#666 Half a Century
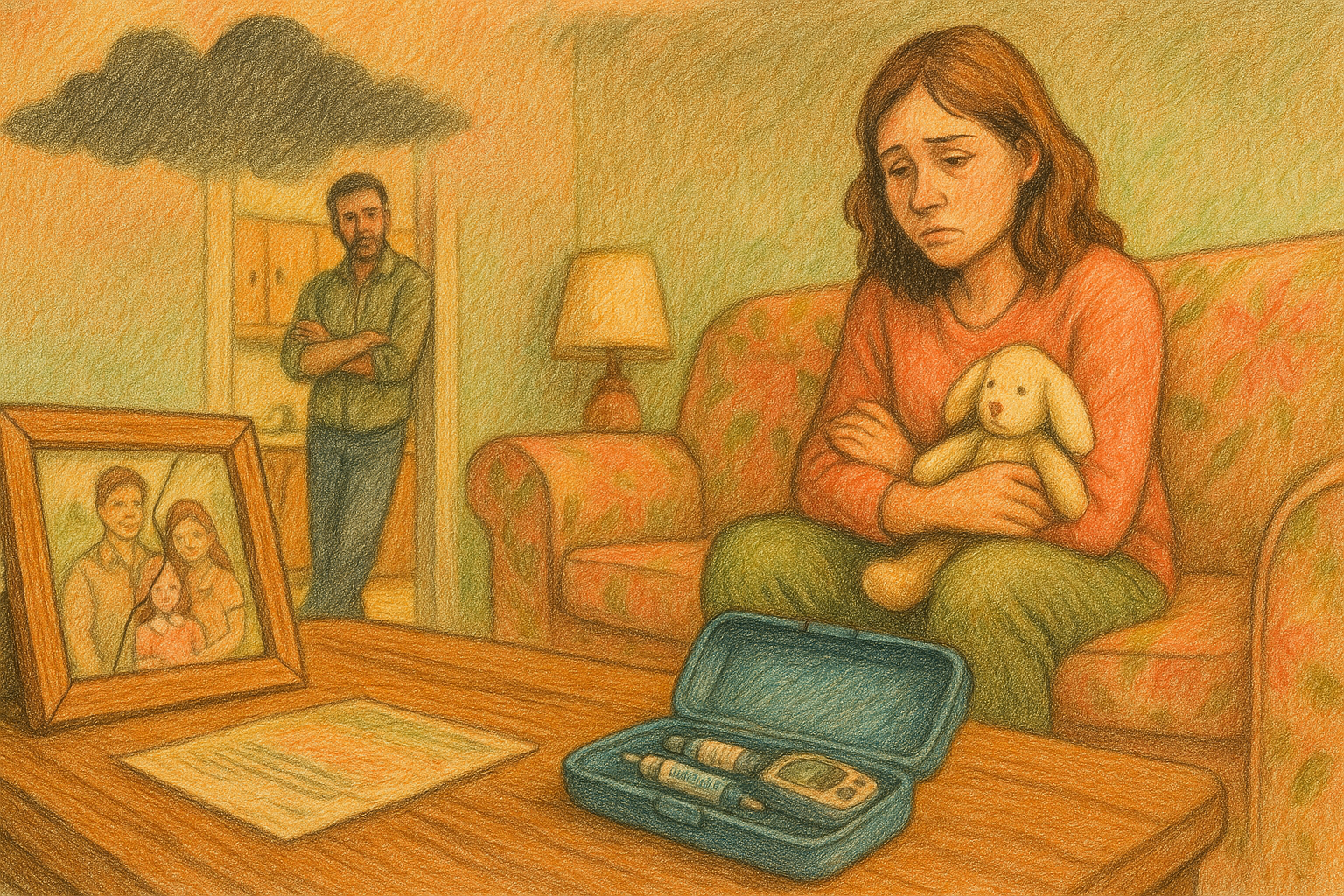
Christine has lived with type 1 diabetes for over fifty years.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
fair to say that everyone listening today is not superstitious, as I welcome you to Episode 666 of the Juicebox Podcast.
Christine's on the show today she has had type one for many, many, many, many decades. And she's going to tell us her story. If you play this next bit in reverse, it will reveal who killed President Kennedy. Please remember today that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan, or becoming bold with insulin. Now try to figure out how to play a podcast backwards, you're never gonna do it. Keeping this theme going for episode 666 I compel you to go to T one D exchange.org. Forward slash juicebox. And take the T one D exchange survey. When you do you'll be helping people with type one diabetes and supporting the show. All you have to be is a type one who is a US resident or a US resident who is the caregiver of a type one. After that T one D exchange.org. Forward slash juicebox fewer than 10 minutes and you're done. It can tell the this show is sponsored today by the glucagon that my daughter carries. G voc hypo Penn Find out more at G voc glucagon.com. Forward slash juicebox. today's podcast is also sponsored by touched by type one visit touched by type one.org. Or find them on Instagram and Facebook. I mean honestly, you could probably do all three of those things, find them on Instagram, Facebook, and visit touched by type one.org.
Christine 2:04
Hi there. I'm Christine and I'm recording from Oregon. Oregon. I grew up in Wisconsin. And I've been out here though most of my life.
Scott Benner 2:19
You went from Wisconsin to Oregon when you were younger.
Christine 2:22
After college, I went to school at the University of Wisconsin at Madison,
Scott Benner 2:28
if I will avoid Oregon or something. I'm
Christine 2:31
a girl. I'm kind of kind of a boy, I heard that Oregon was a beautiful place to be and I had done some internships out in the west and just headed out this way. And as soon as I got here, I knew it was where I needed to set my routes down. But I came out here by myself basically.
Scott Benner 2:54
Okay, that's excellent. All right. Let's let me remind you, as we go, zippers, banging anything like that is gonna come through pretty loud. You have a really good microphone, so Okay, try not to fit. Are you nervous?
Christine 3:11
Um, I'd be lying if I said that. I didn't have a few butterflies, but generally, I don't get nervous. Um, I'm excited.
Scott Benner 3:24
Good, good. It's gonna say, Christine, you're a grown person. There's nothing to be nervous about. I think it kind of it fits into your story. So how old are you?
Christine 3:34
I just turned 65. Yeah, happy birthday in September 14. Congratulations. Yeah, it's getting diabeetus at age 13. On my birthday, basically, was, was quite the present.
Scott Benner 3:52
Do you recall any of that?
Christine 3:54
I do. How did it happen? Um, I recall standing at the kitchen sink, all summer long drinking gallons of cold water. And my mother would say that I would sit down at the table before anybody got there. And I'd start eating. And I was still there after everybody left. And I was pretty little I was, you know, that was seventh grade. Going into seventh grade. I was 7075 pounds. And I was just eating like a horse. And it was mostly my mother was watching that scenario go on. And when school started, it was in the days. I don't know that they still do this but the nurse we'd get weighed, and I had lost six pounds from the year before. During a period of time where you're supposed to be growing Right. So Mom took a urine sample into the doctor. And bingo, there it was. So I wasn't sick. I think it was caught pretty early. My recollection is maybe my blood sugar was in the four hundreds.
Scott Benner 5:19
I have a question. Did the doctor asked for a urine sample? Or was your mom just the kind of lady that when you didn't feel good, you had to pee in a cup?
Christine 5:25
I know, I think I think she had a doctor's appointment for herself. And then she called in and talked about what was going on with me that I had lost the weight and she was watching the water drinking. And they said, just bring a urine sample in. So and that was the weekend of my 13th birthday. And he wanted me to go to the hospital right away. And she said, Well, we're having a birthday party this weekend. And he says, Okay, you can wait till Monday, but don't let her eat too much birthday cake.
Scott Benner 6:02
Oh, you didn't get a cake?
Christine 6:05
I think she let me have a little bit.
Scott Benner 6:08
And then from there, what is the policy? I usually ask what the beginning of your management life is like, but it's gonna be a big chunk of it for you, right?
Christine 6:18
Yeah, well, it was 52 years ago. And if that was in the days of you pee in a cup, you check an eyedropper and put in, I don't know, five drops of urine 10 drops of water and then this little tablet in it fizzed up and turned color. And usually, you know, to have no sugar in your urine. It was blue. But by the time you're dumping sugar into your urine, you're already way too high. So it was pretty rudimentary tools that we had at that time, and I was mortified that I would have to do this at school, you know, lock myself in the bathroom and pee in a cup. And you know how the day
Scott Benner 7:17
is how often did you do that? Well,
Christine 7:22
I do remember doing it at school a couple of times. And then probably going to the doctor and crying about it. And he said I didn't have to do it at school anymore. So no, we probably did it in the morning and in the evening. You know, we we boiled the glass insulin syringe and put a new needle on it every morning. But it's pretty long time ago it was beef and pork insulin and and probably on some sort of mixture. I don't remember we certainly didn't have fast acting insulin.
Scott Benner 8:03
No, no. This is 1969. Is that right? Yes. Yeah. You know, if your birthday was a month sooner, I could call this episode summer of 69. But fall of 69 it's not going to make anybody go Oh, I wonder what this is about?
Christine 8:18
I think I think something else will come up.
Scott Benner 8:21
Yeah, you've exceeded your to say something insane in the next hour. Okay, well, let's get to that part, then. I do want to like dig through a little like contextually, like you say it's so offhandedly like we boiled the syringes and, and but you had a set right? They were glass syringes with metal needles, and then every time you use them, they had to be sterilized.
Christine 8:46
Right? You know, I don't remember boiling the needle. I think there were disposable needles that you just clipped on the top of that class syringe? Sure. Um, but with you know, that went on, because I was in seventh grade. And I just kind of remember that class syringe for a long time before they came out with the disposable needles. Show. Yeah, the doctor didn't say I had to keep doing that urine test at school, but I was doing it at home. Um,
Scott Benner 9:20
what? What was the goal of the test?
Christine 9:24
The goal of the test was to have it be blue, that meant you didn't have sugar in your urine. But again, my recollection was that by the time it turned a different color was that you had already dumped a lot of you know, from your blood, filtering out the sugar into your kidneys. Your blood sugar is already pretty high. So that was the best that we had at that time.
Scott Benner 9:55
But I mean, if it wasn't blue, you didn't get more insulin right? No, what did you say? up eating or running around, or what was the plan, then
Christine 10:04
you just kept taking your insulin dose. You know, there really wasn't much strategy that I remember. It was I was on one of those diets that they called the exchange diet. So, for breakfast, I had two starches a protein, you know, a fruit, a milk, lunch, you know, kind of the same sort of thing. And my mom was pretty good at sticking to that exchange diet and what that all meant. It was harder on her than it was on me. She had a hard time giving me shots. I mean, she would just fall apart every time she had to give me a shot. And I would just say, Mom, just give me the needle. And I would, and I would take over it. That was it. It just hurt her to feel like she was hurting me.
Scott Benner 11:07
How many? How many kids? Did your mom have?
Christine 11:10
Um, there are four of us. We were all really stretched out my I had an older sister who is eight years older than I was. And then I came along, and then a younger sister who is almost four years younger. And then another brother, who is you know, there was almost eight years between him and I
Scott Benner 11:31
wow. So was your mom only fertile every eight years or?
Christine 11:34
I know, I didn't get to ask her. Before she died. What was that family? What the heck was going on in between? I know there was one miscarriage. I think between me and my younger sister. So yeah, who knows?
Scott Benner 11:54
Maybe your dad was only nice every seven years or so?
Christine 11:58
My dad, my dad wasn't around very much. So that may have been part of it. I don't know.
Scott Benner 12:04
No, it's interesting. That's all yes. How would you know, but I don't know. I'm interested. I love that. So okay, so you do this for ever and ever. And there's not a ton of impact on you, right? Like, you don't remember your life as being difficult.
Christine 12:21
I don't I, I have never in 52 years been hospitalized for DKA. I remember never skipping an insulin dose. I do remember screwing around with my diet, though, that as time went along, and you started to push the envelope a little bit and go, Oh, I really want a piece of cake. And you'd eat the piece of cake and nothing really bad happened. You just kept pushing it. And I think I was pretty good in high school, you know, just kind of telling the mark, I was a good girl. And um, but then when I went to college, I went through some rebellious years, and maybe a little bit of light depression, about about living with this disease and kind of using it a little bit to be in denial. I mean, I remember going down for the vending machine in the college dormitory and getting not one Snicker bar, but five, I'd eat five Snickers. And then I'd get really tired and take a long nap. But I never got it never got so bad that I ever was hospitalized. So I'm patting myself on the back for that for all these years that I never really got into serious trouble,
Scott Benner 14:04
even in college that there is no meter right.
Christine 14:07
So, in college, I finally got to see an endocrinologist. Up until that time. I was still being seen by a family doctor, and I didn't know about endocrinologist. And for some reason, you know, we must have had a health plan at at the school, and I got into at the University of Wisconsin to see this Scottish physician. And there's a couple of things that I remember very distinctly about him and that really helped to form how I carried on with this disease and so So he, I don't know if we I don't I don't think because that was in the late 70s. I don't think we still had the a one C test. I don't know, you might know when that test was developed. But um, I remember him saying to me, he actually called me at home one night maybe to give me some lab work. And he basically laid it on the line and said, you know, you really got to get your act together here. And he used
Scott Benner 15:44
you froze? Hold on a second. Christine, hold on. You are frozen frozen? Is Oregon internet is dodgy. Something happened to the tree you live in? What happened?
Christine 15:57
I don't know. I don't know. I checked my internet connection. It looks okay.
Scott Benner 16:01
It's okay. Don't worry about it. You were talking about the doctor. And
Christine 16:05
so he called me and he said in his little Scottish accent, Gather ye rosebuds. While he may. And I remember that. And I guess it hit home. And there were a couple of other things that hit home right at that time it was I was in my early 20s. I did have a cousin, a second cousin who developed diabeetus, we were the same age. And but he developed it five years earlier than me. And when he was 21, he lost his sight due to diabeetus. So I had this doctor telling me this, I had my cousin who had just gone blind. And I was like, Oh, my God, this stuff is real, I better start paying attention here. And I got on the bandwagon. And I and I also was studying to be in a health occupation was vacillating between two different fields. And being in a Health Occupation, you you know, I was exposed to people who had complications I was exposed to, you know, stuff that was going on in the medical field. And I really think it helped me to get on board. Okay, quickly. Yeah, he was
Scott Benner 17:40
telling you, by the way, Gather ye rosebuds. While ye may, proverb act, and it may, it means enjoy yourself now, before your situation is changed.
