# 385 Gvoke HypoPen
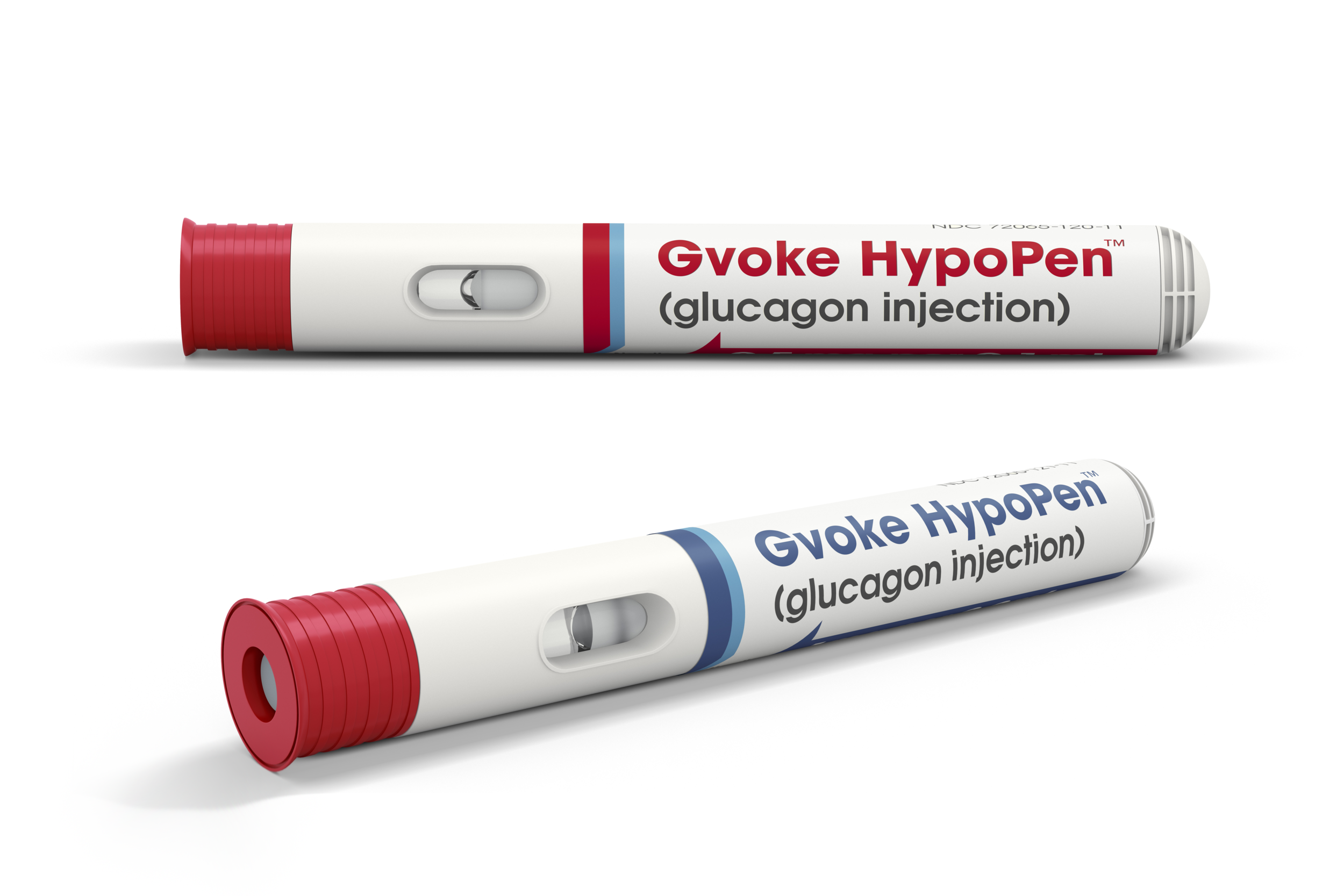
Gvoke is a premixed, prefilled, premeasured liquid glucagon that now comes in a HypoPen!
Ken Johnson is Senior Vice President, Clinical Development, Regulatory, Quality Assurance & Medical Affairs at Xeris. Ken is here to talk about the Gvoke HypoPen. Xeris makes Gvoke. The premixed, prefilled, premeasured liquid glucagon for treatment of very low blood sugar in adults and kids with type 1 diabetes ages two and above.
Jenny Smith is also here to help me answer questions about glucagon.
Learn more about Gvoke here
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott (1s): This episode of the Juicebox podcast is brought to you by GE Voke. The world's only liquid stable Glucagon G Volk is available in our, a prefilled syringe and in an incredibly convenient to carry it an easy to use HypoPen. As a matter of fact, I have a trainer of the HypoPen right here. Let me show you how easy does to use cap comes off. I find some skin press down
1 (28s): And it's done that.
Scott (30s): Yeah. Easy to administer glucagon. It's the easiest thing I've ever seen when it comes to Glucagon hands down. We're going to talk all about it today. How the G vote Glucagon came to be or what it is, and this brand new HypoPen, which is incredibly convenient to carry. And as you just heard, super simple to administer, anybody could do this in my opinion, before I start the show, let me say thank you. Because every question and this episode came directly from listeners to the podcast. So I really appreciate the effort and the thought that you guys put into those questions. And I hope you get your answers. I think you're going to today's episode is going to be a little different than most I'm interviewing to people today about Jeeva Glucagon first.
Scott (1m 16s): I'm not even first. Now here's the surprise. Let me just give you the surprise. Jenny is on this episode. Jenny Smith is here and I'm also speaking with Ken Johnson. Now Ken is a senior vice president of Clinical. Wow. This is quite a title at here. Ken Senior vice president Clinical Development Regulatory Quality Assurance that? Medical Affairs at Xeris pharmaceutical's Xeris makes Gvoke. Ken's got to answer all of your questions and Jenny is going to answer something to me.
1 (1m 45s): You guys,
Scott (1m 46s): You love Jenny. I love Johnny. How can we not love Jenny that's who else are you going to love? Ken Ken who buy the way has the secret talent. The man could play the piano, but not have to wait all the way to the end, to find out about that. Please remember that Nothing you hear on the Juicebox Podcast should be considered advice Medical or otherwise always consult a physician before making any changes to your health care plan or becoming Bold with Insulin
Scott (2m 38s): And there are two ways that you can request it through your doctor, either online or in person. If you have commercial insurance, you can request a prescription for Gvoke HypoPen right from the comfort of your home and have it delivered to your door fulfilled through PillPack by Amazon pharmacy. Just go to
Scott (3m 19s): We're going to start with Jenny Smith and then do a little Ken and then back too, a little Jenn. And Ken you got to get a nice rhythm going a little Jenny a little Ken is going to go just like that. I think you're going to enjoy it at the risk of repeating myself, because I say it in the episode, this is a leap for people who use Insulin making Glucagon liquid stable. It just This. If you don't understand why listen closely Jenny I already talked to Ken Johnson from Xeris pharmaceuticals about the Gvoke Glucagon and he's gonna be on the Show.
Scott (4m 7s): And just a minute, we talked a little bit just about what they were, you know, what they're trying to accomplish. I told him if the end of our conversation, that I'm incredibly excited about that company, like the ability to stabilize Glucagon in a liquid form, I think has other far reaching possibilities that I'm really excited about. But while I was talking to him, I got a it's a it's a, and can you tell if you can see this or not, but it's called their HypoPen and this is just a trainer, so it's not, it's not real, but you just pop off the cap and go like this and that's it. And it's over yet. And I was like, huh, well, that seems simple.
Scott (4m 47s): And I'm going to get one of those for Arden
Jenny Smith, CDE (4m 50s): Beyond simple. It's not scary
Scott (4m 52s): Exactly. Because you know, till this point in my life with type one, diabetes, glucagon has been a little bit of an, a, like a science experiment, but it was going to be an in a pressure situation. It's almost like someone saying to you here, do this while your driving a car, and there's a bear in the backseat, you know, you kind of felt like that to me the whole time. And, and they have their pre, they have their premixed syringes for emergencies to, which is just, you know, it's you just, it's in and push and you're done right yet. But, but still, and I'm, I'm going to ask you first, before I tell you what we do.
Scott (5m 35s): Do you carry Glucagon with you when you leave the house?
Jenny Smith, CDE (5m 40s): I don't carry Glucagon with me. If I'm just leaving the house for like going to the grocery store or going across the street to the park. No, don't I absolutely don't when we leave to go on even like a short weekend, two are in-laws or I go on, you know, to speak somewhere and whatnot. Yes. I, it with me now in that same case, though, if I'm carrying it with me in my pocket at a conference, somebody got to know what's in my pocket.
Scott (6m 9s): There's a lady on the floor. Hey, there's a science kit in your pants. What do you think? That's? What should we do? Where in the same boat, we don't carry it around like that either. If we're going to go too far away, or if it's going to be, if you're going to do at the beach or a trip, it comes with us. So here's my question. Would you carry this with you?
Jenny Smith, CDE (6m 28s): I would, because one, that's really easy to keep in my purse. And I mean, I've also, you know, knowing that I've got a son who'll be in second grade or something like this are easier to carry, I think, and from the standpoint of even teaching him visibly, there's no needle. I can easily say, Hey, pull this cap off, you know, stick it in my thigh, push it until it turns red and it clicks and it's done. I mean, that's it.
Scott (6m 58s): And it has these audio responses. I don't know if you can here the sec. So there's too, there's the push. And then the second one tells you your done. And I was like, huh, this I would put in Arden's bag. Like I really would. It's not going to scare somebody. And not only that, but if somebody opened this up a person who had no idea what they were doing, it's going to, you know, the packaging tells you what to do. And there's nothing about what I said to Ken when I was talking to him was I took this out of the mail, this trainer, and I handed it to my wife. And I said, I don't wanna tell you anything about it. See if you can make it work. And she did it right away, but it didn't take any like thought to do it's easy.
Ken Johnson (7m 39s): Hey Scott, this is Ken Johnson I'm with zeros pharmaceuticals. And I have a number of responsibilities that the company, including how we develop our drugs in the clinic and get them approved by the FDA. We also have medical team that supports ah, people with diabetes. And there are clinicians in the marketplace. And I also have a quality assurance team that makes sure that the drug's as we make them package them and ship them to pharmacy's and ultimately people and their homes meet the higher quality standards required for a prescription product. So all of those combined have been my responsibility at Xeris pharmaceuticals. For the past three years, I've been in this type of role for pharmaceutical development for a better part of 25 years.
Ken Johnson (8m 25s): I started out, I was trained as a pharmacist. I did research at the university of Colorado, whereas also involved in clinical research as a result of that clinical research. And I found my way into the pharmaceutical industry sector and had been there ever since. So that's a little bit about me. I'm I'm in Chicago where our headquarters are based and really happy to be with you today.
Scott (8m 47s): Thank you very much for doing this. I have a question about how you pull a team together for something like this. Does Paul know of you and com for you, or how does that work? Like how do you end up at Xeris?
Ken Johnson (9m 1s): Great question. So Polytech, our CEO, as someone who I met at the early part of my career. So 20 plus years ago, we were at a company based in Chicago called Searle pharmaceuticals. Paul was in charge of a number of commercial activities there and ultimately taking over some of the regional activities around the world, ah, for a number of our products. And I was his medical support. So a, you know, these things start early and have sort of an indelible effect. If these partnerships work and these collaborations work, you sort of maintain these relationships throughout your professional arc. We haven't always worked together, but oftentimes we'd been together out a couple other companies since that time. And most recently is he took the home at Cirrus who wanted to bring it together.
Ken Johnson (9m 44s): A group of folks that you felt could take us to the next level, get Gvoke HypoPen to market. And with that, he found me as well, a few others, we had this collective past together. So it's a little bit analogous to getting the band back together again. And we've, we've done that. And because of our past a familiarity success together, a what I think is an ease of collaboration, we do enjoy working together and I'm sure I'll do it again someday. Yeah.
Scott (10m 13s): How do you feel like The from the starting point to where you guys are right now, do you feel like that was on schedule went quicker than you anticipated? How much of that has to do with the, the, the, the, you know, the G Voke itself and how well it does, what it's, you know, what you're trying to, what you're trying to do.
Ken Johnson (10m 34s): Yeah. I think we encountered a situation where things were a little bit stalled or, or there's a few things that we had to take heat of that had been discovered before we arrived to make sure that we had, you know, a product that could meet all of the standards of the FDA. You could pass all the Clinical assessments. And so it really good foundation Scott, but it needed them and sort of to be rebooted to use that term it, and that meant conducting additional clinical studies further characterizing the product, making sure that we could put it into a prefilled syringe that's RPFs configuration or the HypoPen in the auto injector that was just released earlier this month. Right.
Ken Johnson (11m 15s): So that whole process of building, making testing, and then releasing brought together the team that you see today, you know, in fairness, there were about 12, 15 people at zero S when Paul took over and, you know, it's taken a lot of resources, people energy now in 200 plus employees later, you know, were on market with an approved product.
Scott (11m 40s): And for me to be sitting here holding this, this trainer pen, I guess it's a, it's a long time to get this into, get to this form and make sure it does what it says. So I think I want to understand what does it do because you've obviously come into a space where everyone has that red box and they genuinely think of it as something, you know, that they just have. They don't think much about it. I've been in that situation. My whole life. I get my daughter supplies, my daughter's supplies show up. They're there. I watch it until the expiration date and then I throw it away and I get another one. And I don't know that it's something that many people think about other than I know in the case of an emergency, you know, I've got this liquid in this powder and the syringe, and I'm supposed to mix them together and redraw them and use them.
Scott (12m 28s): And here's how, and ya know, and that kind of thing. And I have to train my school nurse to do it and, you know, My and her, grandma's got to know. So when she comes over, that's, that's, that's the narrative around that my whole life and for, for many, many people. So how do you improve on what's been going on for so long? Like what makes you feel like this is a great business and we should be doing that?
Ken Johnson (12m 52s): Well, I think, you know, just listening to your story and kind of the anxiety and complications that come with administering Glucagon for many, many years now, you know, going on in several decades of having the same configuration, it is a important pancreatic hormone Glucagon has very well known affects in terms of its ability to raise blood sugar. I think, you know, most days we're concerned about lowering blood sugar and insulin is critical, but, you know, think of this as the, the, the break where the accelerator, the, no, that the challenge is always been, it's a powder that requires reconstitution or, or, or put into a solution immediately at a time of use.
Ken Johnson (13m 37s): You can't do it early because it starts to break down very quickly. Most of the potency has lost or within 24 hours after mixing the powder for all these decades, that red box that you describe has been the single and only configuration available to people with diabetes are folks who would experience very low blood sugar. So our chief scientific officer took that on as a mission, you know, had his own personal experience and people in his life who said, you know, is it possible to overcome all those complicating, a multistep requirements of the lateralized Poudre in that vile? And he said, yeah, I think I can fix that. So it was his mission to make it a liquid, ready to use room, temperature, stable product, and to do that, we had to overcome the limitations of water and water is what you would use in the traditional kids to make it as a solution.
Ken Johnson (14m 29s): So we've taken water and replaced it with other a well known a solutions. Ours is called
Ken Johnson (15m 24s): And so you have basically a, a built in system to raise your blood glucose. And as such, we, you know, we wanted to just make the process of administering very approachable, very intuitive and not intimidating. And so we think we've accomplished that, but that was all only facilitated once we had a liquid version.
Scott (15m 44s): All right. After someone uses Gvoke what happens after is, are there side effects or are there things that happen afterwards? Am I going to feel nauseous? Do I have to go to the hospital? That's also, what's your dog's name, Bailey like that?
Ken Johnson (16m 0s): The question is, so I guess, I guess we'll have to give her a credit today. So a couple of things, I mean, you know, the effect that you do want is to raise a blood glucose, and that happens very quickly as we start to see changes in the blood glucose concentration within the first five minutes of administering the product is raised to what we consider a safe level of blood glucose very quickly on average, about 14, 15 minutes. And then the duration of action is probably about 90 minutes or so. So you have this ability to sort of bring yourself back up and then have it come back down, right? So it's a, it's a temporary fix two. What was a scary as hell? What can happen?
Ken Johnson (16m 40s): Glucagon has some other effects has some effects directly on the gastrointestinal tract. And so it at about 30% of the subjects that are trials has some nausea and about 10% handsome vomiting. So those are 10 or 15%, and those are kind of the hallmark features of what Glucagon does not matter what too, to anyone that sensitive to those GI side effects, importantly, they are transient. They are mild 80% of the people in our study and characterize them as mild. They went away and in our case, no one actually stopped being in our study because they had that, that known side effect that you would see that Scott with the old movie got, and you would see it with our Glucagon a you'll see it with future Glucagon so that we haven't mitigated.
Ken Johnson (17m 30s): It's probably dose-related. I think, you know, there will be a Day I hope someday where if we, you know, use different doses for different purposes, that we can mitigate some of that nausea, vomiting, but for the rescue one milligram setting of use your gonna have, in some cases, nausea and vomiting, then those side effects are
Scott (17m 50s): Side effects of Glucagon do not have a specific brand. It's just what happens during the process of bringing that low blood sugar up so quickly through Glucagon.
