Countdown: It's Endo Time.
From July 2014
This was the month of #ShowMeYourPump but Arden's Day readers were more interested (By just a few hits) in Arden's Sudden Needle Anxiety.
From August 2014
In August I tried with all my blogging might to get you to believe that Diabetes and Fear don't have to go together, Guts over Fear was written, the hashtag #DiabetesandFear was tweeted and my quest was underway.
From September 2014
I traveled to the Dominican Republic to deliver a speech to a group of D parents during the summer but wasn't able to share the video of my talk until September. My time in the D.R. led to a very popular post, my first invitation to give a keynote at a JDRF event (Info coming soon) and a whole lot of new understanding about the rest of the world.
From October 2014
Hello Dexcom SHARE you are the remote monitoring I've been waiting for.
From November 2014
Arden changed her first OmniPod without any help from me while she was at a sleepover, I'll Take Insulin Pump Change for the Win Alex.
From December 2014
I shared our experience with getting an insulin pump in the hopes that it would give you the freedom to speak your mind because, Don't Let Doctors Push a Pump on You, that's why.
I can't thank you enough for reading about Arden's day. I hope you have time to check out one more post from 2014, it's one I wrote today about what diabetes blogging means to me, you can find it here. Have a happy, healthy 2015... you are all in my thoughts. Best, Scott