Christine 17:50
Exactly the rest of the poem goes. Gather ye rosebuds, while ye may old time is a flying, and this same flower that smiles today, tomorrow will be a dying. So that really stuck in my head. And and, you know, I'm grateful to him for that i He, I got involved in a couple of research studies. In college. He did one he asked me if I would volunteer to be hospitalized for a week. And I was all about trying to do the right thing. And the hospitalization was going to be about seeing if you could get a faster reaction from your insulin. And by that time regular insulin was out, I believe. And to see if you could get a faster reaction if you didn't, I am injection inner muscular injection. And I said, Okay, I'll do it. And admitted myself to the hospital. I was probably in for five days. And they were starting to do blood tests, then at that point where you put a drop of blood on a strip and the strip turned color. It was still pretty wide ranges, but it was better than the urine testing. And so I had to agree to using a one inch needle that you'd go straight in usually to your quad Big Muscle on your thigh and see if having muscle uptake was faster than subcutaneous. So the I don't know what they used to measure. I don't know how long I did it for But it was an interesting theory. And it didn't go on very long. And it was it's painful to do an I am injection sounds like it. Yeah, yeah. And the cost, the benefit wasn't real clear. And, you know, he said I didn't need to keep doing it, but showed there was that study. And then there was also a study going on that just started at the University Wisconsin called the The Wisconsin epidemiological study for diabetes, retinopathy, that did W E, S, D, R. And they were looking at, you know, control how well your control was, and they were going to do a 20 year study. And I was followed in that study for probably not quite 20 years, they stopped the study, because the results were so obvious that if you had good control, that you could slow down I disease, and they measured a bunch of things. And every year, I'd go in and have my eyes photographed, and just go through a series long series of questions. And it was usually a two hour appointment that I had. But they they did stop that study before 20 years, because the evidence was obvious that could control was
Scott Benner 21:39
read good outcome,
Christine 21:41
and had good outcomes. Yes. So and but we still didn't have good tools, right to measure. And,
Scott Benner 21:51
well, you know, you mentioned the a one t test with the best I can find is that in the 80s, the A one C test came up. Okay. And it doesn't say exactly when but that's also the decade of meters, test strips requiring less blood, like all that stuff sort of picked up a little bit in the early right. Through the 1980s.
Christine 22:11
Yeah, yeah. And I graduated from there in 1981. And I, I'm an occupational therapist, so I worked in hospitals and clinics. And I, I worked with a lot of people who had diabeetus, because in their complications, so as an occupational therapist, you help people to deal with their disease process or injury. And I got to see what happens when you don't take care of yourself.
Scott Benner 22:48
So, so those people you were working with could maybe act as the Ghost of Christmas Future for you. And it did keep you in line a little bit.
Christine 22:55
Oh, I'm sure that it all influenced. Yeah. You know. And then, you know, I was constantly, you know, in the field where I had good access to health care. And, um, yeah, I mean, all of it helped. I'm really glad that I chose that occupation. And I had that sense of, and I don't know which doctor along the way, said, You know, this isn't a death sentence, getting diabeetus there's a lot worse things out there. And I looked at, you know, our family history, and there was, there were things in our family history, like depression, developmental disabilities, muscular dystrophy, alcoholism. And I thought, you know, maybe diabetes isn't so bad, you know, we all get somehow struck down with something in our lives and diabetes teaches you how to live balanced and healthfully exercise eat right, all those things. And I took on that attitude of this isn't horrible. It college. I did. I think it was probably through going into that university health clinics. Somebody told me about a support group. And from college on up until even now, I've always been involved in some sort of support group around diabeetus. And I remember clearly that we had a nurse in our support group, and he was talking about how and again, this is late 70s, early 80s. How he says, Well, you know, if I wanted to eat I'm a little bit more I would just take some more insulin. And we all the rest of the people in the group we just guessed, like, oh my god, you can't do that. You can't just take more insulin. And he said, why not? You know, and it was that first sign of, yes, you could take more insulin to cover more carbohydrates or, you know, yeah. And so, of course, you know, that's where we are now.
Scott Benner 25:33
Well, I want to ask you a couple questions before we keep going. So there was like, muscular dystrophy in your background? That's autoimmune, I think, right?
Christine 25:42
Um, yeah, maybe it was on my dad's side. diabeetus was more on my mom's side. If if, in fact, you're right, I don't know that. But how about that would be the main autoimmune thing.
Scott Benner 25:59
How about thyroid, any thyroid, celiac? That kind of stuff?
Christine 26:07
Kind of surprisingly. You know, thyroid disease is pretty prevalent, but I don't remember anybody.
Scott Benner 26:15
Maybe, maybe, um, maybe Muscular Dystrophy is not it's the best I have here is a hyperactive immune system can lead to inflammation and autoimmune disorders. Muscular Dystrophy is a group of inherited diseases that lead to progressive muscle weakness. Yeah, it's not it's not making an indication there. Okay. Yeah. Depression, though, huh?
Christine 26:38
Yeah, I think my mom suffered from depression, my sister. There's alcoholism in my family. So when I looked at all those things, I thought, okay, maybe diabetes so bad. I mean, at least, I mean, I found a way to embrace it. Which I think it's a healthy way to
Unknown Speaker 27:01
live with it. Yeah. So I mean, I
Christine 27:03
would I would I rather not have diabetes, of course, right?
Scott Benner 27:07
Where did you find support groups back then.
Christine 27:11
So that one was, through college, there was some sort of thing on campus that we'd meet. And then as I was taking jobs in hospitals, or kind of working with my doctor, you know, it was often suggested, oh, there's a support group that meets, you know, once a month, that's such in such a place, and they would have guest speakers come in, or we would all just get together and bitch, you know, about having this disease or help each other to, you know, deal with certain things like how do you? How do you function with this. And I also, I just, we kind of know, in research that support groups help people to, to function better to live longer. You know, they say that women who are involved who get breast cancer who are involved with support groups often live longer with their disease. So we know it's a healthy concept. And I've been fortunate. Now up until COVID. Those last support group that I've been in was at a pump, users support group. So when I was vacillating about going out a pump, and I really pushed it away for a long time. It had been suggested by my doctor, you know, try a pump, dry pump. And I was like, you know, I do pretty good without it, and I wasn't ready for that attachment. And it wasn't until I get I was in my 40s. Show. I went along. I wrote jotted down some notes last night about I probably went along about 30 plus years, on MDI. And I've been on a pump now for 20 plus years. And what pushed me to finally go on a pump was that I couldn't remember. Like, when did I take that shot? How much did I take? You know, and when was my insulin gonna peak? I just couldn't remember, you know, it's just loose, you know, start to lose your mind in your 40s and 50s. And I was like, Okay, I should come. And I was the first pump that I went on was that Cosmo pump and I love After that little pump, I was very sad when the company went out of business and I think I went through two Cosmo pumps. And then I went through two animus pumps. Those are the ones that
Scott Benner 30:14
you hear people. They're very romantic about the Cosmo and and the ping Right. Was that yeah,
Christine 30:20
I liked the Cosmo. I did not like the ping, though. The endless scrolling just started to get to me. And so when they came out with the touchscreen, on that tandem, I couldn't wait to get that. So Should I've been on I've had to tandems now and I'm gonna be up for my next hand. And next year,
Scott Benner 30:45
can we? Can we talk for a little bit about what it's like to get older when you have to remember all this stuff? Because I'm I'm 50. And I searched for words. Sometimes, I have a fairly decent vocabulary. I don't whip it out all the time on the podcast. But there are times I couldn't tell you where to go to look for it. But I'll talk around not remembering a word. And I'm pretty good at it. So you might not hear it. But I'll feel as I'm speaking when I get going. I know what I'm saying before I say it. So I'm five words ahead. And I'm like, oh, gosh, it's almost like looking up the road and seeing a tree falling across the road. And I'm like, Oh no, there's a tree across the road, meaning I don't remember the word I want. And then I will speak an entire sentence to avoid needing that word. Like I'll explain the word instead of doing that. That's one of the things I've noticed as I get older. But I don't have to remember that I gave myself insulin and is there fat and what I ate and stuff like that. I really do want to know what that's like?
Christine 31:45
Well, I would say that right now at 65 If I have any fear that I have about MIT continuing to manage this as I get older.
Scott Benner 32:05
G voc hypo pen has no visible needle, and it's the first pre mixed auto injector of glucagon for very low blood sugar in adults and kids with diabetes ages two and above. Not only is G voc hypo pen simple to administer, but it's simple to learn more about, all you have to do is go to G voc glucagon.com. Forward slash juicebox. G voc shouldn't be used in patients with insulin, Noma or pheochromocytoma. Visit G voc glucagon.com/risk.
Gonna get back to Christine in just a moment. But before we do, I'd like to remind you to go to T one D exchange.org. Forward slash juicebox. And take the survey also to get a touched by type one.org. And find out what they're up to over there helping people with type one diabetes as they do find them on Instagram, Facebook, and on their website touched by type one.org. I'll remind you that the links to the sponsors and all of the sponsors can be found in the found can be found in the show notes of your podcast player. And at juicebox podcast.com. No kidding. When you click on the links and support the sponsors, you are keeping the show frequent and free. So I appreciate your support very much. That's it you're ready. Here comes Christine.
Christine 33:35
Continuing to manage this as I get older, so certainly going out a pump helped immediately with oh, all the history is right there. I can just go and look and find it. Okay. But you're right. As I'm aging, I'm noticing that I can't walk from room to room without going oh my God, what did I what am I doing here I there was something I was going to get and I have to retrace my steps and, and it does impact well impacts everything but particularly, you know, diabeetus and I heard a statistic once about that as a diabetic. I'm I am thinking and having to make at least 200 Or maybe 300 I don't know what it is extra decisions in a day about what I'm putting in my mouth counting, you know, doing the numbers. You know, the pump does numbers for me, but all those little things that as a diabetic, you are thinking about that. Nobody, you know people don't have diabeetus don't have to think about and when you think of 200 extra little pieces of detail in a day. That's a lot you And so it is a fear that I have about what am I going to do? And I, what if I forget the steps of, you know, filling my pump? And I have to be, I've noticed now that when I'm loading my pump, I need to shut the door. Don't let anybody interrupt me. Because I might lose track. And I might skip a step or you know, or have to go back and start over. But yes, I am noticing the impact of just ah, just a yes, exactly.
Scott Benner 35:39
I mean, as a person who worries about a person who has diabetes, you know, I think the, the way I always thought of it is the first thing that concerns me greatly was, of course, Arden was diagnosed so young. And so when they're telling you stuff, like don't worry, you know, side side effects from diabetes and those impacts, they don't come for 30 years. And I was like, Oh, well, she'll be 32 then when she started having problems, like, that's not comforting, you know, were you trying to comfort me, because that didn't do it. Then there's the thinking about being on your own. And that whole process that you spoke about, about kind of, you know, just rebelling against life and going through that late adolescent period, getting, you know, getting out of your 20s alive, basically, that feeling. And then, you know, having to build a family being concerned that if you make a baby, is your baby going to have autoimmune issues as well? Is that something you want to give to someone else? And is it a burden you want to add to yourself? Because now you're not, you know, I think about how difficult it is to be the parent of a child of type one, but I don't have type on. So if you add that, is that an extra thing. And then I think about the getting older parts that we just spoke about. And then the part that scares me the most that if I talk about too long, I will just cry is what about when dexterity gold goes when you get older, like with your hands and grabbing and twisting and being able to manipulate small things and buttons. And then I feel like oh, God, like there'll be a day, if she lives that long, she'll have to go back to injections. And she won't know what the hell she's doing with that. And I won't be there. And you know, like, that's that that kind of like tidal wave of how I think about all that stuff?
Christine 37:20
Yeah. So I did make some decisions in my life based on just what some of the things you just talked about, I did not have children. And I remember my doctor at the time, who is a, he, he was an endocrinologist saying, okay, now's the time, I didn't get married till I was like 30, he says, but if you want to have a baby, you should do it sooner rather than later. And pumps were just coming out. And he said, we can put you on a pump during your pregnancy, which would help. And I just, I was sitting on the fence. And the one thing that probably multiple things, but a big thing that stuck out was I can probably get through this pregnancy successfully. I will be a good mother. But I will probably not take as good care of myself. Because I'll be taking care of a kid. I knew that my own my energy would go to taking care of the kid instead of taking care of myself. And you know, I have moments right now where I feel like I really wished that I had a kid. Just one would have been nice. But I didn't. I made the best decision that I could at that time. And I probably wouldn't be as in good health as I am right now. I think I could be wrong. But definitely pregnancy is hard on your body, anybody's body. And when you're diabetic, it's going to be a little bit harder. So, you know, I did that. That was a pretty large part of my decision not to have children.
Scott Benner 39:26
How was your husband with that?
Christine 39:28
I'm sure he was okay. Um, he I think he sat on the fence as much as I did. And so
Scott Benner 39:40
are you guys together? No, we
Christine 39:43
were no longer together. So, um, but,
Scott Benner 39:48
but at that time, it felt like he was in on it.
Christine 39:51
Yeah, he was supportive. And so, like, it wasn't like, it wasn't like, you know, he really felt like he went I have a kid and he was disappointed by the fact that I wasn't going to lean in that direction.
Scott Benner 40:05
Is that one of the more difficult decisions you've made?
Christine 40:10
I suppose, you know, none of the kids and my siblings, nobody had children. So there's, there's really no, yeah, a four out of four of us. Nobody had children
Scott Benner 40:24
purposely for the other three.
Christine 40:27
Um, you know, I think because my dad was not around very much. I don't think we had a really great role model of good family, what what a good family looks like. And that may have been part of it. My I think my youngest brother may have wanted to have children and his wife didn't. My older sister had some stepchildren, and then I have a younger sister who might have but she died of alcoholism. And at a young, pretty young age. And so yeah. Probably lots of different reasons. But it is unusual to have four kids. And there's no, there were no offspring.
Scott Benner 41:21
I need to ask you just so I don't wonder the whole time your father not being around. Was that alcoholism?
Christine 41:27
I think so. Yes. Hidden, hidden alcoholism. And I really, I didn't realize that until he was almost dead, you know, there was like, Oh, my God. That's why he was never around. He had his own business. And I think he was drinking over there. And I asked my mother about it. One day, they were both ill in their 80s. And I said, Was Dad drinking over there in his welding shop and and she changed the subject and said, No, so fast, I got whiplash.