Ken Johnson (18m 0s): Yeah. And it may not even be read to get your rights. That's, that's the correct way to describe it in event, not even be related to the blood glucose, going back up as much as it is. There is a known, in fact that Glucagon to slow down the action of your GI tract so much. So that is completely different from what we're talking about today, but a radiologist will actually use this drug to stop someone's GI tract from moving, if they need to do procedures and other things. So now this is one of those situations where a bad thing for some person is a good thing for another, but it is important to let people know that there is some mild nausea in about 30% of people who use it for, for rescue.
Scott (18m 41s): Can you help me understand the different ways that I can administer as you vote when, you know, when you guys first came out and I became aware of You, my daughter switched too it, and she has the, the prefilled syringe, but now I'm holding. Like I said, This this dummy pen. That to me feels like I'm like what people would consider an epi pen and to be, I, I, I just push it down on my leg and hold it there for a second and, or a couple of seconds in, and I pulled away. Why do you have different versions? And can you tell me the difference between them?
Ken Johnson (19m 16s): Sure. The Glucagon it's the same for both a Gvoke PFS are people terrains in G Voke, HypoPen in the auto injector, you're holding a, in your hand. And so there's no difference. And that the active ingredient, the solution, the concentration is identical. It was a simpler and more straightforward manufacturing process to come to market with the prefilled syringe. It's less mechanical requirements because you, as a person, are the person helping you is actually going to do the injection much like you would self-inject or Jeff Insulin. Right? So it's a small subcutaneous injection, the necessary requirements to then put that into a device that fires itself, the auto injector, umm, it's more complicated, more engineering.
Ken Johnson (20m 7s): And we wanted to make sure we had sufficient quantity. So we come to market like we did the Smith and not having a sense of shortages or, or, or running out to be able to supply to market adequately. So, umm, there's a really, really high specification for performance of that auto injector because you're no longer responsible for pressing the plunger and the mechanics inside the auto injector. Our and so the FDA has carefully scrutinized the performance of this device and it has to work 99.99, 9% of the time. So that's a manufacturing spec and it came out of the experience that we've all had with epinephrin and HypoPen we want to make darn sure that if someone's going to pull that red cap off and press that yellow plunger, that if a fire's and so that took us a little more time.
Ken Johnson (20m 57s): Both were approved last September and in 2019, we could bring a prefilled syringe to market immediately and then to deal with all the issues that I just laid out. We just need a little more time and happy to release that now in July,
Scott (21m 12s): That's exciting. It really, it really is terrific. As I'm sitting here holding it, I mean the, the leap and leap really is the only word from what I'm accustomed to, to this it's it's like they're not even the same species in a, to B to be honest, it's a, it's a great, a great advancement. So I mean, whoever that guy is, you figured out how to make that, that liquid stable stuff is, is brilliant. Hey, have you ever used the Glucagon Isn't working on everything she's like, so the reason I asked is because while, while we were talking about this, he said, you know, we, we were talking about people administering it at themselves and I'm trying to think, I wish really trying to picture like, where's the tipping point where you're, it's gotta be, you know, it's not going to be one of those like, Oh, I got a little low, I need to eat something.
Scott (22m 10s): Obviously that's that's first, but there's probably a moment where you, I'm guessing, you know, imagine you're on a CGM and you see, you have double arrows down in your 50 a and you think, you know, you do the math real quick and you think, Oh my God, I gave myself too much. Insulin I can't catch this, do this like this. Right. Yeah. That made a lot of sense to me. I I've definitely been in situations where I thought, I don't know if I'm going to stop this with food and you know, and that's for Arden, but I really thinking about adults living by themselves. Okay. Can I have a question that I heard you say a second ago you were talking about self-injection and I think that there are many people who might assume that Glucagon has only for when you are having a seizure or an unconscious, but how would I self inject if I'm having a seizure or unconscious?
Scott (23m 4s): So obviously that's not the only time to use it with when are the times I'm supposed to be using this or, or I'm able to.
Ken Johnson (23m 11s): Yeah, I think that that's a great discussion. Thanks for raising that point. So I think, you know, there are a number of settings. Everybody has their own personal experience with what they deem very low blood sugar. I think you, in some of your colleagues have taught me this phrase, the, I don't know, low. Right? And so when that happens, it could be because you are looking at your numbers, it could be because you start to feel differently. And you know, some of the sort of classic signs and symptoms are, you are shaking. You're dizzy, you confused, maybe you haven't changed your personality or, or more combative, you know, trouble answering questions. Those sorts of things are all kind of hallmark sciences I'm going low.
Ken Johnson (23m 52s): So when that starts to happen, of course, the first rule of thumb is try to correct it with food or drink, right in your favorites. A source of glucose for many, many decades now has been referred to you as the 15, 15 rule, you know, take those 15 grams and the 15 minutes and see if it's work, if you're improving. So that's one situation maybe that isn't working and it's a stubborn lo and you know, you're starting to now wonder what's next. So that would be a time to consider administering Glucagon. And I think most people would not have reached some state of incapacitation where if they were familiar and able to a administered the auto injector where the prefilled syringe, they can, there are other settings where people are unwilling or unable to swallow or to have enough, you know, stuff available.
Ken Johnson (24m 43s): Maybe there a place where they don't even have access to a source of glucose. That would be another situation. If you feel like your passing out and there's somebody with you, obviously you'd want them to be able to administer it so that the community discussion, he should know the other people in your life, be familiar with where, with the gun it is and how to administer it. As you pointed out this HypoPen auto injector, it's a super intuitive and the instructions are printed, write on the pouch. And so I think if somebody found you and you said, you know what to use it, you know, it's going to be very straightforward process. We have tested that and found that in simulation exercises where someone is going through simulation or of an emergency in a very low blood sugar, they were able to administer correctly 99% of the time, follow the directions and do the two step process that you just talked about.
Scott (25m 34s): When the, when the trainer arrived at my house, I took it out of the packaging, took the instructions away from it. I handed it to my wife and said, I told her what it was. And I said, don't even think about it, try to use it. And it didn't take her 10 seconds to figure out what to do with it. And nobody here has ever used, you know, an epi pen or anything like that. So we've never held her or seen anything like this before. And I made me feel like, I hope my insurance company will cover a bunch of them or spread them all over. Arden was a college experience when she leaves for school. For me, I'll just, I'll just put one everywhere. It just really was intuitive. Is the word for it. It's you can't look at it and hold it and like eat.
Scott (26m 16s): There's no other thing to do with it. I don't know if that makes sense or not. You know what I mean? Like it feels like there's just one way to accomplish something and it, and it shows you that while you're holding it, like you said, it's in the instructions, but I'm seeing when you have the physical things in your hand, it's not like there's seven levers and you've got to decide which one it is. It only does one thing. And then, you know, if it does it well then perfect.
Ken Johnson (26m 37s): You know, I think, you know, that was part of the design, the understanding there's a whole area of science, human factors, research the services. How do we approach? So to solve a problem. And, you know, there's very, very intentional features built into that auto injector. The colors are intentional, the little window that you have that shows the liquid Glucagon, you know, in there. And it disappears. It turns red when the dos has been delivered, that's intentional. The clicks that you hear, those are intentional to let you know the sort of audio queue that the cycle it has been completed. We also have safety built in when you finish the injection and withdraw the plunger from the bare skin, it locks out.
Ken Johnson (27m 19s): And so you cannot have a needle stick because there is a needle inside the device, but it's, you know, never appears during the process of the injection. And when you're finished is locked out. So you can't have an accidental needle stick. Can I ask
Scott (27m 32s): Where can, can you just inject it? I mean, anywhere, like where has it, where did you, where were you able to get the FDA approval? And how do I remember that when I'm going low? Like, you know, or is it just anywhere I can get it into me is good.
Ken Johnson (27m 47s): And we, we concentrated on three areas, thigh, abdomen, and your upper arm. So we figured out, in most cases, one of those is going to be readily accessible. If you do have to have bare skin, because we want to make sure, you know, this is a 27 gauge needle. We want to make sure that there's nothing sort of inhibiting its path as it goes into the skin. But you know, we, in our assessment, Scott, most people opted for the abdomen. I think it was probably an easy to just pull your shirt up. And most people have an adequate real estate there. So, you know,
Scott (28m 20s): If I'm going to say I'm okay, I don't, I might all need Glucagon, but I'm a, but I definitely have a place to inject it. So,
Ken Johnson (28m 27s): So, so any, any of those three sites and it didn't matter, you know, the results, the clinical changes that we saw were the same, regardless of psych.
Scott (28m 35s): Well, that's even, that's very exciting because like I said, for people who know about older products, it's a, we were always taught, you know, deepest part of the buttocks, you know, like it's a, it's a big needle, you know, it's a, it's not an exciting, not an exciting endeavor for certain. So even that's a huge leap is my insurance got to pay for this. How do I, I mean, that, that's part of your purview, right? When you were talking earlier about what it is, you're a, you've done in the past. And so you, I'm assuming you have some background on this. You can talk about it a little bit. Yeah, I do.
Ken Johnson (29m 10s): If you know, and you never want to have a drug approved, but then not have any access for people. And so, you know, that's an important contribution that the company had to make in terms of going to insurance companies, going to pharmaceutical benefits management companies, you know, very close to the time of our approval last September and have these discussions about why it would be so critical to be able to offer this new a much easier, much more approachable version of Glucagon and the one they have been covering. So there wasn't any restriction on your Read KIS. And so we ask, can you give us the same treatment? And I'm happy to report as we sit here today for a commercially insured individuals, if you have unrestricted coverage at 87% of plans in the United States.
Ken Johnson (29m 54s): So almost 90%, wow. That, you know, why isn't it a hundred, there's no product that ever has a hundred. So there's always some small portion where there's going to be additional requirements. So that would mean that you would probably still have a copay and everybody's plans are different. These can be very, but you won't get one of these not covered types of messages. And the 87% of covered lives in the United States for commercial insurance. If you look at Medicare, probably the next biggest segment for people with diabetes, who should have Glucagon is about 80%. And then we're still working our way through the Medicaid requirements and were about four to 30% on Medicaid.
Ken Johnson (30m 37s): So if you know, for most folks, your not gonna have any significant access issues in terms of affordability, we are right now, if you go to glucagon.com, you can get all the details on a copay assistance program. And the net effect of that Scott is you would have a $0 out of pocket for the HypoPen for the, for the present time. So we're, we're starting out the launch of the product, offering that additional support, which means if you say had a $30 copay and you qualify it for the program, the company would subsidize at $30. He is essentially received it for free.
Scott (31m 15s): That's excellent. A great what was the,
Ken Johnson (31m 17s): The webinars Gvoke glucagon.com. It's GV. Okay. Now I've had a few people say, gosh, how do you pronounce that? But a GV. Okay, look again on.com.
Scott (31m 29s): Glucagon.com. I got it. And I'll put it in the show notes so people can find it too. So if someone's using a different Glucagon right now, and they've heard you on Thank I'm would like to try this, do they wait to their next appointment, go to their doctor and say, I want to switch my Glucagon are, or what are the pathways to making the change?
Ken Johnson (31m 49s): Yeah, I think any of those might work. I think traditionally, when we need something new, we would contact her in health care provider and se there's a new Glucagon and it's called Gvoke HypoPen. Can you send me a prescription for that? Can I get a film, our experience with clinicians if they are pretty well aware now, but this is a configuration that's on the market. We've been working hard with a professional society's and through their channels to make sure that they know that as a personal Diabetes requested that they would, you know, no of it and not be afraid to read the prescription because have the access issues. Now you have also been cleared that makes it very easy for them. So it's not very cumbersome if you don't want to pursue it that way and just make a call to the doctor's office, usually does not require a visit.
Ken Johnson (32m 34s): Scott it's just a, you know, a new script is an issue from the electronic system. You can pick it up. That's your favorite pharmacy. You can also go to the website and we've set up some services. They're a little bit more analogous to kind of ordering online and you can enter some personal information or information about your doctor. And we have support services available now through pill pack and Amazon company that will work with your doctor in deliver it to your home at no cost.
Scott (33m 5s): I'm not sure I heard you, right. Is it PillPack?
Ken Johnson (33m 8s): Yeah. So the Jenny that helps assist in sort of the transactional part of this is PillPack. It's an animal Amazon company. A but the easiest thing to do is to go to
Scott (33m 50s): Right? So if someone listening just feels that economically they can't do this, they should be able to and contacting you is the way to go.
Ken Johnson (34m 1s): It is. And I think Listen, there are, there could always be some leg and whether or not the coverage policy has caught up and maybe their getting a strange answer about how much their out-of-pocket would be and things like that. We have a whole assistance program in place to help navigate that. We know how frustrating that is, you know, we wanted to make Glucagon easy to use, and now we want to make getting a prescription filled, easy to do. So, you know, we have very, a nice set of services that are linked to the website. There's also a phone number at the website. And in case it's easier just to call and talk to a real human, but you know, that takes you through a whole tiered process of, you know, is it going to be covered?
Ken Johnson (34m 42s): You know, what pharmacies have it and so on and then write down to even, so the patient assistance programs for folks who can't afford their medication,
Scott (34m 53s): The concept of having to mix Glucagon stopped us from using Glucagon when Arden was legitimately having a seizure. I just don't know that. I mean, you know, technology's better now, obviously, and that's great, but I don't see, I can't imagine going backwards on this one, like this to me seems like the best it's available. Right. I was wondering, do you hear from people about mixing and what did they, what are the responses? Do you think that that having to mix the Glucagon stops people from even considering it as an option? Sometimes
Ken Johnson (35m 33s): I think given that that was all of that, there was all that was available
Jenny Smith, CDE (35m 39s): For such a long time. I mean, you know, again, thankfully my parents never had to deal with that. They never had to mix it. They never had two. It was always there. He always knew where it was in the house, but I, I would say that it's certainly a deterrent to use because it's, there are just the extra steps, again, as you brought up in your situation, it's like having to think through those steps when you got your loved one, either having a seizure or you've discovered them completely like not with it at all out, can't talk to them, whatever your brain is thinking in terms of helping them.
Jenny Smith, CDE (36m 24s): Yes. But all the steps of mixing, making sure it was mixed right now, you've got in the needle on that. I mean, this is scary looking needle, compare it to a syringe needle for Insulin. It is, it's a bigger needle, right? So, you know, imagine putting that into your two year old or even your 12 year old child and knowing that you're doing it the right way. And I can say that it would be a it's a deterrent, although I dunno, in the case of not having anything else as an option, you figure it out, but it's certainly going to be,
Scott (36m 58s): Well, I have a friend who recently had a teenage son, a have a seizure and she got the red box out. She got it mixed. And when she went to draw it back out, like in the, what your describing, running upstairs, people yelling, she broke the needle off in that crazy. So they had to go to a secondary option, but they were getting ready to use it. And she, she was trying to traverse there's and mixed Glucagon at the same time she was running to where it was happening, you know? And I think, I just think that that's the point, is that anything that simplifies that is genius and putting it in, you know, what can be described to people who don't know any different?
Scott (37m 44s): Is it as an epi pen style? Like just this thing in your hand that you just push down and hold this, turns it into something people can carry with them.
Jenny Smith, CDE (37m 52s): Absolutely. I even think two from a school type setting, even the comfort level of, let's say for some reason, you know, technology is down your not able to contact the parent. You don't know exactly what to do. I mean, from the standpoint of safety and feeling okay, and teachers or the Peros or whoever's helping at school, this is a hundred percent easier.
Scott (38m 17s): I think this takes away from that thing that a lot of people who aren't, who know, who have kids know, you go to school and you're like, I need somebody to be a Glucagon advocate from my kid. And everybody's like, no, thank you. You know? Like, like they really do too, like teachers, or like, I don't want to be on the hook for this, but, but this is like, again, I think this takes away the possibility that they can make a misstep in the middle, like drunk when Arden was a little, her, her directions were drawn up half the vile. You should have saw the fear that put on someone's face. Well, how do I measure half of the vile? I'm like, I don't know. I bought it. And they're like, what? I'm like, Oh, here we go. This is fine. After I get either the prefilled syringe or the HypoPen, how long do they last until they need to be replaced?
Ken Johnson (39m 4s): Yeah, that was part of our design criteria. We didn't just want to make a liquid ready to use if you wanted to make sure it could last a long time because you know, hopefully once or twice a year event and most, and even if it's a never event, you know, let's do not have to replace it too often. So right now, from the time of manufacture to the end of life or a potency, a sufficient for a re restarting, the blood glucose it's two years, but it's a very long shelf life. You know, we, again, you know, that was part of the design process and certification process and approval with the FDA that we have a two year from time to a manufacturer expiration.
Ken Johnson (39m 46s): So that'd be printed on that other product. You'll know when it expires a number of pharmacies. Now you can have reminder programs. So, you know, it's time to get at all.
Scott (39m 54s): Can I have to tell you? And I genuinely mean this. I've spoken to a lot of people who work for peop you know, manufacturers of different drugs and devices, and that's the first time anyone's ever said anything to me that almost knocked me off of my chair. I just took two years. Is it's amazing. And not what I expected you to say. That's because what I was going to say is, you know, we got the prefilled syringe, and I had a question about that actually, before I go down my story, we got the prefilled syringe and it comes in sort of a pillow bag is my best description of it. And my first thought was, huh, there's a needle in there. And this is sort of a bag. And then when I reached out to the people who are listening to the podcast, that was actually a question they had was, you know, why does the like, explain to me why the, the needle is safe in this bag?
