Stunning admission by Aetna medical director
CNN Exclusive: California launches investigation following stunning admission by Aetna medical director
California's insurance commissioner has launched an investigation into Aetna after learning a former medical director for the insurer admitted under oath he never looked at patients' records when deciding whether to approve or deny care.
California Insurance Commissioner Dave Jones expressed outrage after CNN showed him a transcript of the testimony and said his office is looking into how widespread the practice is within Aetna.
"If the health insurer is making decisions to deny coverage without a physician actually ever reviewing medical records, that's of significant concern to me as insurance commissioner in California -- and potentially a violation of law," he said.
Aetna, the nation's third-largest insurance provider with 23.1 million customers, told CNN it looked forward to "explaining our clinical review process" to the commissioner.
Amazon, Berkshire Hathaway and JP Morgan Chase join forces to tackle employees’ health-care costs
By Carolyn Y. Johnson January 30 at 8:31 AM - Washington Post
Three major employers, Amazon, Berkshire Hathaway and JP Morgan Chase, announced Tuesday they were partnering to create an independent company aimed at reining in health- care costs for their employees.
The independent company would be jointly led by executives from all three companies and would be focused on technology that could increase transparency and simplify health care, according to the joint announcement. It will be free from the need to deliver a profit.
"The ballooning costs of healthcare act as a hungry tapeworm on the American economy. Our group does not come to this problem with answers. But we also do not accept it as inevitable," Warren Buffett, Berkshire Hathaway chairman said in a statement.
Few details were available about the new initiative, described as in the initial planning stages. The announcement comes amid anticipation that Amazon could disrupt health care as it has in other industries -- sending tremors through companies that make and supply prescription drugs.
“The healthcare system is complex, and we enter into this challenge open-eyed about the degree of difficulty,” Jeffrey P. Bezos, Amazon founder said in a statement. “Hard as it might be, reducing healthcare’s burden on the economy while improving outcomes for employees and their families would be worth the effort. Success is going to require talented experts, a beginner’s mind, and a long-term orientation.”
the original article can be found here
Medtronic deal with Aetna ties insulin pump payment to patient results
This does not feel right...
My opinion.... Medtronic has way too much power in the insulin pump space. You may also want to check out Mike Hoskin's thoughts on the subject over at Diabetes Mine.
By Bill Berkrot Reuters
Medtronic Plc said on Monday it signed an agreement with health insurer Aetna Inc under which payment for its insulin pump systems will be tied to how well diabetes patients fare after switching from multiple daily insulin injections.
The deal is the latest example of the move toward contracts for prescription drugs and medical devices that attempt to bring down soaring healthcare costs by tying reimbursements to whether the products achieve their intended results.
The deal with Aetna will measure health outcomes for patients who transition to one of three Medtronic pumps that self-adjust to keep blood sugar levels in proper range based on patients' individual needs for insulin.
"This agreement reinforces our shift towards value-based healthcare," Hooman Hakami, president of the Medtronic diabetes group, said in a statement. "We know technology alone isn't enough and ultimately improved outcomes are what matter."
Patients with type 1 diabetes and those with type 2 who have progressed to the need for insulin typically check blood sugar levels several times a day and inject insulin as needed. The pumps eliminate that chore.
Medtronic declined to discuss financial details of the Aetna agreement, but said such deals tie revenue to achievement of clinical improvement targets, as well as shared savings for delivering on or exceeding clinical outcomes and cost targets.
Suzanne Winter, vice president of the Medtronic diabetes group in the Americas, said the Aetna agreement will initially focus on whether patients on its pumps achieve their A1c targets, a commonly used measure of blood sugar levels. The American Diabetes Association recommends A1c levels below 7.
In the future it may look at other measures, such as hypoglycemia episodes, time in proper glycemic range, and patient satisfaction, Winter said.
Medtronic already has an agreement with UnitedHealth Group Inc that is moving toward including patient outcomes and other metrics, such as total cost of care, and the company is discussing similar deals with other insurers, Winter said.
Pharmaceutical companies are also beginning to embrace reimbursement options that take patient outcomes into consideration.
U.S. biotech Amgen Inc, in an effort to improve patient access to its expensive new cholesterol drug Repatha, has offered contract options that include refunding the cost of the drug if patients suffer a heart attack or stroke while on the medicine intended to prevent them.