Scott Benner 42:05
If you pardon me, Dad fight in the war.
Christine 42:10
He was in World War Two, he did not do combat. He had a desk job in the army, because of some sort of something I think he had, because he had a vision thing. They gave him a desk job. So
Scott Benner 42:28
I was just, I was trying to get out. I was wondering if he had PTSD or anything like that, before they understood what it was. So that's okay. I didn't mean to dig up your entire I just know.
Christine 42:39
I know. Okay. It's i It all relates. It relates. Yeah.
Scott Benner 42:44
No, I think it does, too. And I just sometimes I hope that people can see that that some of these details, make some of the bigger statements make more sense. And then they become valuable, not just you and I chatting for no reason. I appreciate that. Thank you. Yeah. So now it's funny, you know, I've heard a little beeping. What What technology do you use right now?
Christine 43:10
I don't know what was beeping. I have a tandem pump. I have a duck's Trump. Oh, to just be Yeah, no heard that.
Scott Benner 43:19
Your blood sugar's whatever your high threshold is you hit it about 10 minutes ago. You're right. I know.
Christine 43:26
Meal. I ate oatmeal this morning for breakfast because I didn't want to. I wanted a little spike this morning. I can eat oatmeal without getting a spike. But when I when I'm getting too low. I start not to think clearly. And I wanted to be thinking very clearly this.
Scott Benner 43:47
So that's interesting. Are your are your goals based on on that? Really? Like were you? I mean, obviously your goals are where you feel good, but are yours different than like somebody else's? Perhaps.
Christine 44:02
So you mean you want to know what my targets? Yeah. And have they changed? She got older. Oh, they've changed as I've listened to your podcast, oh, they're getting tighter and tighter and lower and lower. I mean, I had my parameter set it between 70 and 150. And, you know, and I was on MDI, for 30 plus years, and they started doing a Wednesday tests. I always on MDI was hovering in the low sevens. Probably when they first came out with the A one C test, I might have been an eight ish, I don't remember being much more than an eight. And then that test really kind of made me hone in better and I always was in the mid sevens. And then once I got on a pump, I dropped down into the sixes and And my last a winsy. And I never ever thought this would happen even though I was listening to you, I was getting bolder with insulin, I was doing Pre-Bolus saying and working with my basals I thought there is no way I will ever get into the fives like some of these people are doing. I just thought that was phenomenal. That my last one was a 5.6 Wow,
Scott Benner 45:29
that is amazing. Good for you.
Christine 45:31
I know. And it was like, it seemed effortless. Show. So the the one thing that, you know you, we were talking about these aging issues. And the one thing I wanted to emphasize was, you know, the idea of complications that we all we've learned about if you know the complications of diabetes, if you aren't trying to stay in control, I kidney, vascular system and all that. But, and I've pretty much evaded those things, I have one thing going on with my eyes that I'm getting some treatment for. But I think that's that's the most wonderful thing right now that I mean, you can still have diabeetus and have none of this technology and do a bad job. But what I'm seeing and hearing is that people are getting onboard with the technology right away, they're doing such a great job. They're not even, you know, they get diagnosed with a a one C of 10. And then in three months, they're down in a normal level, it's like, we're gonna get to a period of time where we don't see those complications anymore. And that is so much, I think, for families, parents to hang on to, you know, the idea that, wow, I can pretty much a kid normally, you know, I have this attitude of this disease isn't as bad as a lot of other things could be. But now you can have this disease and really hone in with all the technology and hopefully not have to be looking at any complications down the road. Yeah,
Scott Benner 47:32
no, I mean, it's, it's only been a number of decades. It's funny when you talk about your life, and you say, I was MDI for 30 years, I'm over 20 years on a pump. Now, my first reaction is like, it's astounding, you know, it feels like you've lived lifetimes inside of a lifetime is how it makes me feel. And at the same time, when you really consider it, there's, you know, past the late 80s, diabetes started to, to move in a completely different direction. And if you even cut away the the 80s, and the 90s, from your, you know, from your analysis of the last 10 years, is astonishing, compared to the first, you know, decades. Exactly. And I think that some of some of the problem is holdover. It's people who live so long in the first part, or the second part, that when they are as doctors giving advice to people who live now, their advice is still just very rooted in 1985. Instead of instead of them just forgetting that, like, just forget what happened before. And look at what what's possible now. It's just it's it's a, it's what slows people down sometimes. Now, I'm not talking about people who don't want to pump. Like I understand if somebody doesn't want a pump attached to them. Like I couldn't argue with that, if that's not what you want. I'm talking about doctors who are saying things like, I just got a note from a lady this morning and her kids graph is ridiculous. And she's like, I don't know, like what happened. I went to my endo and told them that we were seeing drops after meals and they made his basil heavier. And now the drops are worse, and I'm feeding his insulin all day long. And I said, Look, I looked at it, I listened to what she had to say. And I said I would put the basil back to where it was and look at your meal ratios because our first problem was the kid was falling after food. But I think the doctor saw the big spike and added basil for some reason, but the spike was from her catching the fruit catching the drop with food. It's just like, How could someone misunderstand this so drastically? You know and to say that they are professionals at it. i That's the That's today's biggest hurdle is getting practitioners who can read those graphs quickly and make sense of them.
Christine 49:59
Yeah, show I've, I've I've my last two internists that I went to and I go to endocrinology person, the last two internist, who were looking at my A wincy at a 5.6. And a 6.0. Said, I'm a little worried about this. A won't see that this is too low. But I see that you're working with endocrinology, and I'll just leave it alone. And I said, that's a good idea. Because I said, technology today is all about. I don't, I don't have to have extreme lows anymore. That 5.6 does not. When I had sevens. I had more lows than I do now. Yeah.
Scott Benner 50:57
It's obvious to me, I don't know why it's like the if you don't get high, you don't have to correct and then you don't get low later. It's, uh, you said earlier that the five six felt effortless. And I mean, my heart just swelled. Because, I mean, if you've listened to the podcast, you know how I think about it, if you don't get high, you won't get high. If you don't get high, you don't have to crack, you know, like you, you put the effort into staying in that spot. And then all that other stuff that everybody struggles with, most for the most part doesn't happen anymore. Your your insulins not timed poorly. It's not working when there's no food in your system, etc. Like all the things you'll hear me say in the podcast. But I was just really, it's lovely that you that that struck you that way too. And I just because you had gone through so many iterations of diabetes, why were you able to hear what I was saying? And how long have you been listening? And how the hell did you find a PA, I have a lot of questions. I don't understand how you find a podcast at your age. How did you find yourself listening to a person who doesn't have diabetes? Like how did you get over that hurdle?
Christine 52:00
Well, I'm so in the pump users support group that I'm currently in. When I first got on the Dexcom, with my tandem pump, I was going to this support group, and people were starting to use the mostly continuous monitoring with their med tronics. And, and, and some Dexcom. fours and fives, you know, and I never wanted to go on a Dexcom earlier because it was like, well, you still have to calibrate it. I was like, I will go on. I'll go on continuous monitoring, when I don't have to calibrate it anymore. Why would I want to do that and still have to test my blood sugar. So I was kind of waiting for the perfect opportunity. But in that group, when I got on to G six, that was my first continuous and, and then I had the chance to pump. I said, Okay, I'm getting all this data. I don't quite know what to do with it all. You know, how do I work with it. And one of the dieticians who ran that group, she says, you might want to listen to the Juicebox Podcast. And so I I didn't even know what a podcast was. So I don't learn how to do that on my iPhone. And I started listening to you and we that was back in. It was in the low 200 episodes, okay. And what the very first day I thought, I don't know if I can listen to this guy.
Scott Benner 53:56
My wife would agree with you.
Christine 53:59
kind of fool yourself. It took me one day to get over it. And I thought, oh my god, this guy has something to say. I mean, stick with this. And I had a job where I worked out of my car, I traveled as a as a home occupational therapist. So I had that podcast going on all day long when I was in my car. And I'd listened to episode after episode and I just started to eat it up and start to make slow changes. Cool. And then I was telling the group I said, you all need to be listening to this. This is really helpful information. And it made sense to me. The idea about you know, the struggle to bring down a high versus the ease and bringing up a low you know, and don't don't do 15 grams of carbohydrate. All you need are eight grapes to bring up that low? And especially if it's a low that you're moving into slowly, which is what happens on a pump, you know, unless, I mean, it's very rare anymore that I overdose on a Bolus. And even if that would happen, like I just don't calculate it right. Then it's like, oh, okay, I get to have a little chocolate right now. This little snack to keep me from crashing. That's excellent. Yeah. So, um, yeah, it's just a whole lot easier. So and I, yes, I attribute my 5.6 to you.
Scott Benner 55:51
Oh, well, I'm very happy for you, sincerely. I, I know I, I know how I can probably come off in the beginning. But there's nothing. To me. There's nothing you can do about it also needs to be interesting. I, you know, so it's always been, it's always been in the back of my head, you know, that you can't just, you can't just pump out the information in the driveway, no one will listen to it, right?
Christine 56:17
Do you remember when I first wrote to you, like six or seven months ago, and I said, I think I have something to contribute to your program. And I said, you, you do such a great job of what we call in my occupation, of oath of occupational therapy. It's called therapeutic use of self. And you do that really well. And, and it allows you to connect with people. And it always allowed me to connect to my patients in a way that I did not see my co workers necessarily connecting. It's putting your whole self into it. It's putting your experiences to develop a connection and rapport between you and your listeners, between you and me, the person that you're interviewing, you just do that really well. You make you make people feel safe and respected. No, thank you. And that, and that is, I think, you know, that's kind of the fancy words to somebody who knows how, who knows how to do the gift of gab, and to be a really good schmoozer? You know, you've been told that by Who was it, Katie Couric that told you you have a good way with people? Was she the one?
Scott Benner 57:44
Yeah, she was the one she's, she's, she said, you don't know, I was doing her television show. And when it was over, she said, all those people, they were just, they were waiting for you to talk again. They didn't care what the other people were saying. And, you know, she's nice, like, I could feel it, like I have whatever that is, like, I don't know that anybody wouldn't have it. But when you're talking, and you can feel people moving, you can feel their emotions moving or their interest moving on your words, it's a, an electric feeling. And so I knew I knew that it was happening. But I didn't have the context for it that she had, because she had watched it so often, I guess, in the past,
Christine 58:22
and using humor, and storytelling, your personal experience, it's just all part of it. And it just makes people you know, believe in you. And connect. Difference between, you know, you as a really good podcaster and or me as an occupational therapist between somebody who's successful at it, and somebody who's just kind of doing their job, right.
Scott Benner 58:54
The way I the way I think about it, I mean, if we want to go behind the curtain, I guess is that I think there's something valuable about me not having diabetes, because of that sort of dispassionate breakdown that I can do of what's happening, you know, whereas if you talk to another type one, their emotions are going to get into it pretty immediately. I mean, I don't know what it's like to have a low blood sugar and think I'm going to pass out. It sounds really scary. And I hope I never have to understand what that's like. But I can stand as a third party and tell you what it was like to watch it happen, and where and what was important to do and when it was important to do to stop it or to slow it down more quickly, where to have it come back without a spike like that kind of stuff. I agree about the storytelling thing. I think people need to hear things slowly. I don't think having things shouted at you or bullet pointed is a valuable way to teach people things. And, you know, being comfortable is I can't even take credit for that. You know, I've got I won't say who and my family but we were sitting around one day speaking about something. And I started talking and being vulnerable about how I felt about the situation, which led to another person in the room doing the same thing. And those people were older, and it made their spouse uncomfortable. And then it started like a, an argument. And I remember at the end, I was not part of the argument. The person who opened up after I opened up looked at me and said, This is your fault. And I laughed, and I said, Hey, the two of you not knowing how to be honest with each other is not my fault. I was like, I don't know if you just saw what happened. But you were honest. It made your your your partner uncomfortable to feel that you were sad. And then you guys didn't know how to communicate after that. I said, that had nothing to do with me. But I take your point. There's something about I was honest. And then it made him want to be honest. And then it just it went on from there. So
Christine 1:01:05
instead of it being your fault, you could take credit for that.
Scott Benner 1:01:09
Oh, at the end, I was like, Yeah, I pulled you aside. I said, Well, you're welcome. You know, it's up to you guys. Now to third times, when I hear people complain to me, and in my head, I think, I think to myself, Oh, so what you mean here is Thank you. But you just don't know it yet. That's fine. And it really is. It's an odd pairing, right? Like, why? Why is it me? You know what I mean? But it all works, and I can't take credit for it working. It just works. And and then then that's the next step. If I pretend that's not the case, if I use false modesty, you're going to feel that. So I'd rather seem brash to you at first when you get to the podcast, and then you realize that maybe I deserve that feeling, then for me to pretend like oh, no, you know, that's not, you know, that kind of both, is. I think that that fake stuff would turn people off it, at least it would turn me off. So, you know, I don't do it, when you hear me get embarrassed about something. I'm really embarrassed. Like, when when people say nice things, it's, it is gotten easier for me to accept over time. But it's still strange. I mean, you're a person who over the last hour has painted an amazing picture of decades of living with diabetes. And to hear at the end of that story, for you to say that I'm in the fives because of a podcast I made is, it's difficult to absorb, from my perspective, you know, but I appreciate it. It just makes me a little uncomfortable. Maybe I'll be a full adult and other 10 years, and I'll be able to accept it better. I
Christine 1:02:46
don't know. Yeah. Well, I want you to know that with every episode I listened to, um, you know, some of the what do you call him the dark after dark? The after dark? Yeah. You know, somebody's talking about drug addiction and diabetes. And I think, Oh, well, that's, that's an interesting title. And, you know, I never did drugs, I'm probably not going to get anything out of this. But I've listened to all of them, you know, as they come up, and there's always some thread of information that I can get from even that episode. You know, um, you know, people talk about, you know, just the emotions behind having a chronic disease. And even though I don't suffer from depression, I remember some depressing times of, and I just can, every episode, it just brings me back to so much history that I just love, you know, kind of that that piece of it where I am constantly reliving some things or remembering some things that I totally forgot.