Scott (40m 41s): And I guess, I guess thinking couldn't it be deployed, but to answer that for me first, obviously you didn't make something and not think, Oh, I wonder, you know, I'm assuming it's been tested, but explain to me how you came to the, the packaging for the prefilled syringe.
Ken Johnson (40m 56s): Yeah. It serves to a number of purposes. The packaging is a sealed foil pouch. Its done a very, a controlled environment. The prefilled syringe that if you describe Scott actually has a noodle shield on it and also has a backstop to keep the plunger from being deployed. So why a pouch? I think you started with that question. So first of all, the instructions are printed on the pouch and we want to make sure because you know, the real estate on a, on a prefilled syringe where the real estate and the auto injector is not sufficient to describe how to use it. It would be six point font and we wouldn't be able to read it. We have these very clear pictures and words printed right on a pouch that could tell anyone how to use it.
Ken Johnson (41m 42s): In fact, we tested that we have people who are untrained in the administration of the prefilled syringe and the auto injector and they successfully administered it. You know, like I said before, 99% of the time. So the second is that foil and the gas that we pack it in inside there. Cause you notice its like a pillow because its actually has a pressurized it's in there helps with and moisture because those are the enemies of any drunk. It doesn't matter if it's Glucagon or anything else sort of protecting it from light and moisture helps contribute to that two year shelf life. So we, we can't stress enough that you should keep it in these pouches until the time you use what people are.
Ken Johnson (42m 25s): You know, people may say, well, it's, here's how I know what to do. What's inside the pouch. So that's why we've provided videos. That's how it could be provided the demonstration units. Like the, when you have, you know, they'll be available in the clinics. Doctors have been requesting those demonstration units. So if there should be no mystery about what's inside the pouch, but we do acid if he started in that until the time of use and it's, you know, so multifold purposes for having that pouch
Scott (42m 52s): Is it all makes sense. It just, and had, I probably thought about it longer, you know, what it really is is that it was just different and so than what I was accustomed to. So when I saw it different felt wrong and now you explain it to me and like, Oh, well different seems like more well thought out in a new and better. So a that's excellent. Can I give you
Ken Johnson (43m 11s): If you want to anecdote as we were testing that power and sort of the size of it and how big the print was and everything else, we've had a number of Diabetes educators as a part of our forum for focus groups. And there was some that wanted it even bigger because they wanted to write all kinds of instructions and the margins and the doctor's phone number and you know, reminders about other things and stuff. That's like at some point we had to say, no, you know, we can't add to it, this giant pouch, it's gotta be small enough and portable enough. So, so, you know, there, there were a few rounds of the things that, you know, let us to the current configuration,
Scott (43m 41s): If they did, they have it up to the size where you could put three holes in it and people get carried around in their binders.
Ken Johnson (43m 47s): They're, you know, so, so know is all intentional and a contributes to the, the long shelf life. It contributes to the successfully administering it and at the time of emergency and it also protects the product
Scott (44m 1s): Going back to the beginning of this thought for me, what I was getting ready to say, when I asked you how long does the product last before it needs to be replaced? What I was gonna say as I think I'm going to get to move on to the HypoPen afterwards, because I can see how, you know, it's just, it would just make, I think this would be easy to show my daughter and say, look, if you really feel like you're in trouble, do this. And it wouldn't feel like, you know, a rigmarole I guess, and, and, and maybe off putting in any way. And so I thought I'll switch, but now I realize I've gotta wait two years. I switched. So a, I M
Ken Johnson (44m 34s): You bet you brought up another issue and that is keep people, staged them at different parts of their daily life. Right? If you keep the prefilled syringe and the nightstand at home, you might have the auto injector at school or with the coaches or wherever. So, I mean, you know, mix and match again. There's no difference that in the Glucagon is contained any of their device for the product.
Scott (44m 55s): No, no, no. I, I, and I, I guess I was half kidding, but I do know that, you know, there are different Podcasts if our kids ever grow back to school, she'll need one for school in, in a couple of other places. And it just, you know, I can't, I can't say it enough, it's the, it's easy to have you on the show and talk about it. Because like I said, this is a leap and this is going to make people's lives. I think easier if they should ever have an emergency and need to use it. And I think the comfort they're going to get from it, just having it around Is is going to be different. I, you know, I really don't mean to pile on somebody, but that, that red box is not comforting. It's off putting, and this, this thing I'm holding this pen here is comforting. So there's a lot to that.
Scott (45m 35s): There's a lot to the psychological, the psychological side of all this. And I appreciate that. That was considered,
Ken Johnson (45m 42s): You know, we've talked with folks sort of who lived through all of this and seeing the changes in technology and new delivery. Insulin certainly advanced and the bringing forward CGM pumps are, you know, all these things have been stepwise improvements. Glucagon just, wasn't tackled. And, and, and now that we have, you know, we want to keep making improvements and exploring other other uses for it and beyond the, the, the currently approved one. And so the companies, you know, vested in making the most of a liquid ready to use Glucagon. And so, you know, stay tuned for more. Now
Scott (46m 20s): That as I was jumping on this call, I got a message from somebody. It was so funny. They don't know the timing of my schedule, but they just were like, if you, if you haven't spoken to the people at chief Oak, yeah. Can you please ask, is there a water and Insulin and if there's water and insulin can, can, Insulin be made more stable with their technology. And I was like, I dunno, I'll find out. So I, maybe my bigger question is, are there other things your stabilizing over there, or, or you just the Glucagon company, or is there more,
Ken Johnson (46m 54s): You know, we are more than a, Glucagon a company. So at our core, we want to take the technology to make liquid ready, to use easily injectable, very stable products and all of the areas where it makes sense. We have talked about it Insulin and it's a, it is a project and it's not anything that's a, you know, advanced in terms of it's Clinical Development. But we do recognize that there are limitations on the storage conditions for Insulin or other things that it can be mixed with cost problems. So maybe we can start to combine it with other effective, low blood glucose agents and make a better combination. So, umm, the, the short answer is yes, we can apply our technology to a broad range of drugs, proteins, monoclonal, antibodies, vaccines.
Ken Johnson (47m 42s): And so, you know, that's, our mission is to take all of the concern and the difficulties of administering and storing and drug out of the equation. And so that's, that's kind of the, the future state of zero S and, and how we'll apply ourselves. But you know, us now as the blue thing, as a company first and foremost, and a, you know, and we'll use that as a starting point and grow from there,
Scott (48m 5s): Your technology applies to a lot of other things. So they're, there are probably many things that we can't talk about that are being considered there. And I'm asking that question as a wink and a nod to all the people who asked me questions that are not covered by your FDA approval. So I can't ask you here, but they'll all understand where they hear this and be excited that you're working on other things I think is that fair?
Ken Johnson (48m 28s): Oh, that's definitely fair. And our company website to a separate from a DeVos glucagon.com describes some of our pipeline and the things that are still in an experimental phase. And you'll see that it's, Glucagon, it's a drug called die as a pan for seizures in other programs. So we're, you know, we're, we're really interested in applying this technology broadly and solving problems for patients and their providers,
Scott (48m 55s): If it's possible that I'll ever be able to get G Voke in a vial for home use to just keep and administer as I need
Ken Johnson (49m 4s): What we would like to pursue that. Yes, I think, you know, there are a number of applications of Glucagon that are different than our are approved used today. It's a one milligram, you deliver the whole dose, a in the setting of restoring very low blood sugar, but there are other settings where maybe the smaller dose would be useful. And, and so there or other settings, whether it's exercise, whether it's hypoglycemia, unawareness, other things were, there are a series of, you know, Clinical Development projects that we've sponsored. We've collaborated with one side as well as a part of a dual hormone delivery with Insulin and Glucagon as part of a closed loop system.
Ken Johnson (49m 45s): So in a, none of these are approved, none of them are a possible with the current configuration. We would need a vile of Glucagon as you describe the Scott. So it'd be very similar to how you would administer Insulin. He would have personalized doses for the situation that your trying to manage. So that's gonna take us some time, but we are investing in those efforts, you know, just ask everybody to stay tuned for more.
Scott (50m 10s): All right, well, I'll say this from my heart and many people may or may not understand this. And I guess if you've been around Diabetes long enough, if it makes sense, but it may not seem super exciting that someone figured out a way to make Glucagon liquid stable, but is super exciting and that it opens many doorways and possibilities for the future. Everyone who has someone that they love with type one diabetes or has type one diabetes, should be incredibly jacked up and excited that you guys figured this out. And I know that it, it's hard to wrap your head around why this is that exciting, but it is. And I'm, I'm very much looking forward to what happens next. So I really appreciate you coming on and explaining all of this.
Scott (50m 52s): And I thank you for your time, unless you want to play some piano. I think we're good.
Ken Johnson (50m 57s): My pleasure. Scott I enjoyed it and hopefully we can do it again sometime. And my best to Bailey you left the room,
Scott (51m 8s): Dammit, cameo bark. So you'll have to cut that part. So I thought I could get a little park at the end and we'd be finished anyway. Thanks so much. Enjoy the rest of your day. Really appreciate your time. All right. Appreciate it by huge. Thanks to G vote for sponsoring this episode and for giving me the opportunity to just speak with Ken and a huge thank you to Jenny Smith for being such a good friend and coming on the show to talk about Gvoke. If you'd like to find out more about you Vogue, there are links right here in the show notes of your podcast player@juiceboxpodcast.com or you can just type the words
Scott (52m 1s): I have a little bonus stuff here at the end for you. If you'd like to keep listening, I actually spoke to Ken the day before we recorded this just for a few minutes, so we could get to know each other. And he told me about his piano playing. So I brought it up at the beginning of this recording while we were getting the audio set up. So it was recorded, but not really a part of the episode, but I left it here. Cause it's interesting. What kind of music do you apply? So,
Ken Johnson (52m 28s): Oh, I'm like what they prefer to, I guess, as a professional journeymen, sidemen I'll play whatever, whatever comes on my way, I read music, you know, I play from classical to jazz, to tribute acts, including pink Floyd and van Morrison and a REIT, the Franklin and two classic wedding bans. You know, the most cliche kind of lounge music. You can imagine it doesn't really matter a musical theater,
Scott (52m 55s): The multiple instruments or not.
Ken Johnson (52m 58s): I'm a piano player, keyboard player.
Scott (52m 59s): That's really, that's an amazing skill to have. That is very cool. And it's great that you get to do it too.
Ken Johnson (53m 5s): Yeah. So Chicago, you know, traditionally has been famous for lots and lots of live music. And of course, many famous bands have come outta here, but we're a complete shutdown now. It's just awful.
Scott (53m 18s): And online really doesn't replicate it. There's been, I think one or two people who have done it well, you know, and it's, you know, you have to, you can see how much money you have to have a, in a crazy example is that, I don't know if you saw, you may not like this kind of music, but maybe you do. You mentioned pink. Floyd Metallica did an old song acoustically remotely. So all four guys were in a different place, but it sounds like it was recorded in a studio. So you have to assume that each one of them has a professional recording studio in their home, you know, but that worked out, but,
Ken Johnson (53m 51s): And that's exactly how they do it. And what we are led to understand as consumers is they record all those tracks independent of each other, and then somebody who mixes them because you can't, you can't use zoom to have simultaneous music because whoever's talking to the loudest takes over the channel. And so there's, there's no mixing up on zoom. It's a, it's a big problem.
Scott (54m 12s): You know, all that equipment and the willingness to spend a couple of million dollars to mix a song together to release it. And they had that money and they did it. And everyone else is just like you said, fumbling through trying to do in a resume for those of you who are not familiar with a podcast and don't know who Jenny Smith Is I thought I'd take a second to let you know Jenny is a frequent guest of the show. She's helped me put together series within the Podcast like defining Diabetes, ask Scott and Jenny. And of course, the very popular Diabetes pro tip episodes and of all of the people I could have had on those episodes with me. Here's why I picked Jenny. Jennifer Smith has had type one diabetes for over 30 years since she was a child.
Scott (54m 53s): She holds a bachelor's degree in human nutrition and biology from the university of Wisconsin. She is a registered and licensed dietician, a certified diabetes educator, and a certified trainer on most makes and models of insulin pumps and continuous glucose monitoring systems. I love Jenny. She is a friend. And when I decided to do this episode, I asked her if she could help out a little bit and she was very gracious and said, yes, Jenny works, has integrated Diabetes so you can check her out. If you do, like@integrateddiabetes.com.
Please support the sponsors when you’re able and it makes sense for you. This episode was sponsored by Gvoke.
LEARN MORE about the HypoPen and other Gvoke products HERE
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
# 324 Gvoke Glucagon
Gvoke is a premixed, prefilled, premeasured liquid glucagon
Paul Edick is here to talk about his path to becoming the CEO of Xeris. Xeris makes Gvoke. The premixed, prefilled, premeasured liquid glucagon for treatment of very low blood sugar in adults and kids with type 1 diabetes ages two and above.
Learn more about Gvoke here
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
This episode of The Juicebox Podcast is sponsored by GE Volk, the world's only liquid stable glucagon. g vocus. a prescription injection for the treatment of very low blood sugar in adults and kids with diabetes ages two and above. Do not use if you have a specific type of adrenal or pancreatic tumor, starvation, or chronic low blood sugar. Side effects may include nausea, hypoglycemia, vomiting, headache, hyperglycemia, and injection sites swelling, itching and stomach pain. Being prepared is always important, but right now it is at the forefront of all of our minds. Did you know stress in erratic schedules can increase the risk of scary lows. g Vogue prefilled syringe is the first liquid glucagon that is pre mixed prefilled m pre measured so it's ready to go. If you need g vote PFS and can't physically get to your doctor's office, there's still a way to get it. You can request a prescription online and pharmacist at pillpack by Amazon pharmacy will reach out to your doctor for a prescription. They will then ship your G vote PFS to your home at no additional cost, just the cost of your copay. Please note at this time, this option is available for people with commercial insurance only. You can learn more including a link to the important safety information about g vote pfs@www.ge Volk glucagon.com, forward slash ordering dash g Volk, it might be hard to remember. So I'll put a link in the show notes.
When I first suggested that Paul, come on the show, I didn't know anything about his history. So I started at the beginning, asking him how did you get involved in this kind of work? And the answer took us on our ride that I just did not expect. I really found it fascinating to pick through someone's life and see where they started and what they thought they were going to do and find out about some of their first jobs that have, you know, seemingly nothing to do with what they end up doing. So sit back and relax. And we're gonna find out how a young boy from New York ends up being the CEO of the company that brings the world's first liquid stable glucagon to market. A glucagon that is pre mixed, pre measured and ready to go. It's kind of fascinating. One last thing, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, and to always consult a physician before making any changes to your health care plan. Yeah, there was just like, there is like air behind you. And it's like, oh, god sounds like you were on the highway.
Paul Edick 2:51
Well, so where our building is located. We're surrounded by train tracks. Well, we're on the 16th floor. But you might hear some train noise in the background. Don't worry, a
Scott Benner 3:07
fighter jet will fly past Dexcom once in a while when I'm speaking with them. adds a little flavor.
Paul Edick 3:14
Well, we chose to put our office close to the train station. So everybody could have an easy commute. So it's a nice idea comes with its
Scott Benner 3:23
Can you take credit for that? Or Where was it? Not your idea? And you just take credit for it? Oh, no.
Paul Edick 3:29
I've done it in two companies now is very purposeful. Okay. very purposeful. Yeah, we promise everybody will be within four blocks of a train and train station or l stop.
Scott Benner 3:38
That's really excellent. That is and you guys are located in Chicago.
Paul Edick 3:42
Downtown. We were one block south of the river on the sale. Nice
Scott Benner 3:47
is that and by the way, we are recording already.
Paul Edick 3:56
I'm Paul edic. I'm the CEO of zeros pharmaceuticals.
Scott Benner 4:01
Obviously, we're just talking as we picked up the column, Paul didn't know we were recording but now that he knows we can just kind of keep going. It's funny now that you said that I want to go in a direction. And I guess I just Well, are you. Not a young man? Paul? Not right out of college, I'm guessing.
Paul Edick 4:18
No, I've been in the pharmaceutical business. This is my 41st year, but I just turned 64 in July. Okay. All right. I've been doing this a long time.
Scott Benner 4:28
So things that other people may not think about, like I'm gonna put a building up and we're gonna get a company rolling and it should be near transportations, so that hardworking people don't then have to schlep home and get you know, like and cause problems for them. That's the stuff you learn over time, I imagine.
Paul Edick 4:44
Yeah. You so if you a lot of companies they locate in office parks in the suburbs, and people are landlocked and there's no real energy. It's just in the building. We you know, I look in the suburbs, and there's all the normal land, you know, buildings. But when you come into the city you can locate in buildings where it's vibrant, there's a lot going on, there are people and movement and energy. And the commute is actually shorter by train for most people than driving two buildings in an office park in the suburb. So it, it helps with the energy of the company. But it also makes it easier for people and therefore you attract people better.