(Reporting by Bill Berkrot; Editing by David Gregorio)
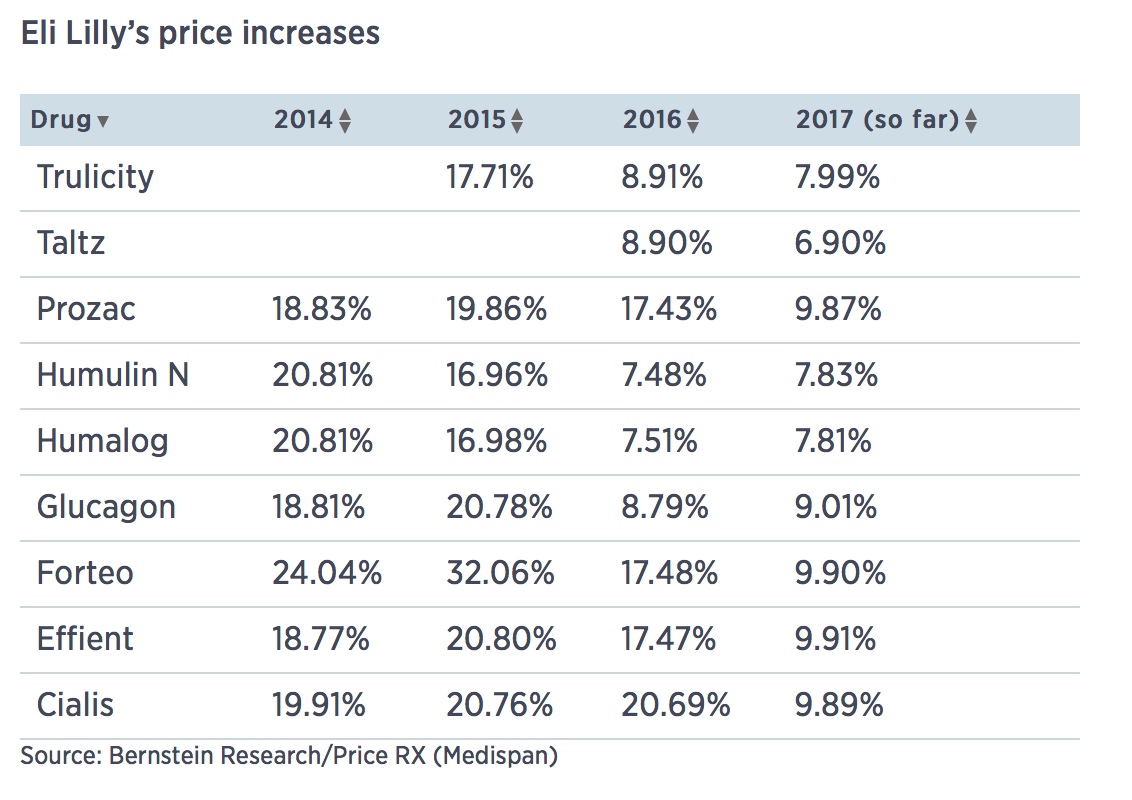
Eli Lilly raised prices on 9 drugs last week
Humalog and Humulin (7.8 percent)
Indianapolis drug giant Eli Lilly raised list prices of nine of its medicines last week between 6 and 10 percent, according to data obtained by CNBC.
The increases, taken on May 2, were for drugs including the blood thinner Effient (9.9 percent), the psoriasis drug Taltz (6.9 percent) and the insulins Humalog and Humulin (7.8 percent).
The increases fit a pattern at Lilly and many other drugmakers of single-digit percentage hikes once or twice a year, despite political pressure and intense scrutiny of the practices. Lilly has come under fire for the price of its insulin drugs in particular, leading Senator Bernie Sanders to call for a federal investigation into collusion. Lilly and other insulin makers have denied any such activity.
Lilly confirmed the price increases in an emailed statement to CNBC, and noted the list prices "do not reflect the significant discounts and rebates that we provide to ensure patients have adequate access to our medicines."
"The net price increase that Lilly recognizes is significantly less," spokesman Mark Taylor wrote. "In fact, in 2016, the average discount to list price on our U.S. portfolio rose to 50 percent and net prices rose just 2.4 percent in the U.S."
You can read the entire article on CNBC
President Obama's Piece for the New England Journal Of Medicine
This piece from President Obama was published in the New England Journal of Medicine on January 26, 2017. Next week on the Juicebox Podcast I'll be highlighting three people living with type 1 diabetes, they will each be sharing their experience with the Affordable Care Act. - Scott
Repealing the ACA without a Replacement — The Risks to American Health Care
Barack H. Obama, J.D.
N Engl J Med 2017; 376:297-299 January 26, 2017 DOI: 10.1056/NEJMp1616577
Health care policy often shifts when the country’s leadership changes. That was true when I took office, and it will likely be true with President-elect Donald Trump. I am proud that my administration’s work, through the Affordable Care Act (ACA) and other policies, helped millions more Americans know the security of health care in a system that is more effective and efficient. At the same time, there is more work to do to ensure that all Americans have access to high-quality, affordable health care. What the past 8 years have taught us is that health care reform requires an evidence-based, careful approach, driven by what is best for the American people. That is why Republicans’ plan to repeal the ACA with no plan to replace and improve it is so reckless. Rather than jeopardize financial security and access to care for tens of millions of Americans, policymakers should develop a plan to build on what works before they unravel what is in place.
Thanks to the ACA, a larger share of Americans have health insurance than ever before. Increased coverage is translating into improved access to medical care — as well as greater financial security and better health. Meanwhile, the vast majority of Americans still get their health care through sources that predate the law, such as a job or Medicare, and are benefiting from improved consumer protections, such as free preventive services.