Scott Benner 1:04:14
Well, there can be value in other people's perspectives. That's obvious, but there can also be value in you hearing somebody say something that's clearly wrong. And it can reinforce it. And you I mean, there. I don't agree with everything everybody says when they're on the show, but I don't stop to you know, I don't always stop to give my perspective that's, that's opposite sometimes. You know, sometimes the people who come on have to realize that by being so open and honest, there are going to they are going to reveal things about themselves that aren't maybe stuff that you would help other people to see. But by letting other people see those things, you end up helping those people. I just got a note about something like two days ago where a woman said hey, in this recent Episode when this person said, you know, XYZ, how come you didn't correct her? And I said, Oh, she seems really, you know, sure about that for herself. But what I hear is then the person who thought her right in about it, that helped them because it solidified a thought they had. And so there's this sort of, there's this bigger there's a bigger responsibility in bringing people's stories out than it might seem to just the casual listener. Right, there's, I'm, uh, I'm trying to accomplish more things. And it might seem like, I guess, it seems kind of high minded for a podcast, but it's actually true. So yeah, yeah. I appreciate that. I appreciate that. You enjoy it? I really do.
Christine 1:05:49
I do. I do. I'm not I'm retired, right before COVID. From the most, you know, the fullest part of my job, I still do a little two hour a week job as a part time employee, but I'm not in a car anymore, driving around. And all day. So I realized, Oh, my God, I'm not listening to as many podcasts, I have to create some other time, besides being in the car, to be listening to the podcasts,
Scott Benner 1:06:24
you know, and when COVID came, I was so worried that that is what was going to happen, you know, that, Oh, gosh, people are going to stop driving. And you know, this is it. Like, I actually, I was worried, like, you know, will the if the podcast, you know, could fold if people don't listen, advertisers won't be, you know, inclined to advertise. If that happens, you know, good luck, all of you with me explain to my wife that I'm now just making a podcast for all of you out of the goodness of my heart, because we have bills and children and college and things like that. And then the opposite happened. So it just it skyrocketed through COVID. And I was like, huh, that went backwards. But your experience was the experience that I expect it? And and I'm sure it happened to some people. But overwhelmingly, what happened is that people found themselves with more time.
Christine 1:07:14
Yeah, so that's good. That's good.
Scott Benner 1:07:17
It's good for me. Because because I want to make the podcast, I'm in a very weird position where I do a thing that helps people. And that is my main focus. But that thing takes so much time and effort that if I can't monetize it, I can't do it the way I want to do it. And then it becomes, you know, it could become difficult to maintain after that. I just feel lucky that I make money off of a thing that's actually valuable to people and that I enjoy doing. Like, I never thought I was gonna get all three of those things like enjoyment value and a living. I didn't I didn't think I could get all of them. So I feel very lucky about it. Yeah, yeah. Having said that, you need to listen more, Christine. Okay, I do.
Christine 1:08:03
I'm gonna have to learn how to like, turn on the podcast and sit, sit in my office hear that? And I I'm a quilter. So I can have it on while I'm sewing. And so, yeah, there's all kinds of ways. Anyway,
Scott Benner 1:08:24
are you enjoying yourself? Is this okay? Did you get out everything you want to talk about?
Christine 1:08:28
Um, yeah, I think there was one. This might give you a title. Today, I do. I am going through one. I call it a minor complication. You know, my cousin went blind when he was 21. And he's, he, he would have been 65 this year, but he died two or three years ago. From all of the complications of diabeetus. He the diabeetus was kind of from both of our mother's sides. And then his father had early heart disease. So he got the double whammy of having not only diabeetus but a cardiac condition as well. So over his lifetime of 62 years, he had three or four heart attacks he had bypass surgery. He was having kidney shut down he lost his sight he lost a leg and you know, he was pretty much heading into another surgery with it for another amputation and and he died. But I have always because I was involved in that I study in college knew right away to kind of make sure that my eyes are being checked every year and been faithful about that. And I remember, you know, the very first time having the physician tell me Well, we're seeing a little bit of background diabetic retinopathy. But it's kind of what we would expect to see in somebody's eyes who's had diabetes for 30 years, you know, you don't have anything to worry about right now, and but just maintain control. So it's another reason to maintain good control, I had a cousin who was blind and, and then I had a little bit of retinopathy. Well, so as the years went by, you know, that little bit has changed. And I'm undergoing treatments now. For it's called diabetic macular oedema, D and E. And they go in, it started out being every month, but now it's every other month for I call it my time to get the sharp stick in my eye. So I get an injection of, you know, a very fancy, expensive drug called eylea. I see advertisements for it on TV now. And it is something that I'm probably going to have the rest of my life, but it controls the edema that can, without the injections, the edema can get worse, and then it tugs at your retina or something like that, you lose your sight. And so, you know, had that been there, you know, when my cousin was in his 20s, he wouldn't have lost his sights. And now I'm at that place where, you know, at first was like, Oh, my God, I have to go have this treatment now. And instead of going down the rabbit hole of, oh, this is terrible and getting depressed, it's like, hey, we have a treatment for this, I am not going to lose my sight. I just have to go in and get a sharp stick in my eye every two months, you know. And so, again, I've heard you talk about with your daughter of how you know how much you know, you tell and make decisions, and you guys text and you tell her what to do. And at first I thought, wow, she's a teenager, she should be able to do all that because I, I, I right off the bat learned how to do all of that my mom was kind of incapable, she would just crumble. And so I had to learn how to do that at an early age. And then I could hear you talk about all the things that you did for Arden. And I thought, wow, she doesn't have to make those decisions. Isn't that? Wow, I wonder when she's going to learn that. And then I thought, hey, if somebody texted me and said, Hey, take five units of insulin, and you know, what are you going to eat? I thought that was pretty nice. Maybe I'd like that too.
And she, and then you talked about, hey, by the time she does have to start learning that by herself, there's going to be more technology out there. So that she may not have to be learning all the things that I do for her. Right, the technology is going to change again and again and again, because it is changing so rapidly. And so I guess the point being like with complications and like this eye disease, I decided not to get all bent out of shape about Yes, I've got this thing going on. But for God's sakes, I've had diabetes for 52 years. Because it's dead. I could be dead and I'm not. I'm doing very well. I have been on the same dosage of insulin from almost when I was a teenager that I am now. You know, I take care of myself, I exercise I stay slim. And I eat well. And we I have every reason to believe my doctor says, you know, you might make the 100 year club happy amazed and I and I know and I know. Some days I think yeah, that's possible. I've I feel like I've been lucky. And I've also worked very hard at it so it's hard to know how much is hard work and home He has some stroke of luck.
Scott Benner 1:15:02
Well, you gotta take what? You gotta take it. Right, right. It's a little, it's a little luck was coming your way. I mean, that's amazing. And maybe there's just something about your body that that did well through those early years and didn't feel the the impact as much, I have to tell you the two things. I was like, as soon as you talked about the injections for your eyes, I just thought, well, that's a miracle that somebody figured that out, you know, like that that exists is just, it's just wonderful. Yeah. And does it hurt? Does the needle hurt? What? How would you describe the injection?
Christine 1:15:37
Um, so the very first one I went in for I said, to the retina, RetinA, but he's a retina specialist. I said, you know, I'm a little I don't get anxious. But I said, I'm a little anxious right now, because you're going to put something really sharp in my eyeball. And I mean, nothing. There's nothing about that. That sounds good. And he said, Yeah, and I'm going to tell you right now that you having anxiety is not helpful. So he says, I'm going to help you breathe through this. And he really put me at ease. And he is very skilled, and very fast. So that, and they put these numbing drops in your eye. So I don't I feel something. But I'm sure not as much as it would be without the numbing drops. And it just goes so fast. And then he's done. And then they rinse your eyeball out. And then you go home. And he says, the best thing for you to do right now is to go home and take a nap. Keep your eyes closed for a couple hours. And because generally, what happens is I feel the prick. And then on the drive home, my eyes starts to feel really scratchy. And I go to sleep. There's something in it that makes me sleep for two hours, I could never take a two hour nap. But I sleep for about two hours. And I wake up and it's pretty much gone. Well, the it's just a slight irritation. And till the next day, I don't even know it. Yeah. So you just have to kind of get over that. Yeah, they're gonna poke your eye for the needle.
Scott Benner 1:17:30
And then the rest is cake. Yeah. And the other thing I want to tell you, and I do have to let you go in a minute, just because I'm running up on something. But the other thing I want to tell you is that I just got back from a wedding, my wife and I drove cross country to go to my god daughter's wedding. And I of course, didn't say this out loud before we left, but Arden stayed at home by herself. And we left Thursday afternoon and returned late Sunday night. So with the exception of one evening, where I'm gonna say we were between the end of a pot of a pump site, where I wish maybe she would have changed the pump a little sooner, and some hormonal things. You know, so there was a struggle, this one for about 112 hour period. And her her blood sugar was higher during that time. 100 ad 200. And but I let her keep going at it. And then once in a while I jumped in. I was like, Hey, you gotta do something here. You know, like, this isn't it's not going to break. You know, you have to do something I already Bolus. I was like, I know, but it's not working. Like, look at the line. It's not it's not working, you know, and then I nudged her towards, I think your pod should be changed. And she said, It's not the pod because I was it worked earlier, she said, and I was like, I know I'm like, but there's this entire experience that we're having right now says to me, we're seeing some resistance and the pump site's not fresh. So I said, I think if you go to a fresh pump site, we're going to start and we make a nice big Bolus, I think this is going to be okay. So she said, No, I want to, I'm gonna do it in the morning. I said, Okay, well, that's fine. But then we're going to make one more big correction. And I said I, because I think we can push enough through this bed site to keep you safe while we're asleep. And she guessed that how much insulin and if the site was working, right, she would have had the right number, but I knew to do much more. So I pushed six units through as a correction for like a 200 blood sugar. But that's based on everything I'd seen over many, many hours. And she got up in the morning, changed her pump and got everything back the way you know again so to me that's a learning experience like she gets to see that happen. And and, and I do believe what I say which is a oversee slowly over time. She's learning more than she thinks she knows. And I do think things are going to continue to get better. And it'll be a different situation for her in the Future.
Christine 1:20:00
Oh, she's gonna she's gonna figure it out as she leaves home and goes off to college that she's going to be on her own. So figure it out, and so she won't do. You know, she'll have some bumps along the way, but slowly
Scott Benner 1:20:13
expected. However, in the many years prior to that, I mean, I think we're up to seven or eight at this point, like, imagine how crazy it is. I've lost track of how long Ardens a onesies been in the fives, I don't even know. And because it feels effortless at this point. But But even at that, if she got eight years of a five point something, a one C, and she's learning how I did it. Slowly without it feeling like she's not pressured by I don't know if you heard the episode with her. Like she couldn't be more chilled out about it. So yeah. So you know, so there's no pressure. She's having good outcomes. She is learning more than she thinks she knows technology is going to get better and moving forward. I mean, I did my best to put her in a good position. So yeah, that's all. Christine, I have to tell you, this is really terrific. I could probably talk to you all day, I am going to go jump onto another call right now. My son has a doctor's appointment that I have to sit in on. Or else the report back we'll get from it. As Doctor said, it's fine. I mean, like he didn't say anything else. That's it. It's okay. How about if I have it if I'm there, too. I really appreciate this. Thank you so much.
Christine 1:21:28
It was it was great. Thank you for letting me come on. And yeah, wonderful.
Scott Benner 1:21:34
Yeah. Well, and hello to your support group, because I'm assuming they all listen to you. And you they listen to the podcast now. So
Christine 1:21:40
yes, I told them. I need to start listening to you. I tell everybody about it.
Scott Benner 1:21:45
So thank you. That's right. All right. Hold on one second, please. Okay, I'm just gonna
a huge thank you to one of today's sponsors, G voc glucagon. Find out more about Chivo Capo pen at G voc glucagon.com. Ford slash juicebox. you spell that GVOKEGL You see ag o n.com. Forward slash juicebox. I just want to take a moment to thank Christine for coming on the show today and sharing her story. I really really enjoyed our time together.
last bits, tea one day exchange.org Ford slash juice box. Take the survey Juicebox Podcast type one diabetes on Facebook, join the private Facebook group. I'm just gonna non sequitur. All these enjoying the show. Tell a friend or a stranger doesn't matter to me. If you really love the show, try leaving a review and rating where you listen like say you listen to an apple podcast, open it up and say five stars. Click and then it says write a review that you click that and then write a nice thoughtful review that will make somebody else think you know this bill from Paris who wrote this review. He really seemed to like this podcast. I'm going to check it out to see what I'm saying about the reviews. That's what they're for. And last but not least, I didn't mean to connect these two things because I was supposed to non sequitur the whole thing. But last but not least, if you're listening in a podcast app or an audio app like Amazon music, Apple podcast Spotify, please subscribe and follow the show. Some apps ask you to subscribe to be a follower. Some apps ask you to follow to be a follower. Fancy words. Not really. But they mean the same thing depends on the app you're in Subscribe and follow. Subscribe and follow. You can pill the digit forget about the 666 thing already. There's only an hour ago. I am your master. You will do what I say. Subscribe and follow. leave a review make it five stars support to sponsor by a contour meter. You need a different glucagon. Your tubing is stinky. Don't you want to see your CGM numbers on your phone? Raha right it's enough just to purchase sponsors. I gotta keep this thing going. Thanks so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#665 Type Two Stories: Leanne
Leanne has type 2 diabetes and a daughter with type 1 diabetes.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 665 of the Juicebox Podcast.
Today we're going to be speaking with Leanne. She's an adult living with type two diabetes. And I am genuinely excited to bring you this conversation. I'm going to explain why after the music. But for now, I just need you to remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan. We're becoming bold with insulin. If you're a US resident who has type one diabetes, or is the caregiver of someone with type one, I need you to go to T one D exchange.org. Forward slash juicebox and fill out their survey. That's all I need you to do. When you do this, you're going to be supporting people with type one diabetes, you'll be supporting the show and you'll just be doing a good thing. The survey is completely anonymous, HIPAA compliant, and it's not hard. I mean, you take those little buzzfeed quizzes, this is way easier, and it actually helps somebody T one D exchange.org. Forward slash Juicebox.
