Justice Served
What would you do if your child’s school refused to listen to you about their care? Would you fight back they way Michell and her family did? Michell’s account of this ordeal is both enlightening and inspirational. This guest post, co-authored by Michell and the attorney that took up their cause, is a must read for parents of children who need their school district to understand.
Guest post from Michell Cheney and Jonathan Chappell
Federal Law Permits a Parent to Give Input to the School Nurse Concerning the Timing or Dosage of Insulin
Imagine if your child’s school nurse refused to even consider your input on a potential adjustment of the dosage of insulin given to your child with type one diabetes (“T1D”) at school, even when there is a medical order giving the parent that right.
As we recently learned, federal law, the Americans with Disabilities Act (“ADA”), supersedes and preempts every state’s conflicting law on this issue. Generally, the ADA requires a school (and many other public and private entities) to make reasonable modifications to its policies, rules, etc.in order to allow an individual with a qualifying disability (as defined by the ADA) to participate or have access to programs and services equally to those who do not have such disability, unless doing so fundamentally alters the program. There is no dispute that T1D is a qualifying disability under the ADA. Most disputes are limited to whether what the student needs is or is not a “reasonable modification.” The United States Department of Justice (“DOJ”) has consistently found that many requests by or on behalf of a student is reasonable. Therefore, the ADA supports a parent or guardian’s right to give the school nurse input on the timing and/or dosage of insulin at school, provided this is permitted by the student’s medical orders.
Unfortunately, though our group of parents knew that we had this right, we were forced to hire an attorney and wait months for the state to reverse its illegal course, and start listening to parents and guardians about potential adjustments to our child’s insulin dosage.
HOW WE LEARNED WE WERE BEING LEFT OUT
My husband Keith and I act each day as our daughter Kira’s primary health care provider, like all Type 1 parents do 24-7. This includes making medical decisions, including whether to adjust the timing and/or dosage of insulin. Type 1 diabetes and the use of insulin is a balancing act, due to (among other things) the nature of the disease, how the insulin infuses differently into the body almost each day, stress, exercise, and many other things that may impact Kira’s blood sugar. Kira is eight, and at least for now must have someone assist her with her care. It is also of the utmost importance that we, as her parents who spend the most time caring for her and know what will or will not work in certain scenarios, must not be left out of the decision of making certain adjustments to the timing and/or dosage of insulin.
This is why at the beginning of the last school year (August 2018), as we began the process of getting Kira ready for 2nd grade with all the requisite calls and emails and meetings and paperwork, I stumbled across a sudden roadblock. Our APRN told us that a representative of the state of Connecticut Department of Education informed the nurses throughout the state that they were prohibited from considering any input by a parent or guardian concerning a dose change. Worse, the nurses were told that if they considered parental input, that doing so was a violation of the Connecticut Nurse’s Practice Act, and the nurse potentially could be sanctioned, suspended, or even have his or her nursing license revoked.
At the same time, the part of the medical form filled out annually by a child’s medical provider that gave the school nurse permission to consider parental input was deleted. The original version, written in collaboration with the experts at the Connecticut Children’s Medical Center and Yale-New Haven Hospital, the two primary pediatric endocrinology centers in the state, gave the endocrinology teams a space to indicate parental changes within a range. We all know the variability of type 1, we all know if it was set it and forget it, we’d all have a lot fewer gray hairs and eye bags. We must be able to adjust to a thousand variables. The permission was removed from the website’s form without any input or discussion with either hospital.
Alarmed at the sudden startling prohibition, I sought to make the state board of education aware of why this was an issue. Someone must just not understand, I thought. Maybe it was a paperwork issue. On our local Type 1 Facebook parent page, I put out the call to see if anyone else had this problem. Who was this happening to? Were their nurses even aware of this change? Were their nurses saying or doing anything differently? Some parents knew nothing about it – those with kids old enough to self-treat largely do not have any nurse involvement, and it wouldn’t affect them as it stood. Others had noticed the absence of that critical line and were equally dismayed. For those of us with little ones, that small allowance in dosing can mean the difference on any given day of this ride we’re on.