We have also made progress in how we pay for health care, including rewarding providers who deliver high-quality care rather than just a high quantity of care. These and other reforms in the ACA have helped slow health care cost growth to a fraction of historical rates while improving quality for patients. This includes better-quality and lower-cost care for tens of millions of seniors, individuals with disabilities, and low-income families covered by Medicare, Medicaid, and the Children’s Health Insurance Program. And these benefits will grow in the years to come.
That being said, I am the first to say we can make improvements. Informed by the lessons we’ve learned during my presidency, I have put forward ideas in my budgets and a July 2016 article to address ongoing challenges — such as a lack of choice in some health insurance markets, premiums that remain unaffordable for some families, and high prescription-drug costs. For example, allowing Medicare to negotiate drug prices could both reduce seniors’ spending and give private payers greater leverage. And I have always welcomed others’ ideas that meet the test of making the health system better. But persistent partisan resistance to the ACA has made small as well as significant improvements extremely difficult.
Now, Republican congressional leaders say they will repeal the ACA early this year, with a promise to replace it in subsequent legislation — which, if patterned after House Speaker Paul Ryan’s ideas, would be partly paid for by capping Medicare and Medicaid spending. They have yet to introduce that “replacement bill,” hold a hearing on it, or produce a cost analysis — let alone engage in the more than a year of public debate that preceded passage of the ACA. Instead, they say that such a debate will occur after the ACA is repealed. They claim that a 2- or 3-year delay will be sufficient to develop, pass, and implement a replacement bill.
This approach of “repeal first and replace later” is, simply put, irresponsible — and could slowly bleed the health care system that all of us depend on. (And, though not my focus here, executive actions could have similar consequential negative effects on our health system.) If a repeal with a delay is enacted, the health care system will be standing on the edge of a cliff, resulting in uncertainty and, in some cases, harm beginning immediately. Insurance companies may not want to participate in the Health Insurance Marketplace in 2018 or may significantly increase prices to prepare for changes in the next year or two, partly to try to avoid the blame for any change that is unpopular. Physician practices may stop investing in new approaches to care coordination if Medicare’s Innovation Center is eliminated. Hospitals may have to cut back services and jobs in the short run in anticipation of the surge in uncompensated care that will result from rolling back the Medicaid expansion. Employers may have to reduce raises or delay hiring to plan for faster growth in health care costs without the current law’s cost-saving incentives. And people with preexisting conditions may fear losing lifesaving health care that may no longer be affordable or accessible.
Furthermore, there is no guarantee of getting a second vote to avoid such a cliff, especially on something as difficult as comprehensive health care reform. Put aside the scope of health care reform — the federal health care budget is 50% bigger than that of the Department of Defense. Put aside how it personally touches every single American — practically every week, I get letters from people passionately sharing how the ACA is working for them and about how we can make it better. “Repeal and replace” is a deceptively catchy phrase — the truth is that health care reform is complex, with many interlocking pieces, so that undoing some of it may undo all of it.
Take, for example, preexisting conditions. For the first time, because of the ACA, people with preexisting conditions cannot be denied coverage, denied benefits, or charged exorbitant rates. I take my successor at his word: he wants to maintain protections for the 133 million Americans with preexisting conditions. Yet Republicans in Congress want to repeal the individual-responsibility portion of the law. I was initially against this Republican idea, but we learned from Massachusetts that individual responsibility, alongside financial assistance, is the only proven way to provide affordable, private, individual insurance to every American. Maintaining protections for people with preexisting conditions without requiring individual responsibility would cost millions of Americans their coverage and cause dramatic premium increases for millions more. This is just one of the many complex trade-offs in health care reform.
Given that Republicans have yet to craft a replacement plan, and that unforeseen events might overtake their planned agenda, there might never be a second vote on a plan to replace the ACA if it is repealed. And if a second vote does not happen, tens of millions of Americans will be harmed. A recent Urban Institute analysis estimated that a likely repeal bill would not only reverse recent gains in insurance coverage, but leave us with more uninsured and uncompensated care than when we started.
Put simply, all our gains are at stake if Congress takes up repealing the health law without an alternative that covers more Americans, improves quality, and makes health care more affordable. That move takes away the opportunity to build on what works and fix what does not. It adds uncertainty to lives of patients, the work of their doctors, and the hospitals and health systems that care for them. And it jeopardizes the improvements in health care that millions of Americans now enjoy.
Congress can take a responsible, bipartisan approach to improving the health care system. This was how we overhauled Medicare’s flawed physician payment system less than 2 years ago. I will applaud legislation that improves Americans’ care, but Republicans should identify improvements and explain their plan from the start — they owe the American people nothing less.
Health care reform isn’t about a nameless, faceless “system.” It’s about the millions of lives at stake — from the cancer survivor who can now take a new job without fear of losing his insurance, to the young person who can stay on her parents’ insurance after college, to the countless Americans who now live healthier lives thanks to the law’s protections. Policymakers should therefore abide by the physician’s oath: “first, do no harm.”
The Massachusetts Medical Society copyright applies to the distinctive display of this New England Journal of Medicine article and not to the President’s work or words.
This article was published on January 6, 2017, at NEJM.org.
SOURCE INFORMATION
Mr. Obama is the former President of the United States.