Podcast this episode of The Juicebox Podcast is sponsored by the Dexcom G six continuous glucose monitor, learn more, and find out if you're eligible for a free 10 day trial@dexcom.com forward slash Juicebox Podcast is also sponsored by Omni pod makers of the Omni pod Dash. And they have a free trial that you also may be eligible for theirs is 30 days long. On the pod.com forward slash juice box, find out if you're eligible for that free 30 day trial of the Omni pod dash. Okay, before we get started, let me just tell you that for a very long time, I've wondered and wondered about how to help people with type two diabetes have witnessed people with type one benefit from community. And from this podcast, from the feeling that they're not alone from others being willing to share what works for them. And it's, it's been life changing for people with type one. I've also seen plenty of entities try to start type two communities. And they never take off. I mean, I'm sure they're lovely for the people that find them. But they never get wide enough to to throw a net that can catch people and bring them in. After I've seen what this podcast has accomplished for type ones and and how far it's traveled. And how willing the listeners have been to share it with doctors and friends and strangers online, anyone who they think it may help. I've come to believe that this is a special group of people. And I think we all know someone who has type two diabetes. So I'm going to start sharing stories of people living with type two diabetes, and I'm going to count on you the listener to try the episode, even though it might not have anything to do with you. Maybe your kid or you have type one and I don't know, I'm just hoping you might you might dive in and and listen and hear these people's stories and, and share them with others. Because I think this is how we build a valuable type to community. And I'm gonna give it a try. So if you're up for helping, check out Leann story today and share it with someone who you know, that has type two diabetes. I'm kicking off this series, which by the way, I'm calling type two stories with Leanne, because she was just delightful, and I had such a great time talking to her. And she shared what her life with type two is like. And there'll be another episode coming up soon with John. And hopefully, if you have type two diabetes, you might hear this and think I'm going to add my voice to that as well. Please reach out if you have type two and you want to be on the show. I want to talk to you. I want to hear everybody's stories. What it's like to live with type two, the confusion, dieting, exercise, what it's like to talk to doctors, friends, family members, the whole thing. I want to weave a generous and A rich tapestry so that others can understand what type two is like and so that people living with type two may find this is my hope that they may find the commonality and the answers that they need to live better with type two.
Leanne 5:19
I'm Leanne. I'm a type two diabetic and when type two cents? Well, I the first time was gestational diabetes in 2006. And then I was diagnosed in 2009. With diabetes.
Scott Benner 5:35
Okay, so you've had type two for like, a dozen years. Yeah. Oh, yeah. All right. So you're definitely a type two?
Leanne 5:43
Yep, definitely. I've been tested. My daughter's type one. So we did all the testing and everything's negative.
Scott Benner 5:52
Okay. When When was your daughter diagnosed with type one?
Leanne 5:56
Um, August of last year?
Scott Benner 5:59
Oh, recently. Yeah. At what age?
Leanne 6:03
1212.
Scott Benner 6:04
Okay. Are you? Are you drowning a puppy? What's going on back there? I just heard
Leanne 6:11
I'm drowning in a puppy.
Scott Benner 6:14
I just know it. Do you have a puppy?
Leanne 6:19
Yeah. My son. My grandson has a little pug for his emotional support animal.
Scott Benner 6:29
Oh, no kidding. That's a That's a? I mean, as long as he doesn't mess up the podcast, I don't care one way or the other. Okay, so how old are you now? Alien? I am 52. Tomorrow. 52. You've had Oh, happy birthday. Thank you. Congratulations. So a dozen years since you're 40 type two, we'll probably get to your daughter at some point. But I want to really start with you. What, how? I guess what, how, what do they say to you when you have diabetes when you're 40? Like what kind of like direction do you get from a doctor is my question.
Leanne 7:10
Well, they, when I was pregnant, they put me on insulin. I went straight to insulin. And then after my daughter was born, they tried the insulin with metformin, and glipizide. All kinds of all kinds of I mean, I've been through the whole rigmarole of pills. I was on a sliding scale of insulin. So I took 10 units with every meal and did just wasn't working. But was it they kept saying they kept saying that I was non compliant.
Scott Benner 7:52
What does that mean? You ate more food than they gave you insulin for or less food and you gave insulin for
Leanne 7:58
it? I guess. I don't know. I did exactly what they said they would say. Now we said to eat, you know, between 60 and 80 carbs per meal. Well, I thought that was kind of a lot. So I wasn't even eating that. I went very, very low carb. I actually did the 500 calorie diet for a while. Wow. I lost 100 pounds. And still insulin resistant, you know. So I, I went through their rollercoaster ride for for 12 years.
Scott Benner 8:39
We ended they call you noncompliant for eating fewer carbs than they asked you to eat.
Leanne 8:44
They just because my blood sugars would stay around 500
Scott Benner 8:49
Oh, okay, so you were eating? Oh, no kidding. So you needed more insulin? Nah,
Leanne 8:56
I needed a lot more.
Scott Benner 8:59
And they were like, just take a little bit of this with your dinner. And then when your blood sugars came back, they just figured you weren't taking the insulin at all. But you are. Right. I understand. Okay,
Leanne 9:07
or the or the pills. So, but I was I was doing everything they told me to do. And they were it was kinda like, they were thinking that I couldn't be doing it because my blood sugar's were still so high.
Scott Benner 9:22
I don't understand why somebody wouldn't believe you if you told them what you were doing.
Leanne 9:27
Oh, I don't know. I guess. They figure you know, type Q if you're really doing these things, and you shouldn't have any problem.
Scott Benner 9:35
Yeah. No, they weren't right about that. Were you just seeing a regular general practitioner? Yes. Okay. Do you still see the same doctor?
Leanne 9:46
No, no, I was diagnosed when I was living in Alaska. I was I was seeing my my, the doctor that my mother saw for her diabetes.
Scott Benner 10:00
Okay. You're Dr. Methuselah Is that who you were saying
Leanne 10:10
you know, we back then we did the best we could we had we had the the intermediate I call it insulin, you know, the cloudy stuff, you got a roll in your hands. We did the best we could with what we had, you know, and there wasn't a whole lot of and there's still not a whole lot of education around it. So
Scott Benner 10:32
no, I know it's one of the reasons I want to talk to some more people with type to to shine a light on the fact that I don't think you guys are given very good information at all, but most of the time, and you said you lost 100 pounds with your with your shifting. And did that change your insulin needs?
Leanne 10:51
No. I'm still a one to four carb ratio.
Scott Benner 10:57
Let us be fair, did you go from 1000 pounds to 900 pounds?
Leanne 11:02
No, no, no, no, no, I, I am about 165. Now Wow. I'm a firefighter EMT.
Scott Benner 11:12
Okay.
Leanne 11:16
homecare aide and I CNA.
Scott Benner 11:18
You're pretty active during the day, then?
Leanne 11:21
I'm very active area. Okay. And I have a little farm.
Scott Benner 11:25
Alright, okay. Let's see, people share your details with me. We're never gonna get the other stuff out. But what do you mean, you have a little farm?
Leanne 11:31
Um, well, we have we have goats and chickens and horses and dogs and cats and lizards. And so I'm constantly repairing fences or feeding animals and mucking stalls, you know? So it's not like I'm sitting on my button lazy all day.
Scott Benner 11:50
I know, you're busy and you're moving. You just, you're just resistant to insulin. Very, and your mother had type two as well? Yes. Okay. My mother, my sister, my grandmother. Was there anything to really? Your mother, your sister, your grandma? So everybody? Is there anything that they did that was successful that you were able to mimic? Or do you guys not even talk about it? Like, how was it discussed?
Leanne 12:16
Um, well, my my mother passed away in 2007. From diabetes from complication of diabetes. Okay,
Scott Benner 12:28
what was the complication?
Leanne 12:30
My sister has kidney disease.
Scott Benner 12:33
What was your mother's complication?
Leanne 12:36
Well, she went blind. She she ended up with kidney cancer. And the treatment for kidney cancer just pretty much wiped her out.
Scott Benner 12:47
Gotcha. And yeah, and now your sister has kidney disease? Uh huh. And this is from her diabetes as well. Yes. Okay. Are they as apt? Were they as active as you are?
Leanne 13:00
No. I don't think anybody in my family so in fact,
Scott Benner 13:08
there's no way to be as active as you are.
Leanne 13:14
Like the Energizer Bunny, man,
Scott Benner 13:16
how would you describe living with type two? Like, I mean, from a perspective of, I think, first your information that you have like, like your set of marching orders, instructions. What is that like?
Leanne 13:33
Well, it's, there's pretty much I mean, all the information that we were given is wrong. If you ask me, it's all wrong. Okay. Oh, how so? Um, when my daughter was diagnosed, I threw out all my pills, I threw out everything. And I started from scratch. Because a light bulb, I was talking to the diabetes specialist, she said, Well, you know more about all this than than I do. And I was like, and that's when a light bulb went off. And it was like, Okay, we're gonna start over. So I I found my, my basil. And then I started working on my insulin carb ratio and my sensitivity factors and from there I went to the doctor and she's like, I don't know what you're doing. But you know, I mean, my a one C went from over 14 down to 5.6.
Scott Benner 14:39
No kidding how and how much time
Leanne 14:43
and five months and this was
Scott Benner 14:45
after you watched your daughter have type one. So what were you watching about the type one that made you think I could be doing this for myself?
Leanne 14:53
Um, well, it just made sense because you know, I know how insulin works and and I knew that I knew a lot more than I thought I knew. Because I was listening to what the doctors were saying, Here, take this here, do it like this, do it like that. But until they started talking carb to insulin ratio and Basal rates, that's when the light bulb went off, and I went, we're doing this all wrong. Because no matter what I do, I'm insulin. You know, I'm,
Scott Benner 15:27
it doesn't feel like you never, you never have enough insulin, and you definitely most assuredly need it. It's not just enough to take a pill. Right, right. So well, how did you learn for your daughter? Like, what was that process like she's diagnosed? And then who teaches you how to take care of her?
Leanne 15:46
Um, nobody. I mean, you're the podcast, I just started listening to the podcast. Oh,
Scott Benner 15:53
okay. I thought maybe you got some, like great information from a doctor and you started using it for yourself. But
Leanne 15:59
no, no, actually, when when I had the meeting with the diabetes educators, she said, Well, you already know everything you need to know, you just need to know how, you know, you need to apply it. Okay. And that's when it dawned on me that, you know, if I'm producing insulin, but I can't use it, what's the difference with her not producing insulin and needing it?
Scott Benner 16:25
Yeah, nothing really. I mean, the the end result is, is that you don't have insulin and you need it.
Leanne 16:30
Right. Right. So I mean, I might not go into ketoacidosis but or have lows without, you know, without insulin, but, you know, she's, she's 12. And she needs insulin. And I thought, I just thought, wow, you know, this makes sense that if I were to treat mine just like I treat hers, maybe we'll get somewhere
Scott Benner 16:57
right. So you were so now are you using a Basal insulin and a mealtime insulin?
Leanne 17:03
I am actually right now looping with the pump with Omni pod.
Scott Benner 17:07
Okay. All right. All right, Leanne. Okay. All right. So you just basically were like, Alright, everyone's got diabetes, minds going terribly. Then she gets it. Was there any fear there? Like when she got it? Where you're like, God, I can't even take care of my own. How am I going to take care of hers?
Leanne 17:28
No, because you know, that Mom Brain kicked in and said, All right, this, this has got to stop. gotcha. I gotcha. So you've got to live a long time now, you know, right, right. When I'm 55?
Scott Benner 17:40
Well, at the very least, yeah. We need you to stay around and stay healthy. When? So, alright, well, how do you find the podcast?
Leanne 17:51
I actually joined another Facebook group. And they somebody in there mentioned it. And so that's where I went.
Scott Benner 18:00
Okay. All right. So you went there. You learned about the show, went and checked out some episodes, watch some people online talking about diabetes, took it back applied it to your daughter, and you were having How long did it take you you just said but I forget the time frame. You got it? You got it down pretty quickly, right?
Leanne 18:19
Yeah. She was diagnosed August 12. And by It was November November 7, my agency was down to I think it was seven. And then in December, or January, actually, I had it down to 5.6. What about hers? Hers went from 12.9 to 6.1.
Scott Benner 18:56
No kidding. In a similar timeframe. Yeah, yeah. Huh. How would you describe your diet? Is it is it still low calorie? Or is it low carb? Is it pretty average?
Leanne 19:13
It's pretty average. I mean, we mostly eat like farm to table type because you know, we're 25 or so miles away from the nearest grocery store. Okay.
But you know, we have we have bread, we have cookies.
We have the normal things. I've never been one to buy a lot of chips and high fat high carb stuff anyway. So, I mean, you know, we go out to eat once a week and we definitely load on carbs then.
Scott Benner 19:48
Gotcha, but you're eating like, like, quite honestly the vegetables, meat. Things that you've raised yourself? Yes. Okay. 25 mile was from a grocery store. I am three miles from 25 grocery stores. I think just I just realized, as you were saying, and I was like, There's no end to how many grocery stores I could get to within a couple of miles. Are you just out in the you're just in a more rural area?
Leanne 20:16
Yes, yes. We live. Like I said, 25 miles out from a small town.
Scott Benner 20:25
So you're not 25 miles away from a big grocery store. You're 25 miles away from just having access to anything? Well, yeah, yeah. Yeah. That's interesting. How do you like living like that? I mean, you were in Alaska prior. Right. So you're used to being rural. But
Leanne 20:43
yeah, but in Alaska, I lived right there in the university. District. I see. I mean, I was right across the street from the hospital in the college.
Scott Benner 20:50
You were more. You were more near things in Alaska. And you are now where you are. Right? Do you enjoy it?
Leanne 20:58
Oh, yeah. Oh, yeah. I don't like to be bothered. I don't like people nowadays.
Scott Benner 21:03
You don't want to be bothered by people? I know what that feels like. Is that scary? Or like, how do you get your insulin?
Leanne 21:13
Um, I drive to town.
Scott Benner 21:16
Somebody's not mailing it to you? No,
Leanne 21:18
no, I drive to town. I don't trust the mail. Because we never know when we're gonna get it.
Scott Benner 21:25
Oh, it's it's not? Oh, I see. Okay. All right. C drive. And then are you in your daughter using the same kind of insulin are using different kinds?
Leanne 21:34
No, we use the same kind I made sure. I tried to keep us on the same dechaine Just so that we don't run out. And it's interchangeable.
Scott Benner 21:41
Yeah, that's a good idea, actually.
Leanne 21:45
So whatever she goes to, I'm gonna go to
Scott Benner 21:48
how were you able to get a doctor to prescribe an insulin pump for you?
Leanne 21:53
Actually, I just called up Omnipod. And I called my doctor and I said, you need to approve this, because this is what I'm doing. And she said, Okay. Once Once I started bringing my a one C down. She was like, whatever you want, and whatever works.
Scott Benner 22:08
Oh, okay. So you showed that you knew what you were doing? And then she kind of got away?