Scott Benner 5:31
I'm incredibly interested about how it gets set up. But I guess I have to, I have to go backwards before I can jump into forwards. So let's start slow. Where did you grow up?
Paul Edick 5:41
I grew up, excuse me in a small town in, in a dairy dairy country in upstate New York. So for for people who are in New York City, upstate New York is Poughkeepsie. I grew up about two hours north of Syracuse, just just a little bit before the St. Lawrence Seaway. very rural, very small. What did your parents do? When I was a little kid, my dad was worked in a Chicago pneumatic, which was a tooling company. My mom worked in a shoe factory.
Scott Benner 6:17
I asked because, you know, growing up in a small town that's, you know, pretty removed from what I would think of is big business. And coming from, you know, your parents doing what they did. And I think of myself, and I always used to say to people, like, it's hard to imagine something other than what you know, you know, what I mean? Like, I know, you know, like, I know, people who want to be professional athletes, but when you look at them, they grew up around a professional athlete. So it seemed like a reasonable thing when I was young, I wanted to write, but that didn't seem like a viable way to make a living because the people I lived around were, you know, kind of hard working blue collar people. And I don't think that writing something seemed like a, you know, a reasonable way to make a living. So I, so I'm fascinated about how you made it from there. To here. I wonder, did it happen in high school or not till college? Where did you start thinking about business? Are we just trying to get out of a small town or how are you feeling?
Paul Edick 7:10
Yeah, great question. I started as a little little kid in Central New York. And then we moved to this town called la ville, in upstate New York, after my dad, finally, he got a degree out of Syracuse University became a teacher. My mom was able to get out of the shoe factory, became a secretary. All I, I you know, in terms of aspirations, from a career perspective, I don't really recall having any I think my aspiration was to do better than my parents. I grew up in a second generation, Italian immigrant family. You know, my mom couldn't speak English. When she started grammar school, I was an athlete. And I had opportunities to go to college for free and a lot of places around the country because of athletics. And I was a pretty good student. But I ended up going to a small, private college called Hamilton College, Central New York. And coming out of Hamilton, it was time to get a job. And I, I interview on campus got a job with Procter and Gamble, my entry into the pharmaceutical businesses, accidental, to say the least
Scott Benner 8:23
yet see, it's interesting, because you're describing You know, I'm, I'm 48. So I'm not of your generation, but I'm probably not too far along, but my parents definitely had that vibe about them the idea that you were just trying to do a little better tomorrow than you did today. And and kind of get get through it. There was no grandiose ideas like this is the thing I'm going to be one day you're just like, I need to get up in the morning, go to school, learn something, go to college, learn something, get a job in that. It's funny how I don't think people now think like that as much like I think they have plans for themselves and ideas.
Paul Edick 8:58
Oh, no question. No question. Every every, every kid I talked to wherever young person I talked to, you know, how do I get to Xyz? And, you know, the first thing I say to say to people is keep your head down, do your job and the rest will take care of itself.
Scott Benner 9:15
Yeah, I'm always amused by my wife will tell this great story about she hired this person. And after 30 days, they came to her very earnestly and asked when they'd be getting a raise. And you don't even understand what the job is yet. You've only been here for 30 days. She said, I've never been late. and was like, well keep keep you keep that up. Okay, thanks. I get out of here. And she's like, I she came home and she's like, 26 year old person doesn't really even understand what our job is yet. Once a race once and I was like, Yeah, good luck. No, that is that's, that's really excellent. So yeah, so your parents weren't as much. They were immigrants more than that, like so I say. It's funny. I applied. by today's standards too, and I just assumed like, that's the job they had. But they were working their way up as well.
Paul Edick 10:05
Yeah, my grandparents came over, you know, on the proverbial boat from Italy, right, my mom was born in the States. But in those days, they lived in an Italian community in a small town. And they spoke Italian, interestingly enough. And we always tell these stories, but my parents, my grandparents refused to speak Italian around us kids, because they lived in a world where they were discriminated against. They didn't want us to speak that language or even have an accent. You know, fast forward to when we're teenagers and adults. And we're kicking ourselves that we don't have two languages.
Scott Benner 10:50
Right. I mean, that's is how things have changed. But there's there's a safety idea more than anything, like they probably saw it as an impediment to your success if people thought of you as an immigrant.
Paul Edick 11:01
Correct. And assimilation. Yeah, right. There was a, it was an absolute drive to become and to assimilate that. It was fascinating.
Scott Benner 11:09
That's excellent. It's really, it's fascinating, because I don't think that we, I just don't think we talk about this a lot anymore. And this is really what our conversation today is about is trying to figure out how you got to where you are now and what your what your focus was. So you're saying, and I don't think this is uncommon at all, but in college, what did you major in first,
Paul Edick 11:30
I would started my freshman year as a pre med student. I had done, you know, National Honor Society, the whole nine yards in high school. So I had great grades. I was also a two sport athlete in college was a little bit different than I my very first semester, I got a C in calculus. So I was done as a pre med student. And so I, I switched to psychology.
Scott Benner 11:57
Paul's smartest kid and his class up there in New York didn't didn't shake out as well.
Paul Edick 12:03
Well, it was it was interesting. The biggest reason I got a C in calculus was because I was still using a slide rule. And if you even know what that is, if people and most of the kids in class had moved on to calculators, the very first Texas Instruments calculator, my parents couldn't afford it. I was still using a slide rule, and I didn't finish most of the tests on time.
Scott Benner 12:34
Okay. That's Yeah,
Paul Edick 12:36
so it wasn't for lack of knowing information. That was I couldn't get it done. Yeah. the right tools.
Scott Benner 12:42
Right. Yeah. That's so interesting. How many letters home said I need a calculator? Or did did your Paul Yeah.
Paul Edick 12:48
No, that was one that was one conversation that didn't go very well.
Scott Benner 12:55
Paul, did you ask for a calculator? And then your mom told you about being born in America? First generation Italian? No, I got the Don't you have a job and can't you work more hours that interesting. You know, My son is a sophomore in college right now. And he goes to a similar type of school. Actually, Hamilton is one of the schools he tried to let you know, he reached to. And so he's in a similarly sized school. He likes a smaller school, he wanted liberal arts. He didn't quite know what he wanted to do yet. And when I asked him about helping out he says that his job is good grades in baseball. I'm now I mean, yeah, I could put him on the phone with your mother.
Paul Edick 13:34
was interesting, you know, to make not to belabor the point, but I had offers for four year full scholarships to three or four different big time universities for sports. I chose to go to Hamilton College, which is division three, and they couldn't, it was non scholarship. So I actually had to pay to go to college. Yeah. And that was a decision I made that don't from my parent's perspective. Okay, well, you got to pay for it. Right? Because they sure as heck couldn't. Yeah,
Scott Benner 14:05
no kidding. I do think that my son Cole did the same thing. He that he had opportunities to go play baseball places that were, in all honesty, just schools where you would have played baseball, you come out with some sort of a degree, but I don't know how great it would have been. And he said, I'm too good of a student for that. I have to go somewhere and get a get like a real solid education. That's like Okay, great. Yeah, get over there. But the same thing, you know, there's not quite as much in the way of offering of money when you when you make that decision. Exactly. Okay, Paul, so you're in college, you're you're kind of jumping around finding your major and everything and finding your level really like looking for where you fit and where you're good. And did you find Did you fall into business at that point, or did you finish with a more of a mathematics track? How did you handle it?
Paul Edick 14:49
No, I actually, I moved to psychology. I was fascinated by learning and memory. I actually did you know, my sophomores sophomore in junior years. did research and learning and memory, so not behavioral psychology but more the learning aspect of psychology. I loved it. And my research was actually published. And I graduated with a liberal arts degree. You know, I took a bunch of other courses, took a lot of religion courses, political science, you know, you had to take statistics if you're a psychology major, so liberal arts degree, and then I started interviewing for jobs on campus. Interestingly, because of the research I was doing, I was getting extra credit. I finished in three and a half years, I was one of the few people that was available to be hired in the spring. Because I wasn't going to school anymore. And I got a job with Procter and Gamble as a sales rep in their case food division.
Scott Benner 15:44
So that's something you just use thin the herd by being available sooner.
Paul Edick 15:49
Yeah. And because I was doing independent study during the summers, got extra credit. And I was done.
Scott Benner 15:56
Okay, that's interesting. So should you head off to Procter and Gamble as a young man? What was your expectation that day where they hired you? And you were probably out of your mind excited? Did you even know why you were going there? what you were doing or were you just like, this is a job.
Paul Edick 16:11
You hit the nail on the head. It was a job I, you know, I didn't know who Procter and Gamble was. I learned who they were. It was, you know, great training and all that. But I, big company, and I had a sales job. And it was, you know, in upstate New York, Albany, actually, Saratoga Springs, what were you selling? I was calling on grocery store managers. Selling Duncan Hines cake mix, Crisco shortening, Pringles potato chips, the original Pringles potato chips, the red wooden in the can that basically tasted like cardboard. And, you know, in grocery store managers, you know, like I said, everybody, they come in two flavors. They're either 65 and about the pinnacle of their career since they were 21. Or they're 21. And they're going to be at the pinnacle of their career until they're 65. I mean, grocery store managers, that's a life. And they grocery stores work on such small margins. If you're making 3% margin as a grocery store, you're doing pretty well. So they're intense. Its intense. It was great training, you know, I learned how to sell
Scott Benner 17:24
and how to read people talk to them.
Paul Edick 17:27
Well, you you very quickly have to understand their needs versus yours. You learn very quickly, if you if you're not really attuned to their needs, and how their store works and what they are trying to do. They won't even talk to you. Because they, they they are focused. It makes me want to ask you a personal question. Are you married? Y'all? Yes, yeah, for a long time. I'm on my second in both of them for a long time. My first marriage was 17 years and this marriage has been 18 years actually good for you. And I bet you, you stay out of trouble, largely in what
Scott Benner 18:06
I'm reading the signals and I know what to say now because I need you to buy some shortening from me. And
Paul Edick 18:11
yeah, yeah. Well, Crisco shortening. Yeah, it was. It was fascinating. It was interesting. I you know, but that's, that's how I, I accidentally ended up in the pharmaceutical business. I was in a grocery store, one of the first stores that actually had a pharmacy, it was an experimental store in upstate New York. And I was talking to the store manager about putting Pringles a big end to end tower of Pringles with beer next to it. And showing him how much profit he was going to make and how it was going to sell. And I was going to put a big sign up above it and all that. And there was a guy standing in the corner, watching me and it was a little disconcerting. So I didn't know you had a suit on and tie. And afterwards, he comes up to me says, you know, I'm from Johnson and Johnson, I'm from ortho pharmaceutical. We're looking for great salespeople. And he gave me his card and said, I'd like you to talk to my boss. And like, I don't know, three, four weeks later, I was working for j&j in the pharmaceutical business. Okay. You know,
Scott Benner 19:16
it's interesting. That's the that's the sales version of the somebody seeing you in the mall and going here. So pretty. Have you ever considered being a mom?
Paul Edick 19:24
Yeah. I don't, I didn't get that.
Scott Benner 19:29
I've just, it's interesting. And was that odd? In the moment? Even then, were you just like, wow, this is a strange situation.
Paul Edick 19:35
It was but it was. It was. It was an opportunity of a lifetime. It was Johnson and Johnson. Remember, I came from a little bitty town in upstate New York where, you know, in a county where there are more cows and there are people actually working working for Procter and Gamble. And now I'm going to go work for j&j. j&j was the most respected company in the world at that time. Right
Scott Benner 19:58
now you would open a medicine cabinet. I imagine they made almost everything and yeah and beyond.
Paul Edick 20:04
So it was it was the opportunity of a lifetime. It's excellent.
Scott Benner 20:07
I have to tell you that, you know, as you and I were getting ready to speak, it kept running through my head, how do you become a CEO? Because I kept thinking, that's not something a kid from high school says to himself, like, I'm gonna go to college and become a CEO. You know, I'm going to run a company, I'm going to make all of the decisions, everything is going to filter through me like that. I mean, if you were thinking that when you were 12, or 13, you probably had a mental illness, and they wouldn't filtered you out by that. Yeah. A little too great. Thoughts for a small child. And so there's no CEO track in college, there's no. And I thought, I wonder if this man's not going to tell me a story of, you know, finding something, doing it well, moving to something else, seeing something jumping around, it's so interesting. This is the way I look at my my wife sometimes. And I realized that where she is, was never once on purpose. You know, she just took a job because she needed a job. And she did her best and someone noticed, and it bothered. And it just kept going. And I wonder how many people actually have similar stories like that?
Paul Edick 21:04
Well, that's what I said earlier, I, you know, I just keep, as a younger person, I just kept my head down and did my job. And you might I was lucky, I work for people who they, you know, you do your job, they take care of you. So I never had to ask for a raise. I never had to ask for a promotion. I did my job and those opportunities presented themselves because I was in an environment where that's the culture, you take care of the people who are performing. I moved up in that company, and then, you know,
Scott Benner 21:42
you foster that. Now, when you're in charge. Is that is that a culture that you try to keep moving? Because I think some people would hear that as generational, but I don't think it is. I think it's, I think it's cultural. What a company.
Paul Edick 21:52
Yeah, it's very much cultural. And it's something that we foster a great deal. Over the years I've, I've taken from every company I've worked for, and every job I've had and different opportunities. It's funny, you say, I'm going to be a CEO, I'm gonna make the decisions that when you're CEO, he very seldom actually make decisions, if you're a good one, because you should have an organization that decisions are made at the level that they're that's appropriate. If If you end up if I end up in a situation where people are saying, well, we got to see what Paul thinks before we do that. It's like that's, we're about to fail. I find out about a lot of decisions. And because of the culture that we foster, and that I Foster, nine out of 10 decisions are usually pretty good ones. Yeah.
Scott Benner 22:40
Now it's it's funny you made me I'm from Philadelphia originally made me think of the Super Bowl a couple of years ago, where there's that great tape of the the quarterback running over to the head coach of the Eagles in a incredibly intense scoring possible situation. They just goes, you want to run this play. And the coach goes, Yeah, sure, go run that toy. And it was just like, it was just wow, he trusts him. He knows what he's thinking. It's amazing. You know, and, and I so I take your point?
Paul Edick 23:04
Well, trust is
I'm not a believer that trust is earned I, if I hire somebody that means I've, I believe that they're the right person, and I'm going to trust them. You can only lose trust in my world.
So I just think it's a different approach.
Scott Benner 23:27
g Volk is an easy to use pre mixed prefilled pre measured liquid glucagon, all you have to do is open the foil pouch, and inject it. Joke does not require refrigeration. It's available in two doses for kids and adults. And there's a simple two step process to administer it. I have seen a seizure from low blood sugar and take it from me, it is a harrowing moment. What you need in that situation more than anything is something reliable. That's easy to use. It doesn't require a ton of steps, because that is a you guys have heard me talk about on the podcast before but it is a crazy situation when someone is having a seizure and you feel like you're what stands between them and further harm. You want something that just works. And evoke is that thing, open the pouch, inject the glucagon, you did it. To learn more about g vote, go to G vote glucagon.com forward slash juicebox. But you get to that link, you can actually order g vote right now today through pillpack. Or you can take some time to understand what g Volk is. So the next time you go to your doctor, you can tell them I'd like to use this glucagon, it's premix. It's prefilled. I think it's going to be easier for me to use. I've read up on it. It's definitely what I want. You'll have some confidence when you go to the doctor, you'll know what you're talking about. So go to the link, check it out. Make yourself familiar with what Evoque is. Then you can decide if it's right for you. Arden I just made the switch at her last endocrinologist appointment. And I think if you take a look, you might want to do the same g vogue.com forward slash juice box with links in your show notes, or Juicebox podcast.com. To find out more about the world's first pre mixed prefilled, liquid stable glucagon. Let's get back to Paul, to find out about the rest of his crazy whirlwind life. I think it's opposite of what most people do. I think most people come in cynical and say, you know, you go ahead, show me. And if you're saying, look, I tried, you know, I saw you, I believe in what you'd said to me now go ahead and do it. That's, um, I think that's the way you build?
Paul Edick 25:48
Yeah, well, we have, like I said, I have taken from a lot of companies in this company, and to some degree in my previous company, but in this company more than any, we, we have one sheet of paper, it's got four boxes, and it's got a series of behaviors in each box. And what I've said is, if we can, if we can behave this way, we will build a great company we can be proud of. And if we do that, and serve our customer, well, in the process, we'll, we'll have a great company will be very successful. You know, we don't have goals that are about dollars, we have goals that are about the kind of company we're going to build the way in which we're going to serve the customer, and then all that other stuff will happen.
Scott Benner 26:38
Yeah. Now I talked to people a lot about management of diabetes and use of insulin. And everyone always wants to know, like, tell me what to do, like, Where do I how much do I use? When do I use it? How do I get my agency to come down? Like, it's always very point on it, and I tell them constantly, that's not what you want to be doing. You need to find the tools, the right tools, learn how to use them, and then all the things that you want will just happen. And you won't even have to, you know, wring your hands every three months. Like I hope my agency I hope isn't, you know, just it just sort of happens when you're using the right tools. It's so
Paul Edick 27:13
right. It's so fast about behavior. Yeah, the behaviors,
Scott Benner 27:17
the basics of most success in any kind of situation. They're all really very similar. Yeah, it's, that's really cool. So I see you're a J and J. You're young man, you've been plucked out of the grocery store. Probably smelling like pastrami and pretty happy this guy found you. And did you just go right into sales again at j&j?