OUR RESPONSE
Initially, a group of us decided to write letters to the person who sent the email. The nurse at the State Department of Education is experienced and has worked for the state for many years. We wrote to her explaining the issues, detailing why this is a problem for our kids and their health, and asked for a reinstatement of the initial form. She was responsive, and wrote back to all of us, but she gave no indication that she was changing her position, that the Nurse Practice Act prohibited a nurse from considering any input from the parent or guardian, but the nurse could only follow the medical order of a doctor or other licensed provider listed in the Practice Act. What was most puzzling, is that the original form always signed by such a person, and explicitly states parents may give input to the nurse within certain guidelines. We wrote to her numerous times, and were met with a firm refusal to consider our case, including this quote from one of her emails:
This past school year we have had significant complaints from both school nurses and parents regarding the instructions contained on page 2 of the diabetes form you referenced. In consultation with the State Department of Public Health regarding these complaints the following information was received:
“The bullets at the beginning of part 2 of this form are misleading. These bullets suggest that an RN can revise an order in collaboration with a parent. Unfortunately there are currently no provisions in the RN scope of practice, or anywhere else in Connecticut’s statutes that allow for this. According to our statutes, an RN only works under the direction of a physician, APRN, or PA. An RN does not have the authority to revise or rewrite an order independently. The only exception here would be if the parent was licensed in one of these categories, otherwise any nurse who changed a patient’s dose without an order would be exceeding his/her scope of practice.
Sec. 20-87a. Definitions. Scope of practice. (a) The practice of nursing by a registered nurse is defined as the process of diagnosing human responses to actual or potential health problems, providing supportive and restorative care, health counseling and teaching, case finding and referral, collaborating in the implementation of the total health care regimen, and executing the medical regimen under the direction of a licensed physician, dentist or advanced practice registered nurse. A registered nurse may also execute orders issued by licensed physician assistants, podiatrists and optometrists, provided such orders do not exceed the nurse's or the ordering practitioner's scope of practice. A registered nurse may execute dietary orders written in a patient's chart by a certified dietitian-nutritionist.”
OUR NEED FOR LEGAL ASSISTANCE, INCLUDING THE DEPARTMENT OF JUSTICE
To not be able to adjust Kira’s dose at school meant her care at school was substandard. A new or old pod site, new or old insulin, getting sick, stressed, getting over being sick, new breakfast – all of these are variables that only a parent or guardian can be the subject matter expert on. We know what our kids might or might not eat and being dosed according to static paperwork can be extremely dangerous when your picky 8-year-old won’t eat the new snack they begged for. We know which fruit tends to be difficult to manage for our Type 1 child. These things all matter. In some places the prevailing method of dealing with this is to run them higher than we should – but we are the ones who will have to answer to them when their complications come later. I’m not going to tell my daughter that it’s the result of letting her run high because it was easier, and neither are the other parents.
SETTLEMENT
It was at that point we contacted Attorney Jonathan R. Chappell, who happens to have T1D, and has been a saving grace to the type one diabetes community time and time again. We scraped together enough donations to get started with his guidance. He researched this issue, finding (among other things) that in 2017 this very issue was the subject of a DOJ letter of findings which found the state of New York Department of Education violated federal law, the ADA. Jonathan contacted many stakeholders and ultimately made contact on our group’s behalf with the Connecticut office of the DOJ. Jonathan drafted and filed a complaint alleging violation of the ADA filed with the DOJ. He then worked closely with an absolutely amazing attorney with the DOJ to try to quickly reach a settlement, where the violation of the ADA was deemed so obvious.
We were able to reach a settlement without needing the time to move to a letter of findings or to commence any litigation. The ADA violation was (appropriately) never contested by the state’s lawyers. The settlement discussions were not real negotiations, but instead a discussion of how to correct this issue so there was no question that parents cannot be left out of the process of the care of their T1D students while they attend school.
The terms of the settlement included that the author of the email quoted above was required to send another email (to essentially all the school nurses in Connecticut) expressly rescinding her prior email and the “policy” in violation of the ADA in it. Also, the settlement resulted in the creation of a new and improved form to reinstate prior policy to allow parental input in insulin dosing if the medical order permitted it. The Connecticut nursing board also adopted a declaratory ruling which now makes clear that a nurse does not violate the Nurse Practice Act if the nurse considers the input on the timing and/or dosage from a parent or guardian.
Despite a partial government shutdown, this all happened within less than a school year, which is a relatively fast turnaround. It turns out – as Jonathan predicted even before researching the issue – that the Connecticut Department of Education’s position violated the federal ADA.
DO NOT ALLOW THIS TO HAPPEN TO YOU:
If you are having this issue, you should contact Jonathan, and we are confident that he will be able to get in touch with your local DOJ office or otherwise get you the help you need to fight this violation of the ADA.
We would be remiss to express that we are very grateful to the complainants that resulted in the DOJ in New York’s finding for working to create very helpful precedent. Connecticut parents are once more able to help take appropriate care of their kids while at school.
If you have a few dollars to kick in, Michell and the others are close to being able to make Jonathan whole for his service. I urge you to support people who are out there fighting for the people living with type 1 diabetes and to pick up the mantle in your state if you’re seeing the same injustice. If you have questions about how you can fight this fight locally, Michell would be happy to talk.