Leanne 22:14
Yep, yep. She's like, she's asking me what, what I need, what I what I want what I need, because she, she doesn't know a whole lot about him.
Scott Benner 22:26
That's something I love that you just, you know, I've I've said before, under my breath, maybe out loud a couple of times, just call the company get a process started. And then just put the pressure on your doctor to just sign off on it. You know, for the people who are like, Oh, my doctor says I have to wait a year, whatever they say.
Leanne 22:44
I wasn't I wasn't about to take any of that. You know, they say that you have to have your blood sugar's under control, before you can do anything. But the way they're, they're giving you the the instructions, you're never going to have it under control like that. You know, I can't take 10 units for five carbs or 10 units for 60 carbs, that makes no sense.
Scott Benner 23:13
So they give you this this goal to get to, and no instructions or tools on how to get to it and then tell you if you get to the goal on your own, then we'll give you the thing you really need. Right? Yeah, and there's no way that's gonna happen. Right? It is an interesting situation. I do wonder what the thought, well, you know, sometimes you wonder what people are thinking you find out they're not thinking anything? Yeah. I was just wondering, like, what the thought process was there for how do you how do you tell somebody, you know, I need you to jump over this wall. And then hide the ladder from them. Tell them the only way, you know, the only way they're allowed to breathe or eat is if they get over the wall? It doesn't it doesn't really make any sense at all. Actually, no, the entire thing doesn't make sense. Because I'm not saying like, I mean, I hear your story. And I'm excited for you that you found something that works. But I'm not even here saying like type two should just always be on insulin or always should be in an insulin pump. I'm saying that there's something that's going to work for everybody could be for some people, it could just be diet and exercise. For some people. It could be, you know, an oral medication and diet and exercise or, you know, maybe some people like you just need the insulin doesn't matter if you lose. I mean, my goodness, you know, almost half your body weight. And right still didn't help you. So, I mean,
Leanne 24:31
they say on the average, if if you're pre diabetic or just diagnosed with diabetes, if you lose on average, 30 pounds, you you'll, you can, quote unquote, reverse it. Well, that's not really true
Scott Benner 24:47
for you. I mean,
Leanne 24:52
even for a lot of people because they're still going to be insulin resistant when they eat carbs. Yeah, so you can eat a low carb diet. I mean, if you don't eat carbs, you won't need insulin.
Scott Benner 25:05
Do you need your basil? From the pump? Whether you're eating or not?
Leanne 25:10
I? Yeah, my basil is running 24/7 How much? Why get like 84 units of basil a day right now?
Scott Benner 25:18
Wow, no kidding. Are you using? Like you 500? Or something like that? Or are you? Nope, no,
Leanne 25:24
I'm using the just the 100 I tried to get the 200 but my insurance is really having a cow. So instead of doing that, I just told my doctor I said, well then just prescribe the Omnipod change every 24 hours.
Scott Benner 25:44
Okay, and you do you put a new pot on every day?
Leanne 25:47
I don't. I try to to cuz I only usually one mill a day. I run on coffee. And, and so I'm averaging about 125 units a day.
Scott Benner 26:04
Okay. All right. So you're making it 1820 hours. Something like that change? Yeah,
Leanne 26:09
I'm making it usually about 36 hours. Thanks.
Scott Benner 26:13
I'm sorry. Yeah, I don't know. I just did the math backwards there. Okay, well, yeah, you know, it's funny for some people were like, Oh, I can't believe I have to change my pump. You know, it won't. It won't last the whole time. Like it, it lasts as long as it lasts. You still don't have to give injections during all that time, right? And you still get the benefit of the pump running your basil. And it's a right. It's you don't even see that as a problem. Right? You just see that as what needs to be.
Leanne 26:38
Right. You know, and I like, you know, because I'm looping you know, it'll self adjust. So if my insulin needs go down, my pumps gonna fix it.
Scott Benner 26:48
No kidding. Are you on the auto Bolus branch are on the way on the pizza branch that does the by basil.
Leanne 26:58
I have the auto Bolus branch too. Okay, or whatever that is. That's great. I have the option. I was doing it for a while.
Scott Benner 27:07
Did you not need it? Do you not need the auto ball thing?
Leanne 27:11
I'm not usually I work. It works pretty good. Like right now I'm running it, you know, 89 I run? I don't get over 120 anymore ever. Unless I'm really stressed or something
Scott Benner 27:26
really stressful. You mean? Like, like a sheep ran away or something like that?
Leanne 27:32
Like, like, a teenager. So you got kids together? And I'm biting my tongue really?
Scott Benner 27:40
Well, yeah. Listen, if you're gonna tell me you live on a small farm, and you expect me to make fun of Canadians when they come on, then I gotta get what I mean, I gotta equal time. How do you feel versus how you felt prior has had any impact on your just your day to day life and energy in
Leanne 28:01
tons? I mean, before if I if I was to play in my house, I might have to lay down and sleep for two days. You know, I my whole body ache all the time. And once I, once I got the insulin and mean that my body needed, man, I have energy that just won't quit.
Scott Benner 28:24
Good for you. No, I cursed. I didn't mean to charge. I'm so I'm so thrilled because, you know, I don't know if it comes to surprise to you or not. But it's incredibly difficult for me to get type twos to come on the podcast. Like it is not easy. I try and I try and there's just not many of them that are willing to do it. And I think it's because, well, why do you think it is?
Leanne 28:50
I think it's because there's such a stigma. And they're, they're so used to everybody judging.
Scott Benner 28:55
Oh, gotcha. Okay. I always thought it was because they don't know what to talk about. Because I don't think anybody understands their time, too. Well, maybe, you know,
Leanne 29:04
the question is, do they have good control? I mean, or are they kind of floundering out there? You know, I mean, I see. Well, I was just responding to a post on your, your page. And it's so many people just don't know what to do. I know, because they've been given bad information,
Scott Benner 29:27
or no information, or none. Yeah, I just interviewed a guy the other day. I don't know when it'll come out. But it was interviewed or interviewed. He was diagnosed as a kid like in his teens and just no one to help them. You know, and he lived for so many years, not even understanding the simplest things about his diabetes and had a real horrible impact on his life and
Leanne 29:48
right, I was fortunate that even with my blood sugar's up between three and 500. I don't have any long term effects. My kidneys are good. I don't have any neuropathy. I was starting to get around 50. And then it went away when my insulin got adjusted,
Scott Benner 30:06
we ended your daughter getting type one diabetes kind of save your life.
Leanne 30:11
I think so. Yeah, that's I tell her all the time. And she's like, well, we're buddies now. And I said, in more ways than ever to are all the time. You know, you you if it hadn't been for you being diagnosed that I don't think I would have, everything would have clicked,
Scott Benner 30:27
right. Yeah, don't give her too much power, though. It'll go to her head, but I hear what you're saying. Like, that's gonna be like, I did save your life. I'm like cleaning my room. Well, that's it's so the really super interesting thing about talking to you is, is it there's no discernible difference between your story and a type one story.
Leanne 30:50
Right, other than I know, you know, like I said, we I won't go into keto acidosis. But
Scott Benner 30:57
sure, yeah, your body's gonna hold off a little, like, hold it down to some degree. Right. And if you stop eating your blood sugar comes back down ish. Eventually, I imagine
Leanne 31:07
is I so what I had to do, I mean, even on my basil, you know, I was on she had me on like, 30 units a basil. I was still running over 300. So I started titrating, my basil up until my blood sugars in the morning, were under 150. Okay, and I, I left it there for a little bit. And then I went down under 100. And I left it there for a little bit that I went down to about Ed.
Scott Benner 31:41
Lee, and you and I Jive right. You get me, don't you? Yeah, I could tell you. What's your total Basal for a day? Because I have a guess at 484. Wow, that is, but it must have taken some real nerve to get to that number. Hmm. Like you must say, You're a little ballsy doing that is what I'm saying? Like that's, well, it's well, no,
Leanne 32:06
no, I wasn't. I wasn't dropping low. So let's go another new unit.
Scott Benner 32:12
Go another unit. Do another five. Do it again, boys. So you're like three and a half an hour? Ish around there?
Leanne 32:21
Yep. Sometimes even more. I mean, it just kind of depends. You know how loop works?
Scott Benner 32:27
Right, right. Yeah, yeah. Sometimes you'll see a checkup right? Does it ever go away? Like you ever see it take your basil away
Leanne 32:35
for maybe 10 or 15 minutes, but not for very long, just looking
Scott Benner 32:39
for balance? It doesn't care. Right? You never look like you're getting low to the algorithm.
Leanne 32:44
See, like right now? I'm running 90 And my basil is 5.1.
Scott Benner 32:51
Thank you. And your basil is 5.1. Gotcha. So it's seeing you try to go up and it's being aggressive with your basil holding you down? Yep. And do you see any difference between how you manage yourself and how you manage your daughter?
If you're using insulin, you might want an insulin pump. If you might want an insulin pump, you definitely might want the Omni pod. How do you know? Well, you could try it with the free 30 day trial of the Omni pod dash. Find out right now if you're eligible at Omni pod.com, forward slash juicebox. Now that I've been sure to tell you about the 30 day trial, I want to tell you some more things about the Omni pod. Like it's tubeless. You can swim with it, shower with it, jump in a lake with it, jump up and down with it. It's not connected to any tubing or any devices. Understand I'm saying every other insulin pump that you can buy has a tube that comes off it seems like it's inserted into your body in the infusion set. These are the other ones I'm talking about. And then tubing, tubing could be a foot long, two feet long, three feet long lot of tubing, you're hiding in your clothes, etc. And then it's connected to the insulin pump. And then that's where the insulin goes. You pick that up to push buttons on and and stuff like that you clip that on your belt or stick it in your bra. You see what could be happening here on the pod, not like that at all. On the pod is a little pod. It has everything you need inside of it. When you need to talk to it. You have a handheld controller that is not attached to it. It works through the magic, whatever, you know, technology like you can touch something like a remote control and then on the other like your TV moves. Same thing with the Omni pod. Do you pick up the PDM the personal diabetes manager you tell it like I'm having 43 carbs PDM push button, and it's not magic. It's technology but it doesn't make a big sound but I think you're following along with what I'm saying where Getting a little far away from the point now, the only pod is not attached to anything, right? It's just the pod that you wear, nothing else is attached to you. And you don't have to take it off to swim, or do any of the other things that you might have to remove these two pumps for that or stand like adults, you know what I'm talking about, right? Yep, and other things like that, for instance, soccer, head over now to Omni pod.com forward slash use box and see if you're eligible for that free 30 day trial of the Omni pod Dash. And while you're in the mood to be on the internet, and get stuff for free, how about a free 10 day trial of the Dexcom G six continuous glucose monitor, because you may be eligible for that as well, you know, where you would find out about that at my link dexcom.com forward slash juice box by the way, the links to the sponsors and all the sponsors are at juicebox podcast.com. And right there in the podcast player. There's like little shownotes right there in the podcast player that you're listening in. If you can't remember dexcom.com forward slash juice box, which I think you probably could remember, but I digress. The Dexcom G six, it does some good stuff baby. It shows you your blood sugar in the real time on your phone. I am picking up my phone now and swiping up. And I am going to tell you that are this blood sugar is 132. She has a little bit of a rise from a late night snack. It seems steady like it's not going to come down. And in a minute, I'm going to talk to her about maybe making another Bolus, not only can I see Arden's blood sugar, but up to nine other people could at our house, it's just my wife and I. But you might want your aunt to also look or your boyfriend, your girlfriend, your school nurses, somebody like that anyway, you can choose up to 10 people to see your diabetes data if you want them to see it. And if you don't want them to say it, you don't have to show it to anybody. Dexcom also has alarms that you set to tell you when you are rising or falling, or hitting a threshold that you want to know about for us. We get an alarm when my daughter gets to 70 and 120. You could make your settings, whatever you like. Maybe you heard that and think oh, that's a good safety precaution. You'd be right. Or maybe you heard that and thought I probably could do better with my insulin. If I knew when I was rising and falling. I think you'd be right about that as well. There are a ton of ways to use the Dexcom G six in your favor. And you're only going to find out about them when you go to dexcom.com forward slash juice box and start to look into it. Honestly, the Dexcom and the Omni pod are great devices for anyone using insulin. I hope you check them out using my links for full safety risk information and free trial terms and conditions for the Omni pod. You can visit omnipod.com forward slash juicebox. Alright, now let's get back to Leanne. No, it doesn't seem different to you know,
Leanne 37:58
I just jacked her basil up to where she's
Scott Benner 38:01
getting to that age ranges, periods and things like that are probably here. She's
Leanne 38:05
getting ready. And I can tell because her blood sugars are creeping up for no reason. So I was like, oh,
Scott Benner 38:12
no, you're not gonna have any trouble with that. That'll look like a joke to you. You'll be like, ah, let's turn this up a little bit here. We'll be all set. Just you know her Basil is not going to go up to three, right? I mean, probably.
Leanne 38:26
Well, um, let me see. I got her follow right here. So she she's right now 1.5 But just a little bit ago she was at like, 2.8
Scott Benner 38:38
No kidding. So she's she's running the algorithm as well. Yep. Oh, yeah. Guys are kicking ass was excellent.
Leanne 38:50
I was the guinea pig. I started I got the the the Omnipod I had, I hadn't vote for her and for me within six weeks. Because I wasn't taking no for an answer. Right. And her endocrinologist is like, whatever you want, because I think you know what you're doing. And I said, cuz she was in honeymoon and they wouldn't. They don't usually like people to have the pumps in honeymoon. And I said, okay, so she's got a one to 250 carb ratio. Give me the dang pump so that I can give her micro doses and keep her blood sugar's lower. Yeah. And so they did. And so I tried it on me first I started the November 2 pumping. And I started her on the 10th
Scott Benner 39:44
we can you figure this all out in a very short amount of time. Seriously, it's wonderful. It really is helpful to be able to practice on yourself you think?
Leanne 39:54
Oh, yeah, yeah. Oh, yeah.
Scott Benner 39:56
Take away yeah.
Leanne 39:56
I played around with it. I have a couple of pretty good lows before I. Okay, we know what that does
Scott Benner 40:08
what's that to ever see Apollo 13 when he puts this piece of tape over top of a switch and just says no on it have you get vented the capsule of its air or something like that they were getting a little squirrely at the end. And and I don't know if any of that's historically accurate. But Lovell looks at the guy and he's like, what's that for? And he's like, you know, just in case. You know what switches not to throw anymore? I'm, I'm listened to we don't know each other. And you're an adult. I know, you might be older than me. And I have no idea, I guess. But I'm incredibly proud of you. This is was really wonderful. I mean, I'm, I'm loving hearing this.