Paul Edick 27:41
Yeah, I was a sales rep in the territory then, you know, sales trainer than a district manager in Chicago and a regional manager out in San Francisco. I was there for like 12 years, I left j&j. And went to Baxter, actually, was a good move.
Scott Benner 27:58
interesting how this happens, because I see this happen a lot to see you gain a lot of broad experience with a large company. And then suddenly, to a smaller company. You're You're like the hive mind. You've seen every little, little corner of the business and you kind of have experience in a lot of different places.
Paul Edick 28:16
Yeah, well, it was a I went to it was a Bachelor's of Medical Products Company fairly big years ago. It was a combination of Baxter and American Hospital supply once upon a time. But I was actually in a small division. So I didn't have any didn't really have the answers yet, because I went from selling pharmaceuticals detailing direct doctors about drugs to a division of axure that was called caremark at the time. caremark at that point in time was a home infusion therapy company, which means that you, instead of putting a patient in the hospital to get an IV, IV antibiotics, for example, okay, you send a nurse to the home and you do it in the home. But that business, you actually run it, you're running kind of like a hospital without walls. You take the assignment of benefits for a patient, you bill and collect on their behalf, you do the therapy, you do everything.
Scott Benner 29:13
You just don't have a structure that they come to
Paul Edick 29:15
correct. And in the learning, I learned how that health, I learned how the healthcare business actually work by by being in a service business, as opposed to just selling drugs. And then I took a detour from there, I met a gentleman who had an advertising agency in the pharmaceutical healthcare business. And he said, I got a lot of really good advertising people. I've got a lot of marketing people, but I don't know have anybody in my company that understands how pharmaceutical companies and medical products companies work. I actually went to work in that advertising agency for a few years, launching drugs all around the world and you coaching, and consulting with clients on how the healthcare business actually worked. In back then that was in the late 80s, early 90s. It was the advent of managed care, in what companies didn't realize is they weren't managing care, they were managing money. And it was, it was all about the, you know, the movement of money in health care. So if you understand what they're trying to do, you know, as a hospital from a financial perspective, then you understand how your services and or products fit into their world better.
Scott Benner 30:40
When you look today at healthcare, do you and you look at your job? Do you see that, you know, you talked earlier about when you're in sales, you have to understand what the needs are of the of the person buying? So now, I'm assuming you need to understand not only the needs of your customers, and what what they require from you, but you have to understand how to navigate the healthcare world? And do you? Do you find yourself just saying, I'm going to get in this canoe? And I know how to get through this these rapids? Or do you try to reshape the rapids at the same time? Like, how much of that? Do you see is your responsibility to move things? in the right direction for the future? And for versus, or maybe not versus but for the patients?
Paul Edick 31:26
Yeah, that's a great question over the last two decades, what I've come to believe, is that with intense focus on the patient, that's the only way you're going to truly navigate what's going on in healthcare. Because the controlling factors of health care delivery, to a larger and larger degree are all about money and less about care. And, you know, having been in you know, big pharma, and then in small companies, and, you know, started a couple of companies, I, my focus is on, if I'm going to do something, if I'm going to build a company, it's going to be around products that can change healthcare for the better products that can positively impact patients lives, potentially save lives, and reduce their overall cost of care. If I can't do those three things, I don't want to do it. Because it just the world of healthcare right now. It's just too difficult to do anything. Otherwise,
Scott Benner 32:33
I had no idea what you were gonna say, the conversation led itself there. And I realized, as you were speaking a moment ago, the only reason you're on the podcast, is because that's the vibe I got from the people you hired, who reached out to me originally. And, and I get, I get pinged a lot by a lot of people, and they're like, you know, they wouldn't be on the podcast or buy an ad and most of them I turned down. And that's because, to me, the podcast isn't about making money. The podcast is about serving the listeners so they can live, you know, healthier lives with Type One Diabetes. So I only really let people in who I have that experience with. And it's, um, it's just fascinating because you and I really haven't spoken before this, that my vibe of what was going on at your company is is really your goal. And so it's, it's completely obvious, you know, to Oh, absolutely. It's very, very interesting and satisfying for me actually, just a moment like when you were speaking I thought who I was right about this guy, thank god
Paul Edick 33:36
Well, that's good to hear. It's an important part of it. It's critical. I you know, I wouldn't be doing this if I couldn't do that. I, you know, I came out of retirement to do this. And it's about like I said, it's about building a great company that people can be proud of. And in that the word greatness comes from the ability to do everything I just said how
Scott Benner 33:58
did that how does that happen to your retired retired like sitting at home on the patio retired or just in between jobs and not in a hurry to get another one? How, what was the situation?
Paul Edick 34:08
No, two years retired, I was retired, retired, I had been approached about numerous companies and CEO positions and I wasn't terribly interested. Two of my former one of my former investors and another investor that I knew well from the world of healthcare investing, called me, and then they reached out to me through a third party to say please just come talk to us come look at this company. This is little bitty group of people. They've got this cool technology, and it needs a reboot and you know,
Scott Benner 34:43
so as a favor, I I spent some time evaluating what Cirrus was at that time. And so you just sort of came in and consulted a little bit saw the the landscape and we're thinking maybe you'd help them in a certain direction or give him some pointers, but then You ended up staying?
Paul Edick 35:02
Well, no, not not consulting, I just was, I was doing diligence. I was looking at it, you know, to say, Okay, what is the substance of the technology? What can it do? But is it well protected from an intellectual property perspective? Can Can you really build drugs around it. And what I found was, was fascinating, you know, very simple, yet elegant technology in terms of formulating taking old drugs that are not stable in solution, and formulating them into liquid stable products that are way more useful for patients. In many different therapeutic areas. The very first area we're in is the world of diabetes, and, you know, hypoglycemia, but the technology can go in a lot of places. And I saw the opportunity to build a company. There were a lot of people in the Chicagoland area that were, I thought would enjoy coming back together and working together again. So I said in truth be told, I spent about a month as demo three or four months evaluating and then I spent one month building a new plan for the company. And I presented it to the board of directors and said, you know, here's the plan. And here's how much money that's going to take if you're on board with the plan, and you're willing to either put in or allow me to go raise the money necessary. Here's the company we're going to build. And they said, Absolutely. In fact, funny story, I kept saying, well, but we'd need this and we need that we need that. And they kept saying yes, so at a certain point, I couldn't say no.
Unknown Speaker 36:42
Maybe, maybe I can, maybe I could talk them out.
Paul Edick 36:46
If I throw enough stuff in front of them, they slowly fade out. I launched a drug once upon a time called Celebrex. Are you familiar with
Scott Benner 36:54
ever heard of that? Of course.
Paul Edick 36:56
So Celebrex before to bring that drug to market, I think was somewhere on the order of $1.2 billion
Scott Benner 37:05
just to get it out the door
Paul Edick 37:07
before the first capsule was ever sold.
Scott Benner 37:11
So what do you do? You just put it next to beer so that people say
Unknown Speaker 37:18
I wish it was that easy.
Unknown Speaker 37:20
If you Paul's got a brilliant sales plan, if you need glucagon, that's a liquid stable. It'll be at the beer store right next to the Miller.
Scott Benner 37:29
Well, I'm sure you've I'm sure you'll adapt your thoughts. But that's Yeah. Can I ask you What about? Because let me be, like blunt for a second. You guys are making a really boring drug. It's just it's the inside of the diabetes world. It's not something you hear people clamoring about, right? Like it's not. I don't know what I mean. It's not sexy. Like, oh, it's a CGM that tells me which way my budget is moving or great insulin that does. You're talking about something that I think most people think of as that red box, it sits in my drawer, I never use it goes bad. And I throw it away or donate it to my kids school so they can learn how to mix the powder with the liquid like, yeah, and and having heard your life experience. I'm interested in what you saw that in those few months, when you were there looking that made you think this is something that people need, and this will be successful?
Paul Edick 38:22
Yeah, that's a great question. Because most people would look at it and say it's boring. First and foremost. There are five and a half million people in the United States taking insulin every day. The vast majority of them at some point, sometime somehow, sooner or later, are going to have a serious hypoglycemia that requires rescue. I look at that. And I say, Oh my god, the current form factor is almost impossible to use. Only about 20% of those people actually have glucagon when almost all of them should have it. Then you look at it and say over 27,000 people die of severe hyperglycemia every year in this country. totally unnecessary, totally unnecessary. Over 250,000 emergency room hospitalizations for severe hypoglycemia every year. totally unnecessary. And the cost associated with all of that. totally unnecessary. When if you could build a better glucagon, one that is liquid, stable, ready to use, you know, you can keep it in your nightstand, you can keep it you know, in your backpack. It's like if you look at allergies, you know, severe allergies, a fraction of like maybe five to 7000 deaths a year
Scott Benner 39:52
because of epi pens
Paul Edick 39:54
because of the advent of a useful product Right, an epinephrine product that's easy to use, easy to administer, stable at room temperature, etc, you're saving lives. You are reducing costs, you're making it a lot more convenient for people. Why wouldn't you do that? And the thing that's even more interesting, if you look at the diabetes community, the general consensus, the education that's happened, where physicians are saying, well, you should you know, you shouldn't use glucagon to your pass out, which is totally wrong. You should use glucagon before you pass out. You know, people always say, Well, you know, why can't you just use juice boxes and glucose tabs? It's like, yeah, okay, absolutely do all that. When those don't work. When you are at the point of I don't know what's going to happen next. a two step convenient. take the cap off, give yourself a shot to glue gun is a life saving experience. Yep.
Scott Benner 40:55
Paul, I have to tell you from, from my perspective, what you're saying resonates because, you know, I can give you some examples. So my daughter's 15. Now she's had type one diabetes, since she was two, when she was first diagnosed, we got into a situation where we just gave her too much insulin, we didn't know what we were doing yet. She had a full on seizure. She was, you know, incoherent and grunting and, you know, couldn't see and talk and everything. And I and I am, I've told this story a number of times before, it was one of the reasons why it was comfortable having you on because I knew when I told it to you, that people who listened would know that I wasn't just saying this, because you were here, we're laying on the floor, you know, sitting on the floor of my daughter's on the floor, my wife is working on glucose gel trying to get it open, and I'm holding glucagon. And in that moment, I could not for the life of me remember what anyone told me about reconstituting it. I didn't know. And I and I couldn't do it. And we brought her out of the seizure another way because we just couldn't, I couldn't figure it out. And when it was all over, and I had time to reflect on it. What I remembered most is that when someone handed it to me initially, they said, Oh, this is glucagon. It's in case you get incredibly low. It's like a life saving thing. You'll never need it. And as soon as they said that, I guess my brain just went, Oh, we'll never need this. And I just think so much was going on in our life, I did not really have the bandwidth to start learning things I didn't need, you know, and so I just didn't it. It's funny, even when you go to explain it to somebody, you're like, hey, well, you know, you take this. So there's this powder in this vial here. And then there's this liquid in the syringe, you want to take the liquid chute. And as you're doing it, you're like, Oh my God, if this ever happens, this babysitter is not gonna figure this out. And moreover, and probably most importantly, we don't carry it with us. It's not, it's not Yeah, doesn't lend itself to something you keep with you. And and I'm excited for something that does it and and that's, that's what you saw when you went down there that days, you saw you saw the the future of what this could all be.
Paul Edick 43:02
Yeah, and I did quite a bit of research. And I went out, I actually went out and talked to doctors, I went out and talked to patients who were you know, diabetics and said, you know, how do you do this. And I remember my grandmother was a diabetic and I remember my mother giving her shots. And but I, you know, I don't even think I don't even know if there was such an glucagon even existed at that time. But the, I just tried to I went out and listened, and said, Oh, my god, there's a, in my mind at the time, there's a critical need here, there. And, and the, the community doesn't understand that there they could be, there could be something better. For me, it was back to what I said before, an opportunity to change the way medicine is practiced, and opportunity to save lives. And in doing so, the net net is going to be less cost to the system.
Scott Benner 43:57
He said the company's been in existence for how long?
Paul Edick 44:01
Because the company was started by the Chief Scientist as almost, you know, like skunkworks in his back, you know, his, his workshop years ago, like 10 years ago. The company, as it's constituted today, you know, really starting to do serious research and putting products into development, probably about five or six years.
Scott Benner 44:30
The initial scientist, you know what led him or her to work on this.
Paul Edick 44:36
He's our chief scientist today, Steve Petroski. He, he was in a company where he was a formulation chemist, formulation scientist working on different kinds of things. And he you know, one of his areas of interest was products that are not stable in solution or not soluble and he developed Have a an approach chemistry where he can put liquids which are not water based into a formulation, get the water out. And in so doing, you create a much more stable product it can, it can, it's fine at room temperature for like two years. And there's a lot of products that require reconstitution, that, that mixing piece that you're talking about, where you've got a powder, and you've got a liquid and you mix it up, and then you've got the drug that you're going to administer. When that's a water based solution. It usually is not stable when it's in solution. So it degrades very quickly. So, you know, if you could take that kit that you describe and mix it up, and have it in the syringe and carry it around for a couple years. I think you'd find that, you know, a lot more of those five and a half million diabetics would actually have glucagon on hand. I think so too, and and I wouldn't have to be buying them over and over again, as they expired. Right. And, you know, it's interesting, people say, Well, you know, I don't know if I'll use it. And I said, Well, I'll tell you, when people will have severe allergies, my grandson, you know, six epipens. When they when they're expired, they go by six more.
Scott Benner 46:23
Because it's not, it's not the, the constant, you're not going to use it all the time. But it's that one time that you better be prepared for I had somebody the other night, a physician, who said, Well, you know, I've I've only had to use glucagon place in my life. And I was done. I said, so glucagon saved your life twice? Why wouldn't you get one of these better devices? So you have it on your person? It's interesting, fair, interesting, the way they think about it, I completely agree with you. I think it's like, you know, it's like car insurance, almost like you're not planning on hitting somebody. But, you know, the day it happens, you know, for whatever reason, and I talked about it in diabetes that way, as well, as, you know, the idea of, if you could plan for when something was going to go wrong, then it would never go wrong. You know, like if you know,
Paul Edick 47:14
yeah, what you went through as a parent, parents, parents should never have to go through?
Scott Benner 47:21
Well, I have to tell you, it's one of the worst moments of my life like hands down, it really, it's up there in my top 10. I wish these this didn't happen to me, it's experienced that I could have gone my whole existence without having. And I'm even liking the idea that Arden could keep one on her. In the other setup, it doesn't really lend itself like anybody can figure out how to just, you know, push the plunger, but the rest of it is off putting. And then you you also have to keep in mind that that process needs to be simplified, because it's possible that while you a you know, as a bystander, or a friend or a parent is trying to figure this out, there's a person who you know, or love having a seizure, that that could be the situation that that makes thinking a lot harder I can tell you from from experience, you know, you're not you think you're like all comical. I remember afterwards, I said to my wife, like, I think I handled that pretty well. And she's like, oh, you're out of your mind, you don't even know. And I was like, She's like, yeah, you weren't doing well, at all, in case you're wondering, I thought I was you know,
Paul Edick 48:24
it, it is a rare individual. It's a rare individual that is calm in a crisis. I mean, you know, there are very few people that in a crisis, they go to a place that is very calm, very deliberate.
That's not your normal, that's not your average human being. I like
Scott Benner 48:42
the idea of anything that takes away steps or need to think or, you know, possibility of dropping something or that any of all that is better. And I'll tell you why. Not that this isn't incredibly exciting. But as you were speaking, what I really heard was this process that your lead scientists came up with has other applications.
Paul Edick 49:03
Oh, absolutely. We were building better drugs in two or three other therapeutic areas as we speak.
Scott Benner 49:11
It's excellent. That's very cool. Well, I have a ton of questions for you, that are more nuts and bolts, but I think we're out of time, honestly. So either I'm going to get you to come back at some point, or I'm going to have whoever you think is the best person to talk to about the real, you know, the real use strategies behind it. And, and there's part of me that really wants to ask you about closed loop systems, but I'm assuming you're a publicly traded company, you're gonna like shoo away my question. So I'm not asking you about that. Unless you unless you want to talk about it, Paul.
Paul Edick 49:42
We will have the only liquid stable glucagon. So if there's a system that works, we've we've now what you now have not to take too much time but what you now have is the real innovation here is a liquid stable glucagon. You can use it in all kinds of ways. Not just Rescue. So if somebody can perfect a two hormone pump system, it needs glucagon and insulin. Now you finally have the only liquid stable glucagon. So we'll see how the, we'll see how it all evolves. If you're building
Scott Benner 50:17
one of those systems, head over to Chicago, look for the building that says Pringles on it. And that's, that's a little B, can I ask you? And if you can't say I understand, but I'm assuming right now that your FDA clearance for an emergency situation? Are you planning on trying for a therapeutic? Like, you know, instead of injecting the entirety of the dose, if say, I was just in a situation where I had the flu, and my blood sugar was stuck at 50. And it just kind of wouldn't move? And I want to put in a tiny bit of the product, would it? Is there? Are you thinking about that over there?