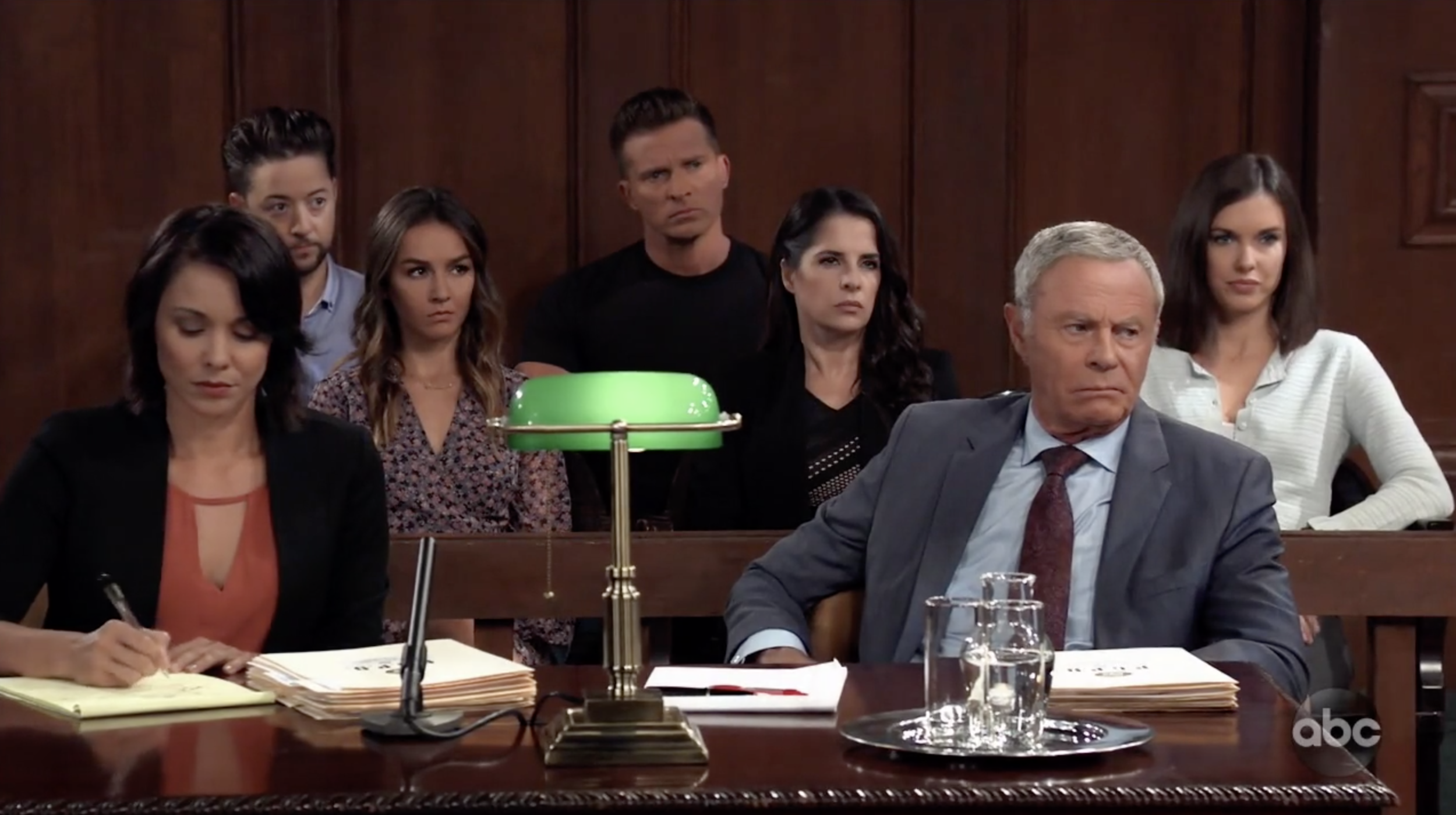
Arden on General Hospital?!
Sometime in August I received this heavily blurred image from a Juicebox Podcast listener named Kate Hall…
The image was a call sheet from an upcoming episode of General Hospital.
Click to enlarge
When I was young I would get home from school everyday at 2:55 pm where I would find my mom getting ready to watch GH. Mom would have a hot cup of coffee and be settling in on our ugly sofa as I arrived. One year the show had a storyline about Luke and Laura that was a cultural phenomenon. It stole the attention of everyone with a television, including me. My memory tells me that Luke and Laura had to “hit the road” to find the left-handed boy. I remember a freeze ray that threatened the city of Port Charles. For a time the show became what mom and I did for an hour after school and into the summer where we would run home from a community pool to see the show. There was even a parody song on the radio about the story. You see kids the radio was a thing that…. never mind. But I should at least explain that TV shows happened on a schedule and you had to be near a TV to see them. I digress…
Back to Kate
Kate is a writer on General Hospital (she’s actually a famous soap scribe), she is also the mother of a little girl with type 1 diabetes. And Kate, as fate would have it is a pretty big fan of the Juicebox Podcast.