Leanne 40:49
Yeah. So I you know, I like with my daughter. I don't mind, you know, and I see a lot of people Oh, my goodness, they're under 100. At night, what do I do? I don't I let my my daughter coast at 7580. As long as she's steady. She's good.
Scott Benner 41:07
Yarden had a great overnight last night. It was super steady. And she was the she was kicking us all night long. Actually, just, I mean, she tried to get a little low around 330 Maybe. But the algorithm got in the way of that. And that was coming down from a correction. To be honest, she had a correction at like midnight. And it took about three and a half hours before it was a little too much. And then a DA it was able to catch it. So I mean, I agree with you, I think steady is steady and steady at any number is, you know, is good. If you're not going to drop then I'd like to be as close to normal as possible. Right? You know? Wow, I don't even think there's much to say to you. You just you're like you just took the podcast. Like I'll do all this. Don't worry. I did it. Now we're done. Let's get back to fixing the fence.
Leanne 42:08
Well, let's rock and roll. If you're gonna do something you might as well go balls in right?
Scott Benner 42:11
Why not? Did you try telling you to try telling your sister about this?
Leanne 42:16
I did. And actually she she told me she was in. I think it was stage two or three kidney disease and I said okay, she said, well, good doctor said she doesn't think it's reversible. I said, All right. This is what you're gonna do. You're gonna you're gonna stop screwing around. Oh, watch my mouth. You're gonna you're gonna stop screwing around
Scott Benner 42:39
where you keep going. Before you keep going. I want to point out that scurrying around seemed like a watch your mouth but balls deep. You were okay with.
Leanne 42:48
Wow, I wasn't gonna say I wasn't gonna say screw it.
Scott Benner 42:53
I love your line. Your line is very jagged. I'm enjoying it. I'm sorry. You said to your sister.
Leanne 43:00
So I I told her she needed to get back into her diabetes specialist and insist that they help her find a insulin to carb ratio. And a good Basal because she was on five different insolence.
Scott Benner 43:19
Really? Like, yeah, trying different stuff she was she was using multiple kinds of insulin at the same time.
Leanne 43:27
She was using like, the weekly one. The ones daily one, then her long acting. And then it was just it was crazy.
Scott Benner 43:38
Sounds like your doctor did not know what to do at all. Just kept throwing things at her. Okay?
Leanne 43:43
She's got her blood sugar's down to right around 130. That's great now, but you know, getting her to listen to a podcast or listen to me very well was kind of hard.
Scott Benner 43:58
Did you tell her I was lovely, and that she would enjoy it?
Leanne 44:03
He's just I don't know, you know, when she's when she's ready to take control? I guess she will. But you know, I'm not here to push anything on anybody? And
Scott Benner 44:11
of course not. No, no, I'm not saying you should. I'm also, you know, it's just interesting. I'm not saying you're gonna reverse her kidney disease. But I mean, even does slow things down or worse, you know, stop progression would be a big deal.
Leanne 44:25
Yeah, well, you know, my dad had my stepdad, he had diabetes, and he was on dialysis. And I took care of him till he passed away too. It's it's hard to watch somebody go down that path.
Scott Benner 44:41
Yeah, that sounds like you might stop the stop the circle in your family. I mean, at least in your in your immediate family. I'm really hoping Yeah, we were all not alive just to grow up and help somebody else die and then to be put in that situation for the next person. You know, like it would be nice stiff and not unreasonable for people to live healthy lives and, and finish up, you know, somewhat reasonably. You know what I mean? Like, like, like, like you're meant to be like in a car accident or something like that. I'm just kidding. Like, you know, like, you know, old on you're,
Leanne 45:19
I'm envisioning, you know,
Scott Benner 45:23
I've just, this is my, this is my luck, I get myself together one way, and then a rock would just fall on my head. But, but No, but seriously, like, we you know, people deserve a shot at a longer healthy life, your you know, your, your end, yours shouldn't be, you know, helping someone else to pass gracefully, knowing that you're about to ask another person to do that for you. And, you know, it's just terrible.
Leanne 45:49
Yeah, well, you know, those in my family that have had diabetes, with the exception of my uncle, I guess I just found out my uncle had type one. All I knew as a kid is he had this packet, this cool little case that he kept all his insulin and stuff in. But I just recently found out it was type one, because I was like, Whoa, you know, no kidding. And then he lived to be like, 84, but my, my grandmother, my mother, nun, or, you know, my mother passed away at 66. And my grandmother was 72. But she had just gotten diabetes. Not too long. He was like, in her 60s,
Scott Benner 46:38
right. So yeah, that's too young. I mean, maybe back then, maybe a couple of generations ago, certainly my grandmother died at 73. It's funny, though, like, I don't know about for you. But like, I look at a picture of myself at my age now. And a picture of Mike my father at 50. And he looks 75 to me when he was 50. And my grandmother passed at 72 or 73. And I mean, in my, in my mind's eye, she was much older. Right? So I know, there's a little bit of benefit that goes on, she also worked much harder than I am ever going to work. You know, she grew up on a farm. And, and, you know, she had a different life. My father worked in a in a factory. I didn't have to do that for very long. I got out of there in my early 20s. So but still, like I get the idea. It's just, I don't know, like, it just, it just seems it seems reasonable, that you should have been able to take these experiences that your extended family had learned something from it and improve, right? Like, that doesn't sound crazy to do and you did it. Like, it's wonderful. I would hope. For me, it sounds like that to me, do you? Do you feel like it's going that way?
Leanne 47:49
I do. Because, you know, like I said, I had a pretty good understanding of how insulin worked. But the way they were telling me to use it, just never, it never worked. It never worked for
Scott Benner 48:05
me because you weren't using enough. Right, right. Because
Leanne 48:09
like I said, I have a one to four carb ratio. And sometimes it's one to two.
Scott Benner 48:17
Really, and but you don't know you won't know when or it just kind of pops up and happens to you.
Leanne 48:23
Yeah. So And in that instance, you know, I watch it on the loop and I say, Oh, well, we're gonna crush that before it gets out of hand.
Scott Benner 48:33
Are you? Are you running? Are you running your your your diabetes? Like a video game? Pretty much I am. Yeah. Score. I have talked to a couple of people recently who seem to put it oh, it seemed to put it in that situation to give me a second, please. I think Ardens Oh, wait, I got I got a hold of her. She's in the shower. Maybe her blood sugar just dipped down. And I was I was texting her for last couple of minutes. She wasn't answering me but she just answered me now. So we're good.
Leanne 49:05
That's funny. My daughter and I both when we when we take a hot shower, we go up.
Scott Benner 49:11
Yeah, I hear it from everybody. You know, you've heard me talk to Jenny about it. And Jenny's like showers don't affect people's blood sugar. Like she's just like it's I think it's different for different people. Like you just
Leanne 49:21
Yeah, yeah. Ours goes up and then our foot on the floor is we both dropped.
Scott Benner 49:26
No kidding. You wake up in the morning and get lower.
Leanne 49:29
Yep. I'll wake up you know. In the 70s and by the time I get my feet down on the floor, I'm my alarms are going
Scott Benner 49:41
what happens to bedtime? We lay down in bed do you get higher or lower when you lay down? Nothing. Nothing happens at bedtime. Okay,
Leanne 49:48
I just stay pretty steady all night.
Scott Benner 49:51
Gotcha. That's interesting with a whole
Leanne 49:54
my daughter. My daughter sometimes will go a little higher but you know a lot of hers are Right now or I'm pretty sure home hormones. I'm dreading the day but you know,
Scott Benner 50:06
oh, you know, stop it. So tell me a little bit about her being diagnosed. What did you notice first?
Leanne 50:16
I noticed the frequent urination. And I called up her pediatrician and I said I need to have her tested for diabetes. And she said, I'll bring her in. We'll just she's probably got a UTI. I said, I'm telling you it's not a UTI. There's too much urine. And too often. So we went in, they tested her for a UTI, nothing but they found ketones. And then they did a blood sugar and an A one C. And I knew where I did. So on the way home, I stopped changing my plans for dinner because we were going to have more carbs for dinner and it a low carb dinner because she her blood sugars are like 279 At that point, but her a once he was 12.9. So I was like, and she had ketones. So I was like, Ah, so I fed her low carb that night. And they call me back in the next morning and said get her to the hospital.
Scott Benner 51:16
Hold on one second formula, and this never happens. What's up? Yeah, go ahead. Well, you need to go take care of that. Right now. Hold on one second. Leanne. Can you give them five minutes and I'll be right back? Yep, I'm gonna stop the recording. So feel free to poke your nose. Nobody will now Okay, again. I'm sorry. I'm back. So, this is so embarrassing. I'm just going to tell you. Things don't usually go like this around here. But Arden you know, her blood sugar was getting a little low. So at first I was just texting or anything like, hey, you know, you need a juice. And she taps on the door, and she's wrapped in a towel. her girlfriends and her are going to dinner tonight. And she's trying to get ready. And she's drinking a juice. He looks fine. I'm like, what's wrong? I'm recording. I'm pointing to my ears as if she can't see the giant headphones on me. And she goes, where's mom? I'm like, I don't know. I made your mouth 25 years ago, like she just stopped telling me where she was gone quite some time ago. I like sound like and so I'm like what's so I finally said the she clearly whatever was bothering her. She wasn't gonna walk away. And I, I uncover my ear. And I'm like, what's happening? And she's like, the dog had an accident downstairs. Which by the way, never happens. Like I mean, just like never happens. And I'm like, we'll go take care of it. She goes, and she's looking at me holding a juice box wrapped in a towel. She's like, I can't and I'm like, All right, I'll go do it. So like I'm downstairs like an all I can think of is like Leanne's talking about mucking the stalls. I'm like mucking my dining room. You know what I mean? Like, oh my God. Oh, I love it. Like if it was hard, it was hard. I would have been back three minutes sooner, but I was like, I've got to sculpt my hands with hot water and soap before I go back upstairs. Anyway, I apologize. That does not normally happen.
Leanne 53:22
It's quite alright. Usually walk. We understand those kinds of emergency. I was
Scott Benner 53:26
gonna say like, perfect day for this because cuz you're gonna just be like, that's fine. I don't mind. It's everybody else would be like, what happened? Like? And anyway, and I don't know what dog it was. So there's two dogs. So now I'm not sure which one's not feeling well, but it's one of them. Oh, no.
Leanne 53:43
Oh, I'm sure you'll find out soon. No, oh,
Scott Benner 53:47
sure. To joy, children, dogs. They're all great decisions I've made as an adult. Anyway, so I was trying to cheeses. So let me try to get back on track here. Your your daughter's diagnosis is like kind of like the the point where I'm interested. So she's when she's diagnosed. You're not getting much information for her either, right? Like it's just sort of like your MDI at that point. Does anybody have a CGM? Has anybody ever mentioned a CGM to you or anything?
Leanne 54:20
No. Well, she was she was prescribed the CGM before we left hospital. When I talked to the diabetes specialist, actually, she was asking me questions and I'm answering her everything, you know, that I've known. And she says, Are you looking for a job? I said, Well, I don't think I have the qualifications to be an diabetes education specialists. And but she she did say that they were opening up a new clinic closer to where I was, and and I should really consider it
Scott Benner 54:58
rolling.
Leanne 55:02
But yeah, but yeah, my diabetes is totally unmanaged.
Scott Benner 55:06
You're standing there right now, you know, you know, basically, boy, this is an insight, isn't it? You basically know about 10 words, because you have type two diabetes, and she's like, you'd be a great person to help people around here. Right? Well, that's a, that's a sign.
Leanne 55:22
Well, I was explaining when, when the doctor walked in, I was explaining a onesies to my daughter. Because you know, I know that. And I was I was even drawn it on the board, write it on the board. And I said, if you have an A one C of 12.9, this means your blood sugar's are Everdeen. You know? And if you want to get under a, I said, Well, what I said was, you want to be around a six, then you need to get your blood sugar's here, and he says, actually, we want him at seven. And I looked at him like, Have you lost your cotton picking mind?
Scott Benner 55:55
Well, yeah, it's, it's interesting. So you knew that much. But what was your agency at that time? Like 11 something right?
Leanne 56:02
Um, no, mine was actually like, well, I don't know it at right then. I'm not sure what it was. But I had fluctuated. The lowest I've ever gotten in, in probably 10 years was a seven. Okay. And I knew how I felt at seven. I still felt like crap,
Scott Benner 56:25
right? How did you get to the seven? Was that just good luck? Was that or is that a lot of restrictive eating?
Leanne 56:30
That was a lot of restricted eating a lot. I mean, I did the HCG Diet For goodness sake, what is that? Ah, what are you inject yourself with pregnancy hormones and only 500 calories a day with no carbs?
Scott Benner 56:45
We and who the hell are you? Wait a second.
Leanne 56:50
I was trying. I was desperate. How did you? You know, low carb and restrictive diet? I lost 100 pounds.
Scott Benner 56:59
But how did you get a hold of? Who are you by this? Oh, you don't even want to know. Really? So okay, but let's be serious, because I see you're out there. Like on some sort of a black market, trying to say trying to save your own life somehow. Right? Yeah. Okay.
Leanne 57:19
Well, I guess you know, my husband and I, we've got six kids. And he passed away when my youngest when my daughter that has type one was five months old.
Scott Benner 57:29
I was gonna say he passed away when he realized he was gonna have to pay for six kids. That's what I would have gotten.
Leanne 57:35
Probably. Okay. And then and then I adopted two kids and I have custody of another one. Plus, I have custody of my two grandsons. So
Scott Benner 57:46
we hold on 678. Is that 1011 11? Did I lose count while you're talking?
Leanne 57:56
So I got six. Adopted to see. I have custody of my my cousin's child. oh nine and then the two grandchildren. And then my two grandchildren.
Scott Benner 58:08
No kidding. What state do you live in? Can I ask this question? Washington? Washington State? Yep.
Leanne 58:16
I'm in Washington now. Okay. All right.
Scott Benner 58:19
You in the 11 kids, the 17 dogs, the lizard and all the other stuff?
Leanne 58:23
Right? Well, well, most of my kids are grown. So
Scott Benner 58:27
it was nice to them believe. Yeah. Do you? Do you have like a line on the wall where you're like, listen, when you're this old, you gotta get the hell out.