Paul Edick 50:54
We're testing it in all of those applications. So if you're if you want to exercise, you have to go through an incredible process to not have your glucose go too low. We're in clinical studies on using glucagon our glucagon in small doses before. Exercise. We're studying our glucagon in continuous infusion for people who don't recognize their hypoglycemia symptoms, that you know, that's the classic person who is one minute just fine the next minute in a car accident. You can reboot with continuous infusion of glucagon for about a month, we believe you can reboot the system we're studying in non these are not diabetic, post bariatric surgery, people get severe hyperglycemia after certain kinds of meals. We believe by using a little bit of glucagon after that meal, you can prevent severe hypoglycemia. So we've got a research project going on there. Like I said, with liquid stable glucagon, you can address a multitude of other conditions. And like you said, you know, what is mini dosing? How does that work? Can you? Can you give yourself a little bit of good gun for different things? We're studying it. We have four clinical programs ongoing right now. That's,
Scott Benner 52:21
that's very encouraging. That's excellent. Yeah. You know what the one thing I didn't ask you, it's so funny, who named the company and how do you guys say it
Paul Edick 52:30
different people in the company say different ways. Some people say seris, and some say Cirrus, the original name was by the Chief Scientist using a similar rationale to Xerox, which was dry printing is not really dry can still a liquid, but it's without water. So his, he said, you know, serious is for dry drugs like xeriscaping, etc. So that's where he came. That's where he came up with it.
Scott Benner 53:03
I'm never in favor of letting the really smart people do the creative stuff, but I hear what you're saying.
Paul Edick 53:09
You never let a scientist name the company, but it was already done.
Scott Benner 53:13
You know, it's and what's the name of the G, Volk, g Volk,
Paul Edick 53:18
glucagon evoke, it evokes your
Scott Benner 53:21
your glucagon from your liver. Now see, now we had a marketing person involved. I see. There we go. I would ask you more about it. But it's it's fascinating. I don't think people understand either that the FDA has really strict rules on it. But you can even name drugs and drug names go through a lot of so they can't be confused with something else. And like there's a lot that goes on that I think nobody really hears. Paul, I really genuinely appreciate you doing this. Thank you so much for coming on. Thank you. In a few months, we're gonna have someone back on to talk a little more about evoke more of the nuts and bolts about how it works, the science of it and the use. But for now, I just thought it was interesting to hear from Paul and find out how the leadership of a company that brought you the world's first liquid stable glue gun thought and how they got to that thinking. And moreover, I think Paul was just an interesting guest. We don't often get to talk. Those people like this right really break down who they are and where they came from. Ge voke is a prescription medicine used to treat very low blood sugar in kids and adults with diabetes ah two years and above. g voke. is the first ever liquid glucagon it is premix prefilled. Pre measured and ready to use, no refrigeration is needed. g voke has been approved in two formats, a prefilled syringe and an auto injector visit Jeeva glucagon.com forward slash juicebox to learn more
Please support the sponsors when you’re able and it makes sense for you. This episode was sponsored by Gvoke.
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#174 InPen is Like Other Pens, but Smarter
click image to enlarge
The smarts of a pump in a pen...
Mike Mensinger (formerly of Dexcom) is back to tell us about his smart insulin pen from Companion Medical called InPen. Type 1 diabetes with multiple daily injections just got better.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - google play/android - iheart radio - or their favorite podcast app.
You can also listen on Companion Medical's media page.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello, and welcome to Episode 174 of the Juicebox Podcast. Today's episode is with Mike Menninger. Mike was once a longtime employee of Dexcom. But he has gone on his own to develop a smart pen CMD I users, I got you covered.
Please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise Always consult a physician before making changes to your health care plan.
Mike Mensinger 0:50
Hi, Scott. I'm Mike Mensinger, Chief Technology Officer at companion medical. Great to talk to again,
Scott Benner 0:57
I appreciate you coming back on now with a different company though.
Mike Mensinger 1:00
Yeah, the left x com about a year and a half ago. And when what an amazing journey that was with dexcom share, and z five. And it was a such a privilege to be part of all of that transformation and in diabetes technology and happy to do it again, in injection therapy. Now,
Scott Benner 1:18
it's pretty exciting. So how long were you at Dexcom
Mike Mensinger 1:21
13 and a half years. So started in 2003. And my co founder, Sean st is the CEO, he actually built the first Dexcom short term sensor in 2004. So we have a lot of early Dexcom heritage here.
Scott Benner 1:35
And so now you and Shawn are on a different path trying something different.
Mike Mensinger 1:40
Yeah, the you know, while the technology was really amazing, and that was really great to be part of everything we did at Dexcom, we were frustrated at the lack of technology that was directed towards the injection market. So there's so many great solutions today, that's available for insulin pump users. It's very exciting to see but comparatively nothing available today for injection users,
Scott Benner 2:02
it really did feel like it does feel like honestly, that people using pumps have access to so much more data and technology. And I don't I don't know if it's a left behind situation or where it was headed. But it really did feel like there was a chasm growing between people who wanted to do MDI, and people who wanted to pump and the people who were pumping, we're getting a lot more, but you think you've fixed that, don't you?
Mike Mensinger 2:28
That's what we hope. So we've brought a lot of the benefits of pumps to syringe users. And we can get into that. But you know, things like the dose calculator, automatic dose tracking those reminders, helping you manage your long acting insulins. So complete solutions that's right there on your phone and easy to use.
Scott Benner 2:45
Okay, so let's, uh, I guess we'll go back to the beginning. Did Shawn start companion medical? Or did you or who, who had the first thought and who came along?
Mike Mensinger 2:57
Yeah, we I think we fight over that a little bit. But we had the idea around the same time from two different vantage points. So he was a tandem running advanced technology. And he says that he was trying to, he was frustrated with how to bring the benefit of insulin pumps, this great technology to really the larger set of users with diabetes. But as you know, it's only about 30 to 40% of folks in type one using some pumps, and much fewer than that it's about 7% worldwide when you look at injection, therapy for insulin in total. And so he was trying to say, Well, why aren't more people buying this product? But then he had an epiphany and said, Well, maybe we're asking the wrong question. How do we bring those benefits to the folks that don't want to use an insulin pump or can't afford it. And so that's where he came at the problem. And I came at it from a slightly different avenue, inside Dexcom, we're trying to really have the best overall solution and without influence data, which we had with our pump integrations, but without for the larger market, you know, you're really limited in terms of what you can do as a solution. And so, you know, we were looking into why isn't anybody doing this? And that's how we both came to the idea around the same time. Nice. And then he was able to actually leave tandem, and start the company. But I stayed at Dexcom for three years.
Scott Benner 4:19
build up your war chest so you could get going, right?
Mike Mensinger 4:22
Well, again, there's so many exciting things happening g five and share and you know, these really great advancements within diabetes. That was, you know, I wanted to be part of those. And that was very fortunate to be able to do that why Shawn started the company.
Scott Benner 4:35
No, it shouldn't be, it shouldn't be overlooked. what you were doing there was, um, you know, and what they continue to do with Dexcom is amazing, but I think you might have, I think you might have the answer here for people who aren't using pumps. And and that's why I was excited that you guys could come on and talk about this. So I get a lot of correspondence from people who say, you know, I listen to the podcast and I want to do these things. But I don't have a pump. And you know, we've had people who listen, no, we've had many different people come on, and we talk about MDI all the time. And what we came up with was, besides not having the ability to manipulate your, your, your slow acting insulin, when you're when you're an objective when you're doing injections. Besides that, if you're willing to inject, you can make as many adjustments to your blood sugar. As people can who are pumping, you don't have, you know, you can't, obviously, your lever mirror your lantis, or whatever your slow acting is, that you're not in control of, but everything else. If you had the data, you could, you could control. And now you're you have a way to show people, everything that's sort of going on in their body with their insulin. And, and so I want to start talking about it. So I'm excited here. Right? Yeah, yeah. So you start you so you have a product called in pen. Is that that that's what I call its intent. Okay,
Mike Mensinger 5:59
that's, yep, that's the product name. Yep. And it's iOS available since December on iOS. And we just got Android approval, actually, last Friday. That's amazing.
Scott Benner 6:09
Thank you questions, and you are FDA approved?
Mike Mensinger 6:12
Yes, we got FDA clearance, actually about a year and a half ago.
Scott Benner 6:16
So what we're looking at here in its simplest idea is it's a insolent pen, but it's a smart pen. And it's speaking to an app that people use on their Android or their iPhone, or their iPhone. And what is that app, giving me? What kind of information comes from that?
Mike Mensinger 6:34
Sure. So just like an insulin pump, you have a complete history of all of the injections. And you know, when you took insulin and how much we calculate your insulin on board for you. So you can know how much is still in your body, that's going to continue to lower your blood sugar over the next five hours or so. And that needs to be factored in, as you know, for for future injections. We have a dose calculator, just like an insulin pump. And you can input your blood sugar, and your carbohydrates and subtract out your insulin on board. We also have dose reminders. So if you forget to take, say, your breakfast dose, it'll be at nine o'clock, or whenever you configure it for it'll, it'll remind you and say, hey, maybe you miss breakfast, but maybe you forgot your dosed. Figure that out, it has solutions to help you manage your long acting insulin. And remember to take that. Let's see here, the pen itself. A couple of unexplained reasons for hyperglycemia are sometimes if you leave your pen in your trunk of your car in the summer, or in the wintertime, and it goes, it's too hot or too cold, your insulin reduces effectiveness. So the pen has automatic temperature tracking. And we'll let you know if you should consider replacing your insulin. And similarly for age, if your insulin gets too old, it's been in there too long, it'll let you know it's been been longer than 28 days, consider replacing that, wow.
Scott Benner 7:56
Okay, so let's pick through that a little bit. Because that was a lot. And I'm going to start at the end, I'll start where you finished and go backwards. So the pen knows, I guess when I put in a new cartridge, and then it starts kind of a countdown for how long it's been in there.
Mike Mensinger 8:11
Yes, exactly. So when you load a cartridge into the pen, you do this every three days or whatever, how long the cartridge last few bits automatically knows that you've put a new cartridge in, and it starts that timer for you. And then 28 days later, if you haven't put a new cartridge in, you'll get a reminder on your home screen in the app saying your influent is a little bit old, consider replacing it.
Scott Benner 8:31
Okay, now that seems obvious, but how does it know what the temperature is?
Mike Mensinger 8:36
So we have temperature trackers on the tent itself. So if you leave in the car, it knows how it seen and it's sampling the temperature, you know, periodically on the pen, and it will let you know it's it seemed this maximum temperature for this length. So you can make a decision yourself whether you want to continue to use the insolent or, or replace it at that time.
Scott Benner 8:55
Like that's impressive because I'm I have the pen here I have a demo of it. And it's not any larger than any other insulin pen I've ever seen. Actually, it looks a little it's it's a little smaller. I think if if I'm right then some of the other ones that I've held. So you've How did you get all right, listen, I guess you can't tell me how you got that in there. But that's pretty cool. Yeah, thank you. Yeah, absolutely. That that is really it's simple. When you stop and think about insurance, you tell me that but I'm assuming that the you know that the work that goes into figuring out how to get that in there and get you good information is probably probably pretty intense. So on the app if I want to say look, I you know, on the days I forget my mealtime insulin. I usually remember around nine o'clock that I forgotten so I can just set up something that does just pop up and say have you taken your insulin or does it alarm or can it do either?
Mike Mensinger 9:47
Yeah, you get a notification, just like Dexcom high alert or low alert. Yeah, it's, it's not going to make the kind of loud sound but a Dexcom alarm would, but it's more of a friendly reminder that if you If it senior breakfast dose, you're not going to see that there won't be any extra steps for you. But if it hasn't seen a dose in that configured time range, it'll, it'll let you know.
Scott Benner 10:09
Oh, so that's actually even more impressive than what I was thinking. So in that time range that you tell it, this is when I eat normally, if it hasn't seen you give insulin, it tells you. Exactly. So I'm not just setting a timer that says, hey, randomly at 10am remind me have I taken my insulin today?
Mike Mensinger 10:26
Yeah, so one of our overall design philosophies, and you'll kind of see this throughout the product is, diabetes is very hard as we know, we don't want to make diabetes extra work. So let's keep it simple. Let's keep it intuitive. And if you don't have to notify you, or make you spend more time on it, get back to life and live it. And that's, that's how we designed the MS DOS reminders.
Scott Benner 10:47
It's really something that Shawn has type one, is that correct?
Mike Mensinger 10:51
Yes. He was actually diagnosed when he was attending, believe it or not. So he was able to get a TGM from Dexcom, the same day of his diagnosis, and he's never lived the day with diabetes without
Scott Benner 11:05
jamjam. Wow. So he was working in the diabetes space, but did not have type one and then developed and while he was there,
Mike Mensinger 11:14
yeah, I'm pretty late in life. So it's very unusual. It really is crazy. I have to
Scott Benner 11:17
talk to him someday. Okay, so what else was I just looking at. So you have integration. This is one of the things I want to make sure I understand correctly integration between my CGM or my, my bluetooth meter data. So I can see my Dexcom information and my information from my in pen in your app. Yes, and though run through how. So that's done through Apple Health and iOS. So Dexcom writes all of the data, it does have a three hour delay on it, but it writes it all Apple Health. And as long as the user gets permission for our app to read that data, it's automatically flowing from the Dexcom system into our system. So if you look at our log book, you'll be able to see not just CGM data, but you can see CGM with your insulin and your carbohydrate intake. And you can see the cause and effect of how they affect each other. You can go back 90 days in our logbook of your CGM with insulin and carbohydrates, and really be able to see to really be able to tell Look, I put the insulin in here. I started eating here. And then you know, now I'm moving away from what I did with the with the pen. And now I'm seeing on my Dexcom graph, here's where my blood sugar went to. And that's when you can start making decisions about maybe my Pre-Bolus could have been, you know, it's funny, there's no there's no word for Pre-Bolus sing with MDI, we'll have to make one up sometime. But pre injecting is sounds a little clunky. But so your Pre-Bolus you know, maybe I needed a little longer, maybe I could have used more insulin, like there's ways to make those fine tune adjustments that the people who listen to this podcast or are familiar with, because you can see these data points held up against each other.
Mike Mensinger 12:53
Yeah, absolutely. Excellent. So on the we also have a report insights by intent, which is right, it's kind of like the dexcom clarity, but it has a you get to see your insulin, and your carbohydrates with your CGM data is the Dexcom user. And you can see the timing of your insulin. And you can see how insulin is stacking on top of each other, because we graph it as your insulin on board. So you see the insulin and how it's acting and actually affecting glucose over time, which is a really great tool for your doctor. But also, if you have a child, you can look at cause and effects and use teachable moments to help them understand the effects of insulin on blood sugar.
Unknown Speaker 13:30
Wow, okay. Wow, that's a lot.
Unknown Speaker 13:34
But yes, there's more, Mike.
Scott Benner 13:36
This episode of The Juicebox Podcast is sponsored by companion medical makers of the in pen. In pen is the only FDA cleared smart pen paired with an integrated diabetes management app, the smarts of a pump in a pen, you get it right, in a pen in pen, the smarts of a pump in a pen. I mean, it's not complicated wordplay. I'm assuming you're getting it, you can find out more at companion medical comm where the links in your show notes are at Juicebox podcast.com. For if you don't want to be you know, all held up with that old timey internet stuff. You just go into the App Store, download the pen app, check it out, and then just push the button and be like, hey, button. I want to get this pen. Listen, I understand that you don't think you talked to the button? It was? I don't know. I don't know why I said that. Push the button. Really. You go in the app and you push the button. And we're off the rails here people. You just go into the app, you push the button and the process begins. It's very simple. Mike's gonna explain later how the insurance process works. But it seems like they've got all their bases covered. He said that some people get their answer back in just a day. And depending on your insurance, you might be really surprised at how low the cost out of pocket is. But we're getting ahead of ourselves. You need to find out more about the in pen before you make your decision. I get that. Mike and I are going to go over everything. It does in this next 30 or 40 minutes, and how you can get it if it's something you're interested in. But let me just say there's a lot more coming. There's integration with CGM and meter data. And it can remind you that you didn't take an injection. Now, maybe you find out how it does that. This pen is smart. Oh, I get it. Now. That's why they say hello, I got a run down the smarts of a pump and a pen. It all makes sense. I'm trying to wrap my head around. I haven't done injections in such a long time. That as you were talking, I just thought okay, so now insulin on board is in sort of one graph, but so is my Bolus, and I can see how they kind of overlap. So instead of having to imagine, I know there's insulin on board, but how much I can, I can see that visually, which I find, I find really amazing now, but let me ask you this question. Have you done it in a way? That's not? I look at it and go, Oh, there's so much here. I can't understand at all? Like, is it simple? Is it intuitive? When I look at
Mike Mensinger 16:00
it? When you tell me, we sent you an example report. So does that make sense to you? Well, Mike, I
Scott Benner 16:06
was opening you up to say nice things about your pen, but no, it does. It's very easy on your I guess as a way to say it, I don't look at the information that I'm seeing and feel like I don't know where to start looking. Or it doesn't make any sense to me. It's done in a really kind of simple and, you know, pleasing way in a way that I can I feel like I'm in. I feel like I'm in a space that I understand what I'm looking at. So so I think you've done a really good job. And you were very time not to take the bait. Just say something nice about the fine, that's fine, Mike. Let's see what some of this other stuff is. Because I don't I don't know that I understand it. We have some like thoughts here. And you and I have notes that I'm looking at, but like, how much insulin Do I need for a meal, it's going to tell me that based on what my carb count is. Okay, so
Mike Mensinger 16:57
I'll steal your phrase, it's about taking the right amount of insulin at the right time. So your bolus calculator just like an insulin pump will take your current blood sugar level, it'll calculate your correction of, say, 200. How much insulin Do I need to get back to my target of 100. And then it'll take how many carbs are about to eat, and figure out how many carbohydrates? How much insulin Do I need to cover those carbohydrates, and then subtract any insulin you still have in your body from prior injections with your insulin on board. And it's very similar to what pumps do. Not much of difference, the only difference that we do have. And this is similar to I think the Cosmo pump. So if you actually if you go to calculate a correction, and let's say you have a lot of insulin on board, if the correct action for the user is to eat carbohydrates, because that iob will bring you below target, it'll recommend the right amount of carbohydrates to eat to get you back to target.