And that’s how a character named, Assistant District Attorney Jennifer Arden came to be during a recent two-day story arc. ADA Arden is named for Jennifer (Jenny Smith from the Pro Tip episodes of the podcast) and Arden.
Huge thanks to Kate (who will be on the podcast next year) and to General Hospital for the years of entertainment. Here’s a 60 second video of ADA Arden in action (WITH Tristan Rodgers). That’s right, Robert Scorpio! Sorry… my inner child got jacked up there for a moment.
The only thing left is to get one of you to name a baby after me… 🤣
Omnipod DASH Apps are here!
Omnipod DASH Display and VIEW apps are available now for iOS…
The Omnipod VIEW™ app allows users to see the insulin delivery information of friends and loved ones whether they’re in the next room or across the country. Omnipod VIEW™ is an application that allows you to view PDM data and Pod status information from any Podder™ who sends you an invitation. Upon accepting the Podder’s™ invitation, the Viewer can see the Podder’s™ important therapy-related information, such as alerts and alarms, Insulin On Board (IOB), last bolus, last blood glucose reading, current basal program, PDM battery status, and more.
No matter where your Podder™ is, the Omnipod VIEW™ app offers peace of mind by keeping you connected and informed.
“I can’t quite describe how thrilling it is to be able to see my daughter’s Omnipod data on my phone — her IOB, last bolus, basal settings, history, all of it! It’s like having the DASH PDM display right on my phone.”
With the Omnipod VIEW™ app, you can:
• Monitor your Podder’s™ insulin delivery and Omnipod DASH™ System status remotely
• Stay connected on up to 12 Podders™
• Enable notifications to your smartphone about Podder™ status for increased peace of mind
• Use the Omnipod iPhone widget for convenient access to insulin delivery information on the Today View
• Set up the Omnipod VIEW™ app’s iPhone widget next to the Dexcom widget for a quick glance of your Podder’s™ DASH™ PDM and CGM information on a single screen.
Omnipod DISPLAY™ is an application that displays your Omnipod DASH™ System information directly on your iOS smartphone.
Don’t have Omnipod? get a FREE, NO OBLIGATION demo Omnipod sent to your home - try it today!
With the Omnipod DISPLAY™ app, you can:
• Monitor your insulin delivery and Omnipod DASH™ System status conveniently and discreetly from your smartphone.
• Use the Find My PDM feature to quickly locate a misplaced PDM. Note that this feature works within Bluetooth® wireless technology range
• Set up the Omnipod DISPLAY™ app’s iPhone widget next to your Dexcom widget for a quick glance of your DASH™ PDM and CGM information on a single screen.
• Invite up to 12 friends and family members to use the Omnipod VIEW™ application which allows them to view your insulin delivery and Omnipod DASH™ System information on their own smartphones.
Enable Omnipod DASH™ System notifications to your smartphone.
FDA recalls Medtronic 600-series MiniMed insulin pumps
Alert says Medtronic's MiniMed device could malfunction on airplanes
From the Star Tribune: Entire article can be found here
“The problem has long been known. Medtronic first notified patients about the problem in 2017.”
The U.S. Food and Drug Administration is reminding patients who use the popular 600-series MiniMed insulin pumps made by Medtronic that the devices contain an issue that could cause their buttons to get stuck while flying or other situations when air pressure changes quickly.
The FDA on Wednesday issued alerts for more than 189,000 MiniMed insulin pumps worldwide. Such pumps are used by diabetic patients who need a steady infusion of the drug insulin to break down the glucose in their blood, in addition to periodic doses (or "boluses") of insulin related to meals, exercise and other factors.
The alerts issued Wednesday are classified by the FDA as a class 2 recall, which is a medium-severity action used when a problem caused by a medical product would be temporary, or when the probability of serious adverse consequences related to the problem is considered remote.
Medtronic has issued an urgent safety notification to patients, which the FDA calls a "recall." However, FDA and Medtronic are not requesting any devices be returned to the manufacturer. The FDA uses the term "recall" to include situations where no product need be returned.
The recalls apply to MiniMed 670G, 640G, 630G, and 620G models, which have physical keypad buttons that can temporarily become "unresponsive" when atmospheric pressure goes up or down quickly around the pump, typically during takeoff and landing.
Read the entire article here
Podder Talk
Thank you to Omnipod for highlighting the Juicebox Podcast in their Father's Day blog post!
Two Podding parents chat about being bold with insulin, not being a diabetes defense attorney, and creating great content that helps people manage their type 1 diabetes.
Check out Amy’s post and the podcast conversation that we had.