Scott Benner 17:54
Oh, that's fantastic. So when we talk on the podcast about bumping and nudging insulin, we also talked about bumping in lodging food. And and the big problem that people come into is they run into that, you know, that old adage like 15 carbs, 15 minutes, if you think you're low or you're low, eat 15 carbs, wait 15 minutes test again, that kind of an idea, those 15 carbs can often be much too much, which sets us off on the roller coaster for the day. And so this is going to tell me no, you don't need 15 carbs, you should try more like this.
Mike Mensinger 18:26
Exactly. Yeah. So based on your current blood sugar level and your iob, it'll figure out how much to overcome the iob and your blood sugar to get back to target. So in certain circumstances, let's say you're very low, you're 50. And you have iob, you may need more than 15 grams of carbs to return to target. Right. So there's less guessing here, it'll it'll give you a more precise answer of how much to eat. And it gives you an opportunity to correct without overcorrecting,
Scott Benner 18:53
which is Yeah, exactly such a huge thing, because then your whole day becomes about chasing those lines around. Let me ask you a question. So we'll jump around a little bit here. What kind of insulin Can I use in the pen?
Mike Mensinger 19:08
So we take cartridges from novolog, or human log, and you get a separate prescription from those, instead of getting it in vials, like you normally would you get those cartridges, a cartridge, so there's nothing for me to fill or anything like that,
Scott Benner 19:19
I pop it out, I
Mike Mensinger 19:20
put it in the pen and I'm on my way. Exactly no selling, you just load it in there and begin using it and then change it out.
Scott Benner 19:27
So now you and I spoke recently about this and you were talking about there's just one aspect that I don't follow completely because I have been pumping in a while. But when people use a pen, the pen gets primed. And so I decided I want to use I don't know six units, and I dial it up but then the pen expresses some of the insulin to remove air from from the system. And then I don't quite get my six units. Is that what happens with most pens?
Mike Mensinger 19:53
Yeah, so you're supposed to change your needle for every injection. We know a lot of users don't do that. But even if you don't do that there Maybe an air bubble or some dead space in the needle that needs to be filled up before it actually gives you influence. And the action of priming is just to fill the needle out to get a drop of insulin out the bottom. This is something many injection users know how to do. But when it comes to smart therapies, like a, like a smart pen, we haven't seen the challenges with that on the system. So for instance, if you inject if you expose two units of insulin to fill the needle, and then you give yourself a small correction, like one unit, most systems if they can't tell the difference between those two, what you injected, and what was actually just filling the needle and priming, would think you've injected three units. And that was, you know, that would mean your iob is three units when it should be one, and your dose calculator is going to give you the wrong answer. So priming, and differentiating what was a therapy dose, and what was a prime dose is something that we do automatically for you, it's a very important feature to have accuracy of your data, so that your tools like your dose calculator can be counted on and
Scott Benner 21:01
stuff like that, you guys just sit down at some point and say to yourself, What is wrong with how people inject and let's hear all the complaints and all the things that that John's experience and everybody else and just like reverse engineering was that how the process began for you guys.
Mike Mensinger 21:19
A lot of its evolutionary, some of the problems you kind of learned as you're putting the pieces together, and then you begin trying the system out and you discover the problems with it. And then you have to go solve those. You know, as one example, the we did a beta use last summer about a year ago. And some of our users came from pump therapy. And they said, You know, I love the product, but I'm always forgetting to take my long acting insulin, because with a pump, I have an automatic basal rate, I don't have to worry about it. There's no meal event to go along with it. So you know, they're going to bed and either forgetting it completely, or like waking up again, and going remembering to eject like, I really need a reminder for this thing. We're like, great, this is a common problem, let's go add the reminder. So now you can just pre configure your long acting amount, you get a notification, and you don't even have to unlock the phone, you can just say, Hey, I log my 18 units of Atlantis, right on the home screen of your phone without unlocking it. It's very simple, very effective. And we're trying to as we uncover those solutions, we're trying to create very graceful solutions to those problems.
Scott Benner 22:23
And I appreciate that, because it's, I mean, there's no shortage of different apps around diabetes. And a lot of them come to me people like, hey, look at this app, you know, and I look at it, I go, Ah, it's just there's so many steps or just, I think that people miss what you and I were just talking about where you're speaking about at the very beginning, which is that these things aren't intuitive, which is an overused word, but simple, like, really just don't take much of your time or your effort or your computing cycles, you know, if it doesn't do that, then what I'm getting isn't worth what I'm putting in. And, and that is a huge problem, because there are a lot of great ideas that are just implemented. Not quite right. And it really feels like you guys thought this through in a way that eliminates that feeling of Gosh, I'm spending too much time in this app doing these things. I just it's very, it's very impressive, because I like I said, I've, I've seen it over and over again, there are plenty of apps where I look at them, I go, yeah, I can't get behind this. So it's like I What am I gonna tell people, you know, they need to spend an hour a day in this app in order to get their agency down. Like, no one's gonna do that. You know? So really well, and you have a small you guys have a small group of that you don't have any employees? Are you at this point?
Mike Mensinger 23:40
We're about the size of Dexcom was when I joined in 2003. So we have about 30 people now. But definitely growing but that includes our manufacturing in house personnel and our sales team. So it's really something Yeah, pretty pretty small company.
Scott Benner 23:55
Yeah. So okay, but you guys have all the you have all the bases covered. It's a small in size but but big in in theory and grander. Honestly, how do I? How do I make the decision, right? Like I tell people all the time, if you want to try an insulin pump, and you want to try the only pot, here's the steps to go try it, but again, on the pod has made it simple for people to go try it. Have you made it simple for people to try the pen.
Mike Mensinger 24:19
Yeah, good, quick story. So when we're at Dexcom, and other products like insulin pumps, it can be very difficult. Sometimes you have to call them get their insurance insurance won't approve you right away, you have to get a prior off and get your doctor to kind of build evidence to get coverage of the product. And we wanted to make this very simple, and kind of a modern, almost in app purchase type experience. So what we did is we tried to get rid of all the hardships for users like obtaining a prescription and running your insurance and figuring that out. And one of the benefits we have is we're not a you know, five $6,000 device like some insulin pumps. This is a very cost effective therapy. So we're able to do this a little bit easier than insulin pumps can sometimes. But we built a flow in the app where you can go to the website, or you can download the app. And there's a get in pen flow. And all you do is you fill in your contact information, you take a picture of your insurance card and hit send. And then what happens on the back end is we will run your insurance for you figure out how much your copay is, we'll obtain your prescription from your doctor. And then you get a call back saying, hey, the intent is you know, your copay is $20. Would you like to move forward? If yes, take the payment over the phone and ship the pen right to you. So it's very simple. And a lot of times that happens same day. So very, very simple.
Scott Benner 25:41
It's crazy, how I'm what's the life of the pen? Like because it's doing things right? It must have a power source, how long do I get to use the pen?
Mike Mensinger 25:49
That's a one year pen. There's no recharging needed. So it has a battery that supports the full year in it. And then you just get another prescription a year later for the next 10.
Scott Benner 25:59
Okay, well, that's simple. Okay, so let's, let's talk about this real quick. So I go into the app. And before, listen, let's ask like this question before people commit to get in the pen, they can still look around the app and decide what they what they see there. Is that correct?
Mike Mensinger 26:15
Absolutely, you can go download the app today play with most of the features. The only features that you can't get access to, obviously, is communication with the pen. The insulin settings and your dose calculator and iob are prescription features that FDA wanted us to verify the prescription for, and how we do that, rather than unlock codes that some beaters have had with Bolus calculators, you're pairing your intent to your phone is your prescription. So just the act of pairing unlocks those features for you automatically. There's no complex codes are anything to deal with there. Okay. So you can do everything but that you can log into and manually, you can use a long acting reminder, you can do your MS DOS reminders, a lot of the benefits and features, you get the CGM integration, the BGM integration, all that comes for free. So go try it out.
Scott Benner 27:05
So we check out check out the app, I decided I want to take the next step. I just hit that the button in there that says listen, let's keep going. And and then you guys take care of it on the other end. I am that's really something. Okay, so now, so let's talk directly to the people here. So I always feel like I'm not doing enough for the MDI listeners. And I get a lot of notes like and I always feel like I'm not doing quite enough because the you know, because the podcast is, from my perspective, it's what works for us what I can, but I can step up and say, you know, is something tried and true for me. So I want to tell people the reason Mike came on, if you have been listening for a really long time, Mike's been on the podcast already back when he worked at Dexcom and has an incredible track record of helping people with type one diabetes, to get their insulin, understand how it's working. It's a it seems to be like for me, it seems that you are you're in for urine for more than a pound with diabetes. So I was I was I was wondering, how did it start for you? Like, how did you get to DAX common initially? And how did you get into this world?
Mike Mensinger 28:11
Yeah, it was a little bit of a coincidence. I was just kind of very fortunate that it worked out this way. But I graduated college on the east coast and just wanted to move to California. So I got a job in Silicon Valley area worked in some really cool industrial automation technology. But then the.com bubble happened, dating myself a little bit here. And the whole market crashed, that industry was doing very poorly. And I wanted to move to an industry that was flourishing a little bit more. And I got all of my friends that left for startups at the time, were now looking for jobs, because they all these startups dried up, but as a different industry. And so little company called Dexcom called me, that was a startup. And I didn't really want to join a startup at the time, because, you know, I thought those were too risky. But they said no, no, it's medical. It's different. And it was down in San Diego. And so I agreed to come down and interview and I met the most amazing collection of people down there. And if you can judge a company's future success by the people they have, you know, it was a really good bet. So I took the risk, and joined an amazing collection of people. And it's just been obviously, the story of Exxon has been absolutely amazing. And they have a lot of those people. They're still today from those days. So, yeah, I kind of lucked into it, to be honest.
Scott Benner 29:30
Can I ask, have you had the experience that you hear a lot of people talk about with and I'm asking you a question you didn't know, I was gonna ask you. But I think that when you meet people who live with diabetes, and you hear their stories, it has an impact that is difficult to you can't falsify it. Do you mean like the the impact that you get from that is, did you have a lot of contact with with users at Dexcom? And do you now within Penn, do you talk to the people who are using the products?
Mike Mensinger 29:59
Yeah, I mean, that's a That's one of my absolute favorite things to do is to go to the shows to talk to folks on the phone who are using the product. And, you know, we're You and I are both extremely lucky to be able to work in an area where there's such a huge need. And you're really impacting people's lives in a major way day to day, and you're doing it through your podcast we do through technology. So, you know, everybody that works here, just loves coming to work every day and know that they make a big impact in the world. And how many people can say that in their daily lives, there's a lot of great jobs out there. But you know, we all feel like we're just in the luckiest of positions to be able to do this.
Scott Benner 30:37
I completely agree. I think there's nothing better than seeing someone start at one level get to another or be struggling and then not struggling or to even help somebody, you know, this, this episode is going to go up this week, and it'll go up with another one. Right? So this is Episode 174, there'll be Episode 175. And that episode is with a person who is just they're afraid of their insulin, they're doing their best, but they just can't kind of conquer that fear. And, you know, interviewed that person, now we've gone back, I keep in touch with Brittany, and we're trying to, you know, I'm trying to help her work through it. And it's, you know, it's just finding friends, it's just finding someone else out there who understands, and seeing the value in that. And, and, you know, I this is might be a leap, and I hope it's not. But like I said, in the very beginning, when I started talking, I always feel like we're not quite doing enough for the people who inject. And I have a lot of hope and a lot of excitement around impairment and what you guys are trying to do, I really feel like there's an opportunity to take those people and kind of like in one fell swoop just yank them up into the same kind of tech world that everybody else gets to live in with their pumps.
Mike Mensinger 31:49
Yeah, thank you. That's exactly why we're here. And there's some other great technology coming now. The world I think is catching up to, to be able to give solutions to the users who don't want to pump. And it's great to see is it's a really big need.
Scott Benner 32:03
Well, let's talk for a second about what people are going to find when they decide they want to they want to try the pen. are most of them going to get a good response back from their insurance companies. What have you been saying? Okay, we're more than halfway through our conversation with Mike talking about in pen today, you must be, at this point, starting to get the vibe that this is something you're interested in finding out more about. I've made it completely simple for you to do that. There are links in the show notes of your podcast that there are links at Juicebox podcast.com. For this episode, there are links, there are links, there are links, there are links, you might click to the key click on and the next thing you know, everything is clear, you can do it. It's not hard. It's not hard to do better for yourself. If you're using MDI, now, this is an opportunity for you to get almost all of the technological. But it's is the word I one benefit. That's a good word. Almost all of the technological benefits that pumping brings you. You know what? Sure you can't manipulate your temp basals. But that's, you know, that's the world you live in with MDI. It's not the worst thing in the world. Can you imagine having all this other information to make these great decisions with you listen to this podcast all the time, and you hear about the return of data, and how we can turn that data into better decisions, better outcomes, less spikes, less lows, this is what you want, if you're using MDI, in pen is worth a look. companion medical comm links in your show notes links at Juicebox podcast.com. Or just go to the app store right now download the app, check it out, and then right through the app, you can apply to get the patent. It's super simple. The embed app is currently available for iOS, that's your Apple products. If you're listening in the summer of 2018, it has just been cleared by the FDA for Android phones. So give companion medical, you know a little bit of time to get it into the Android store for you. are most of them going to get a good response back from their insurance companies? What have you been saying?
Mike Mensinger 34:24
Yeah, so right now and you know, the normal process of a new category of product introducing into the market is you have to go to every company, one by one, you go to the blue Cross's and the kaisers and get knows of the world and tell them about the product and convince them of the benefits. But we've been very fortunate, largely due to our low price point. So compared to other insulin therapies, this is very affordable. So we've had very good coverage right out of the gate. So a lot of I would say about 70% of our users are getting covered at some level. It's pharmacy benefit, so on Like insulin pumps, which are kind of a different channel. Usually it's whatever your copay is based on your your individual medical benefit or your pharmacy benefit design. So it may be $20, or maybe $50, and maybe zero dollars. That totally depends on your plan. But we're seeing, you know, we had someone the other day that filled out to get in pen flow at the diabetes conference in Orlando, they had a call back same day and their copay was $5. So it's, we've had some really, really good experiences with getting getting folks covered. And we're working with the insurance companies to get that better every day.
Scott Benner 35:35
Do you have a mechanism? If somebody should find that they're not covered at all? Do you have a mechanism for an out of pocket cost?
Mike Mensinger 35:41
Yeah, absolutely. So if if you get that we will work with you, we have some programs in place to make that affordable. We don't want anybody who wants this product not to be able to get it. So just give us a call directly at companion. And we'll work through that with him. Okay,
Scott Benner 35:55
so I'll put links in the show notes to all this so people can find it. And there'll be links back at Juicebox podcast.com. And I'll give, I'll give you guys everything, how to get the companion medical, how to find the apps, all that kind of stuff. So when I have now I've done this, right, I've got the pen, it's tracking my data, I'm hooked up with my Dexcom data. I'm not through, you know, through my healthcare. What am I going to be? How do I go about taking that to my healthcare provider when it's time for my endo appointment? What do I have to bring with me or do?
Mike Mensinger 36:27
Yeah, the Yeah, the MDI. Users have traditionally had these log books. If you're lucky enough to have a CGM, you can bring your CGM report, but you haven't had any source of integrated data. So we just released prior to Ada being in June, our insights by intent report, which is kind of our version of clarity, or you know, any of the other reports out there, but we did, as we mentioned, integrate insulin insulin on board, you can see the effect of every day and every decision that you made. And that made it very easy to share. So, given the mobile technology, it's not a separate app, it's right there as a tab on your main app. And when you want to share it with your healthcare provider, you can email it, you can message it, you can fax it directly in the app to your doctor. So it's extremely easy to print share directly from your phone,
Scott Benner 37:17
okay. And then the other one, which is something that happens to me a lot in the in the office is I just hand my phone to the doctor,
Mike Mensinger 37:25
or you can print ahead of time and
Scott Benner 37:27
just here just swipe through this and look real quick. But know that that's listen to one of the main things you hear people kind of wringing their hands over as their endo appointments come as I haven't put this information together, I you know, I have to write out logs, and I have to find everything. And then I think they just end up not doing it. And and then it's a shame because it's an opportunity missed. You're going into the endocrinologist, now's your time to ask your questions. And wouldn't it be great if you could lay the information out the simple way that the endo could follow that you could point and say here, look, I did this here. And this happened? And what do you think, you know, should I try something different? And so you guys have made that easy, too?
Mike Mensinger 38:07
Yeah, I mean, who has time for manual logbooks, just no one does this, if you know most of them are filled out the day before if you do have a logbook, but you know, your doctor is only as good as the data they have. So if you have some, if you have a CGM alone report, which is fantastic. And you have some hyperglycemia, you know, what's the cause of that? Did you forget to take your insulin? Or did you underestimate the carbs in that meal, are your bolus calculator parameters wrong and need to be adjusted, there's many, many causes there, or maybe your temperature of insulin was went out of range, and your insulin is less effective. So the more tools and getting to the root cause of those problems, that report can help your provider with, you know, the more actionable data they can use to make better therapy adjustments with you.
Scott Benner 38:52
Yeah, for sure. The idea that, you know, I talk a lot about people, people, sometimes they have a, you know, some sort of anomaly with their blood sugar, right. And instead of doing something about it, they spend a lot of time wondering what happened. And I tried to kind of coach them through the idea of like, in the moment, it's not important what happened, just take care of it, think about it later. But what you're able to do with just little things, like, you know, seeing on a graph when the insulin went in, or knowing that the insulin got too warm or too cold, is you're removing, when those anomalies happen, your your what your your apps doing is it's removing possibilities like it Well, it wasn't this, like I know the insulin didn't get out of temperature, so I can eliminate that. And when you could eliminate things from that thought process from that. It becomes more streamlined and you can get to your answer a little quicker to an absolutely yeah. And I like the idea of not having people in a situation where they have to unnecessarily wonder about things because I think it adds anxiety because you can't really know about some stuff, right? You just sit there and kind of just turn over and go well, maybe it was this. Maybe I do. didn't do that. And the more of those things that can be removed from your thought process, I think I think the better. Yep. I totally agree. That's excellent. Okay. Okay, so I've gone to my doctor, you know, they've made some great adjustments for me. And I come home and I try stuff. And I come back, I look at my data again. And I see, I did this. And we always talked about that, you know, kind of this. I don't know what to call it even. But it's a process, right? I did this, I expect this to happen. Instead that happen. So next time, next time, I'll try sooner, more, a combination of sooner and more longer. Whatever. It's, it's right there for everybody. So everybody who's been listening, who uses MDI, and is always wondering, like, how do I get what, you know, what I'm hearing these other people talk about, and this, this is an incredible leap for you. You know, Mike, we talked about it here, because it's, you know, I think it needs to be spoken about. So people understand, we're talking about, but at this point now, with a pump, and index calm, my daughter's a one has been between five, six and six, two for over four years. Amazing. It's It's spectacular. But it's because of it's because of technology, right? I can't trust me, I know who I was before. pumping. I know who I was before. Dexcom. I know who I was, before getting that information that I needed to make better decisions. And I think that when I hear people with MDI talking, what they're saying is, I can only get so much done with injections, because I lack the rest of these things. And it sounds to me like for, but somewhere between five and $50, I get a pen that works for a year, and gives me everything that I need. Does that sound about like what you guys are shooting for?
Mike Mensinger 41:45
That's exactly what we're trying? And then, you know, we we don't think we're done. We have a lot of, there's still a lot of low hanging fruit, that we'd love to hit everything from hydration, you know, can the system help you determine? You know, if you're only going back into your healthcare provider, making big adjustments every three months? You know, can we help your healthcare provider do that at a faster interval to get you into the right range and personalize your bowls, calculator settings. You know, androids coming out, we're looking at Europe and other markets that should be coming out later this year, or maybe next year. solutions for exercise, because as you know, exercise is a big challenge with diabetes. So the one great thing about Android and iOS devices is they track your steps and fitness thing. So can we look at the history of you walked a lot today, or you exercise a lot. And therefore, you know, that's why your blood sugar went lower, and you're more sensitive to insulin. So just taking all these variables that affect your blood sugar, and demystifying those and making those understandable for you and actionable. Okay,
Scott Benner 42:51
yeah. So it's really getting people to a better outcome with less effort on their part and it not costing as much is, that's an amazing goal. Let me ask you about a couple of things that you just talked about there. So the, the idea, the idea of an algorithm algorithms, a word everybody's hearing now, because there are so many, you know, closed loop systems that are being developed by insulin pump companies. And so you have, it's no different for you, right, you have there's something living in that app that sees the information coming in and makes better decisions, and how will I and that's something you're thinking about for the future? But how will that look? Do you imagine? Is it in the form of feedback or, you know, suggestions? And can the app make suggestions about my insulin? Or is that a gray area?
Mike Mensinger 43:35
Yeah, there's, there's multiple different ways to do this. And there's a lot of research groups already working on it. So one way this could look is, for example, users on fixed dose therapy, which we are looking to have solutions for them to and then increase their diabetes awareness and move up to more sophisticated bolus calculators. The normal process that doctor takes is they put you on therapy, they guess, at your settings, and then they're going to titrate up a little bit until you get close to your goal. And then if you have any hypoglycemia, they're going to back off pretty simple algorithms that the doctors use in order to make these adjustments. Same thing for both calculator users, that just adjusting your your correction factor in your carb factor. So it's just an incremental little steps and looking at the outcome of those changes, and making sure you're you're getting a lower average glucose without a lot of hypoglycemia. So these algorithms are pretty straightforward. And these are something we think we can help offload the doctors and increase the frequency of those changes. So you get to control and get the target faster. Obviously, there has to be coupled with education and, and other things in order to be effective, though,
Scott Benner 44:46
is there? And you mentioned just briefly, but I want to understand like ideas about getting my long acting insulin to be more effective. Is that something you're working on as well?
Mike Mensinger 44:57
Yes, that's something in our roadmap that we're doing interested in getting to as soon as possible. So it could look like your doctor starts you on the product, you're on a Dexcom or CGM. And so it's looking at your overnight control. And if your glucose is rising steadily, you need more long acting insulin. If it's dropping, if your glucose isn't stable, it should back down your long acting insulin. So the user could see a notification that says, maybe it's approved by your doctor, maybe maybe the algorithm can do it. These are things we'll have to work out with, between our clinical partners and the FDA, right. But you get a notification, it says, we recommend this change, maybe instead of 18 units of lantis, you should be taking 17 now, and the user would be able to approve that and it updates your setting. And now your next time, your reminder goes off to say I'm take your lantis it'll say take 17 units rather than the 18. So very simple, all the user has to do is approve or say no, that I don't agree with that change, let's
Scott Benner 45:56
talk to my doctor, the rest just happens. It's those little things that we don't really consider as much and, you know, I've seen, I've seen it with my daughter, and I'm with other people as well, like, you know, you just inject your slow acting in some when it's you know, it when it's comfortable for you during the day. And that doesn't necessarily mean it's going to work for 24 hours the way it's supposed to. But we just make that assumption that it does. And we move on. And then you see problems that come down the line and you never go back to that you never say well, maybe it's my slow acting because because in the doctor's office, someone said, Hey, this is how much slow acting insulin used, you know, put it in in the morning or put it up before you go to bed, whatever they told you and in your mind, that's a set it and forget it idea. It that must work. I've been told to do it like this. I think it's it's incredibly valuable to have this technology, looking at those ideas and saying to me, Look, don't overlook the fact that maybe this needs to be considered. So, you know, without you having to run around all day thinking about a million things in your head.
Mike Mensinger 46:57
Exactly. It's the system working on your behalf and helping make recommendations, obviously, the user has to play a role in that you don't want to completely remove, you know, the human element of that, whether it's your doctor, whether it's you a parent or or the person with diabetes themselves. So you have to have the right experience that leverages the benefits of each one of those technologies and the person themselves. Yeah,
Scott Benner 47:21
no, that's excellent. And are you guys, I know you and I are speaking I'm sorry, I asked like I didn't know. But I know. So we're talking on the 10th of July right now. And this is going to go up pretty much right away. And in Penn is going to be at children with diabetes this week. When are you guys getting there?
Mike Mensinger 47:36
Yeah, so that that's one of our favorite conferences of the year, just so much excitement and engagement and great opportunities to make everybody aware. So we will we're having a booth, please come by to the booth and say hi, check out the product, we'll have demos there. You can fill out the get in pen form right there. And and also let us know what you like about the product or what you want to see. We love hearing from everybody and just excited to hear what people think
Scott Benner 48:04
microwave colors. It's a pretty superficial question. But can I choose different colors in the pen?
Mike Mensinger 48:09
Well, funny, it's not a superficial question. Because there's a there's a concern of mixing up your long acting and your bolus insulin. Okay, so one of the things we did there was we provided the pen in three different colors. So there's six different models. So we have novo pen, and we have a human log pen. And we have to do that because the cartridges are different. And so the pen has to make sure it's dispensing the right insulin amount for each of those devices to pick your insulin type. And then you get pink, gray or blue. And what we recommend is if you if your long acting pen, if you're using a long acting pen is gray, you know pick blue or pink, and vice versa to make sure you don't mix those up. That's great. Okay,
Scott Benner 48:49
so listen, I don't know if you're gonna be comfortable with this. I haven't told you I was gonna say this, but I'm going to so we'll see where it goes from here. Other companies make pens, right? What Why do I Are you comfortable saying Why do I want yours and not theirs?
Mike Mensinger 49:04
Well, right now, we're the only smart choice that's out there. So eventually, there will be alternatives. We expect to see some competition in the next say two years on the market. So whatever solution works for you, we want the best for users. So of course a decision that you didn't make for yourself. But I think when you really take a look at the solution, what you'll see is it's very user centered design. So we're trying to reduce the work that you have to do day to day and get better outcomes. We've put the data together in an intuitive way such that you can see cause and effect of insulin, carbohydrates and other factors on your glucose so you can learn from that data. The reports doctors are giving us great feedback on really the features in their understanding of doses are missed if you're using the calculator, the split between your basal and bolus insulin along with the daily charts of Seeing all the effects and you can have real powerful conversations and then adjust therapy together. So when you look at the total package, we think you'll see that this is a really great solution and brings a lot of the benefits that computers have had, but really haven't been on available. So
Scott Benner 50:17
Mike, that was very professional, you didn't go all WWE on us there and start telling me why that's a good for you. So No, but seriously, there's there's other pens on the market. So in and they're from companies that people have heard of before. And, and it's important for them to understand that they're not all equal. And that there may be not just maybe, but there absolutely is benefits that far outreach, you just have to try to understand them. And I think that's the last kind of thing I want to ask you about. So trying to understand what I have my pen now I've decided, Hey, Mike made a lot of sense on the podcast, I'm getting an in pen, I have it in my house. Is there a learning curve? If there is how steep? Is it? I mean, how soon before I feel comfortable with it? I think I I think from looking at it, it doesn't seem like it's much to me, but what are you seeing from people who are using it,
Mike Mensinger 51:09
most people are able to pick it up and use it. And it's just very intuitive. Our human factor study, pumps require two hours of training. Typically, as a start, a lot of settings, a lot of configuration that's required for setup, ours, our prescription form that the doctor fills out for all your personal settings for your dose calculator, your insulin type, etc. It looks like the screen you enter it now. So we validated that there's zero training required, and the users are able to set up the product and get going on their own. But we've shown that from very young ages all the way up to, you know, into the Medicare population. And so we've seen great response. And if you do have some challenges, please give us a call. We have a great support department that can help you through any of those issues.
Scott Benner 51:55
But it's just as easy as going into a screen and putting my information in and then it starts helping me make those decisions. And then it went How long do you think it takes to because this is something that you hear people say a lot when they start a pump, like my doctor set me up with this insulin to carb ratio, this but I guess if you're MDI already, you're not going to you're not going to a new way of managing. See, I just answered my own question there, Mike. So when you go from MDI, to a pump, it's not apples to apples always about your your insulin to carb ratio, and other things like that. But from just injecting to injecting nothing like that should change. So I shouldn't see a big, I shouldn't have a spot where I have to make more adjustments afterwards, should I?
Mike Mensinger 52:38
Well, like you said, just like a pump, you have an influence to carb ratio and insulin sensitivity factor, these are your personalized settings, your dose calculator, if there's a process of dialing those in, that would be the same as starting on a pump. So if you know those, and those are correct, and you've been using a dose calculator, maybe it's not a smart pen connected one, well, then you just transfer those settings in and being in using it. If you don't know how to count carbs, that's not a skill that you're comfortable with yet. And maybe you're on meal estimation or other ways of approaching, sizing your doses. And those are things where you can still do that. But you get the benefit of subtracting your insulin on board. And you can see what that number is and just subtract that from the dose you would have taken. Or you can begin kind of learning the skill of using a dose calculator depends on where the user is starting from. And the biggest hurdle would be if you're not familiar with carb counting, and those calculators. But that's an optional feature, you get the benefits of automatic insulin tracking, the reporting, the Dexcom integration, the connected meter integration, the Miss dose reminders, your tempo, all those other things, you don't have to have the skill of carb counting and get all those benefits.
Scott Benner 53:48
And in my case, I don't have a dexcom, I don't lose it. Having a dexcom helps me integrate that information in your app. But if I don't have it, I'm not losing any of the other features.
Mike Mensinger 53:57
Yes, exactly. And obviously, we're talking to the other PGM makers as well to integrate that data because it is so valuable if you have that stream of data to integrate that into the product and see the full picture. But we work with the Vario connected meter, the one drop the agamatrix meter, the sensor meter will be writing to health soon. And it's kind of a magical experience. As a side note here, when when the user has their phone off, they they're on their Vario meter, they take a finger stick, and then they unlock their phone, open our dose calculator without opening a second app, they go into the dose calculator and their BG is already there from your finger stick, the bit magical. You don't have to enter that. So it's wonderful that we could remove that step.
Scott Benner 54:40
What I'm seeing here is there's leaps for two people who are if you're using MDI right now and you're, you're counting your carbs and you're making decisions based on that or if you're not if you're put on more of I don't even know what they call, you've used the phrase a couple of times, but it's so like, it seems so foreign to me the idea of just taking some insulin and letting it roll through the day but Both of these people, these people in these two segments have a real opportunity to make a leap forward in their understanding and their management, if they can have this information at their fingertips. So I don't, I don't see how I mean, if I'm objecting, I don't see how this isn't worth it to me to try. So I really appreciate you coming on talking about all this. Thank you very much.
Mike Mensinger 55:32
You got to remember when I, when I started Dexcom, it was a startup. I really love that early phase where we really get to transform and define and we're new, a new category. And this is a very exciting time in a product life.
Scott Benner 55:47
I think you're the exact right mindset because there are just a lot of people who couldn't leave something that is that stable and successful to try something new. So I am I'm making a leap here. It's not something you've said to me. But I really believe you must believe in this if you've done this. So but you know, I appreciate you continuing to take, take your stabs at making people's life with diabetes easier. And and thank you very much for coming on and sharing this all with me. Yeah, thank you. Yep, have a good day. The impact is bringing the technology found an insulin pumping to multiple daily injection users. If you're injecting insulin, and you don't have in pen, you are missing out on a lot of information that can help you make better quicker and easier decisions about your type one diabetes. The in pen app is absolutely free. And once you've downloaded it, and you've decided that you want to move forward, like Mike said earlier, it is a super simple process to get your insurance coverage figured out and get the pen in your hands. All the links you need are at Juicebox Podcast comm or in your show notes. You can even just go to companion medical.com and find out more. Hey, guys, if you found this episode through the children with diabetes conference, if you were down there and you saw in pen and they told you Hey, if you want to hear more, go back and listen to Episode 170 for the Juicebox Podcast, if that's how you got here, welcome. You may not realize it but you're listening to the best user reviewed Type One Diabetes podcast online, please consider taking a moment to subscribe in your podcast app and listen to other episodes. There are many many to choose from, I would probably started Episode 11. It's called bold with insulin. From there, you're going to meet people who are living with type one diabetes as adults as children and as caregivers. You're going to hear their stories, you're going to hear their management techniques, you're going to be uplifted. So if you're interested in hearing real day to day management techniques that have my daughter's a one c between 5.6 and 6.2 for over four years. And as the kids say spoiler alert, cheats everything. No food is restricted. We talked about how to use insulin on this podcast at its core. That's what this podcast is about. Stick around. Subscribe, listen to new episodes as they come they come every week, or go back in the catalogue. There are 174 other episodes that you haven't heard. Thank you so much for listening. I hope you try and enjoy the in pen. And hope you come back next week for the next episode of the Juicebox Podcast.
You can download InPen for IOS here. Android has been cleared by the FDA and is coming soon.
This episode of the Juicebox Podcast is sponsored by Companion Medical makers of the InPen.
Find out more today.