Leanne 58:37
I just I just said, my 18 year old is attending UAA. And then I have a I have a 15 year old. My 12 year old my 11 year old grand fun. my eight year old she's my daughter and my six year old grandson.
Scott Benner 59:08
Are there any other medical issues with all those kids?
Leanne 59:12
No, but I do have I'm gonna get I have the trail net that I'm gonna do for them because my my cousin's child, my aunt, her grandmother had type one diabetes, but she's not blood related to me. So
Scott Benner 59:27
I'm just gonna check to get those kids through me by any chance.
Leanne 59:32
Um, I did
Scott Benner 59:34
send them back and I get credit for when you send
Leanne 59:38
them back in. I get everything through you. I do the I do the surveys through you.
Scott Benner 59:42
I appreciate it. But I mean, you know, we're joking around. I'm having a lot of fun here but I basically like I was a huge help to you, right?
Leanne 59:50
Yes, yes. So any any way I can repay that? That's what I'm gonna do.
Scott Benner 59:55
Send me a guinea pig. I'm kidding. Do not send me a live animal.
Leanne 1:00:00
Well, you know, I got a funny story about guinea pigs but you probably don't want to hear.
Scott Benner 1:00:05
I don't know yet. I might be up for anything you say you don't know. Don't sell yourself short. You've said a lot here. I've been intrigued by every second of it so far, so don't don't sell yourself short, please. Okay, so you see, you're managing her. They they're saying a seven for her. And you're saying no, I know that needs to be lower. But then you go home, they do give you a Dexcom going out the door.
Leanne 1:00:36
Well, well, we went on vacation the day after I said, you know, they released us on on Sunday, but they wanted us to stay till Tuesday for the day the education and I said oh, no, no, we're going on vacation on Monday morning.
Scott Benner 1:00:52
She just with the education are not what you take with you. Needles. vials. Yep,
Leanne 1:00:58
I took I took pins and extra needles and a vial and here we go. Blood your blood testing kit.
Scott Benner 1:01:08
And you just went where do you go on vacation?
Leanne 1:01:11
We went to Silverwood amusement park
Scott Benner 1:01:14
to an amusement park. Sounds fun. In Idaho. There's an amusement park. See? There you go. Now you surprise me now you got my east coast. snobby? Miss out of me. I was like there's an amusement park in Idaho. Why would there be an amusement meanwhile? Why would there not be but Idaho so that's a bit of a trip. Did you drive that? Yep. Nice. All those kids. You put them into a horse trailer with all the kids. Where do they go in the car? Car Are they like rolled up in a carpet on the roof? Or how do you how do you handle that?
Leanne 1:01:48
I threatened a couple of them to be ornaments on the hood. But we we broke out on the side of the highway and I had to repair my alternator right there. We got it. We got to write in the on the back of a big old tow truck. It was a fun adventure.
Scott Benner 1:02:07
I bet you it was I'm not looking at pictures of silver woods. Or silver one. Look at that. It's an art. It's cool. There's trees around it and mountains. Yep, yeah, I we
Leanne 1:02:18
we ran into we went through the b&b and we rented a campsite with a tent and everything.
Scott Benner 1:02:26
That sounds like fun. And how did your daughter do? Being diagnosed? Was it stressful on her? Or did she kind of roll with it?
Leanne 1:02:36
As she just rolled with it? She said? She said Well, no, I'm kinda like you so well. Kinda. Yeah. She says, Well, you got me. I got this.
Scott Benner 1:02:47
Just like she trusted you. Oh, yeah. I bet you that felt like a lot of pressure. Because you were like, kid, I can't even take care of my own diabetes.
Leanne 1:02:57
Like, I was I was hell bent on on taking care of hers correctly, though. You know, I mean, I understand. Oh, and that's when I realized. I mean, I realized right away. I had been struggling with mine for so many years that I was about to give up. Just flat give up. Um, on management, and then I don't know, when they said she has type one. I went ding Yeah.
Scott Benner 1:03:27
I like given up quite Yeah. Well, listen, you should never give up. You're raising 11 Children, 53 animals. You're, you're a widow, and you can fix an alternator on the side of the road. I think I don't think you should ever give up to be perfectly honest. You might be the last person left when this whole thing goes to hell. They just, I mean, really, you You sound very capable. And I mean, if this doesn't prove it to you, I wouldn't know what would I would think just raising those kids would make you think you could do anything but
Leanne 1:03:59
well, well. I mean, not not like give up in life. I mean, but I was just Yeah, no, I understand. I think that there was no no treatment for me. That was gonna work because I've tried everything. Yeah. I'm not a big pill popper,
Scott Benner 1:04:16
though. The idea that just there's no answer. Like, this might just be my reality. Right? Yeah, I've got that kind of diabetes.
Leanne 1:04:24
Yeah. And I was, you know, thinking back you know, you reflect back on your mom and your your stepdad and you see the crap that they went through. And it's like, oh, I don't want to do that.
Scott Benner 1:04:35
No, I mean, your mom lost her sight. Your sister's kidneys are going like there's there's plenty for you to be scared of, you know? Yeah. Is there any chance one of those 11 kids will name a kid Scott? Can I just throw that out there now like tried to get a like you said you do anything. I don't really need you to do much. But I would take a name child or horse. Horse. I don't know we might be able to convince one. Yeah, no, no. That's probably not gonna happen. They're gonna have their own problems in life and then probably name it Benner. You think I'll take that? That'd be a cool name. Oh, cool. We'll roll with that, then I'll take. I think it's, interestingly enough, because I'm adopted. And my one brother has two stepchildren, but none of his own. And my other brother has a daughter. The I think the bloodline stops with me. My dad had a brother who didn't have kids, and he had a sister, so I'm right. Right. Like, I'm like that. Yeah, it's gone. If my if one of my brothers doesn't have a boy, that's that.
Leanne 1:05:39
Yeah, that's
Scott Benner 1:05:42
okay. I mean, I don't care how much it matters one way or the other. Yeah, to be honest with you. I'm not out here trying to keep this. I mean, it ain't so great. You know what I mean? I don't think the world is gonna be no offense to my brothers. They're wonderful people, but, but I'm just saying, you know, I don't think it's super important to get the name going. But that's interesting. You know, my dad. My dad's name. I've never said my dad's name on here before. But my dad was my dad basically had a girl's name. And because of that, he had a nickname. And his nickname was so it was just the first three letters of his last name, like people called him, Ben. But his name was not Ben. And if you and I sat here, it's two o'clock in the afternoon, if you and I sat here for the next seven hours, and I let you guess what my father's first name was, you'd never guess it. It literally was just, it's one of those things. Like I'd look at my grandmother and think like, what were they thinking? Is it Carol? No, that would have made sense even. Do you want three more guesses? I'll give you three more guesses. And I'll tell you and I'm gonna give you the first letter. It's L the mind boggles
Leanne 1:07:00
no idea. Yeah.
Scott Benner 1:07:03
Like how could this be? It's a woman's name. It begins with ln. Now see, that's even really a woman's name. That's a pretty androgynous name. Right? You Lin Lin could be a man. My dad, my dad's given name was Luverne. Luverne. How does that even happen?
Leanne 1:07:19
I have no idea. That's like, Sue. Yeah,
Scott Benner 1:07:22
there's a boy named. Exactly right. I didn't know we were gonna do a no, we were gonna do all country songs while we were sitting around together today. Yeah, no, my father's name was Laverne. People call them Ben. So, and my mom not a big fan of his. So I couldn't name a kid Ben. That's for sure. Nobody was naming a kid Luverne based, they sounded weird
Leanne 1:07:44
that he wouldn't go by verb.
Scott Benner 1:07:47
You know? I never even kind of weird. You're making sense? I don't know. Alright, man. Is there anything that we haven't talked about that we should have? Oh, I don't know. I mean, what made you do this? Just because I asked for type twos, right?
Leanne 1:08:06
Well, yeah, I mean, it was kind of impulsive. You know that ADHD? Sure, why not? And then it was like, oh,
Scott Benner 1:08:17
did you? Did you breathe? Think it as Time was passing?
Leanne 1:08:21
Yep. I was like, oh, but then talking to you know, John,
Scott Benner 1:08:27
on the board. Uh huh. Who also has type two? He's coming on the show. Right? Right. Yeah. Right.
Leanne 1:08:33
So then I was like, Okay,
Scott Benner 1:08:36
you can do it. Yeah, there's a small,
Leanne 1:08:39
good to see. And people may even help, you know, I mean, it's it's a tough one, because everybody wants to trust their doctors, and I don't trust doctors as far as I can throw him anymore.
Scott Benner 1:08:53
Well, I mean, listen, if you get a good one, then you're you're lucky, you know? And then you can but if you start getting money if you taken six different pills and injected a bunch of stuff and your blood sugar's you know, you're a one season the elevens. And your blood sugar's are four and 500. I mean, somebody, somebody's not giving you the right answer, that's for sure. And no, yeah,
Leanne 1:09:12
well, I guess, I guess, what I what I really mean by that is, when it comes to diabetes, it doesn't matter what type you are, if you don't take control of it. There's nothing the doctors can really do for you. You know, I
Scott Benner 1:09:28
mean, they don't know you. Everybody is different. Yeah. That's that honestly, and they just go by protocol. That is the most insightful thing anyone said on here in a while, you're 100%. Right? Really, you have to do this for yourself, and you have to take I mean, common sense, I think is of the utmost importance. You can't just fall into like patterns where you say, Well, this is what they told me it's not working so then it must just not work. Like it That can't be your answer. It's your health, like, at the end of bed at the end of poor health is death. You know, like you can't it's not like you're ignoring replacing a screen door on your house or a creaky board on a floor or something like that, you're not gonna just start walking around at one day, like, you're gonna, you're gonna die. Like you were on your way to dying. You know? And you figured that out. Like, it's, it's really interesting that you had the same exact kind of epiphany thing that I've heard so many people talk about on here, so many adult type ones, who would have described their care as shaky, maybe have a child or get married, or have a child get diagnosed, and then they realize, Oh, God, I have to stay here. And I'm not on the quick path to staying here. I'm on the quick path to leaving, and I have to fix it. And it's the same thing happened to you. It's, it's got nothing to do with diabetes or type one, it's a human thing. Like you. You were faced with an ultimatum that didn't have an escape plan. And you were just like, Alright, why I mean, I'm not I'm not gonna, I'm not leaving. So I gotta do something. And I'll be damned. Like, we ended with no training whatsoever and only a podcast under your arm, you're giving yourself three and a half units of insulin an hour as a type two in a basil. Like that's a lot of you're laughing. But that's a lot of it's a lot of common sense. It's a lot of caring about yourself. It's a lot of saying, I'm not going down without a fight. And that's, that's all really important. You know, you need those things.
Leanne 1:11:38
I don't do anything without.
Scott Benner 1:11:41
I mean, listen, I wouldn't went on that damn vacation after the kid got started. I'd tell you that much. I'd been like, look, kids, we're not going to Silverwood right now. I need a minute. But you were like, Let's go. Load up load.
Leanne 1:11:56
I actually I was in the hospital. I told my my 15 year old I told him and I said, Hey, little change of plans. I'm gonna need you to pack all our bags for me Sure. We all have swimming suits and, and clothes to wear.
Scott Benner 1:12:13
And when we get home, we're still doing this. You know,
Leanne 1:12:17
we had to buy hoodies we had.
Scott Benner 1:12:21
But you hear people talking about being afraid to go to college? Or, you know, how's my son gonna do this? How's my daughter gonna do that? You were just like, we'll do it. It'll be alright. And you just did you know? Yep. Yeah,
Leanne 1:12:33
well, I'm not gonna. I decided since she was diagnosed, and she was crying. And she was like, I'll never be able to have this. And I said, Listen, baby, you're gonna be so sick of candy. You're not gonna want anymore?
Scott Benner 1:12:46
Yeah. No, no kidding. I've heard art and be like, I don't want that. Please don't give me that.
Leanne 1:12:50
Yeah, yeah. So we we actually don't use candy or anything like that to bring her blood sugar's up anymore. Because she's so sick of it. Yeah, I believe it. I really do. And so, you know, all we do is eat. Text or eat
Scott Benner 1:13:09
snack? Yeah, yeah, no kidding. And she's doing okay, how much of it she managed on her own.
Leanne 1:13:16
Most of it. Good for her. I watch her follow up. And I tell her, you know, if I see her trending down and she's in school, not really paying attention. I'll just shoot her a little text if she means just a little bomb. I'll say snap. Yeah. But if she needs a full fledge, stop that low.
Scott Benner 1:13:41
Eat. And that's it. And that's how you guys are doing it. That's really wonderful. That's
Leanne 1:13:45
it? Yeah, she matter of fact, she. She went to spend Christmas vacation. She spent a whole week at her friend's house.
Scott Benner 1:13:55
By yourself. Yep. Oh, good. You didn't worry about it. But you watched her a little bit from a distance with a Dexcom follow.
Leanne 1:14:02
I have alarms
Scott Benner 1:14:05
where they said that by the way for her.
Leanne 1:14:08
Um Let me check my other phone here.
Scott Benner 1:14:12
Where do you set yours?
Leanne 1:14:16
Mine Oh, okay. Hold on. So her settings I have her at at 75 for her low to alert me. And then on the other app I on on one app. And then on the other app, I have her at 70. Okay. So I know the difference between the two. Yeah. And then her high is one ad right now but we're bumping that down next week to 150
Scott Benner 1:14:53
for you. That's excellent. And what do you do for yourself?
Leanne 1:14:56
So my mind is set. I My correction range is 70 to 80. My suspend is 70. My Basal rates are 84 Yeah,
Scott Benner 1:15:11
you don't get very high. You're saying anymore?
Leanne 1:15:14
I don't get usually over 120.
Scott Benner 1:15:18
That's excellent. Good for you. Well, yeah, now they are gonna make you work in that clinic.
Leanne 1:15:25
Well, I don't I'm not as aggressive with hers because she is she has hormones going on and what she's Yeah, so one ad with hormones is pretty good, I think. No, I
Scott Benner 1:15:35
do too. I also think she hasn't been doing it that long. Like you're talking like a professional here. But I mean, how long have you been at this? Really? Not that long. Right? Is she honeymoon? Do you think at all or? No? She's done with that now, but you did see it in the beginning.
Leanne 1:15:52
She was horribly bad. That's why I pushed for the pump so bad. Um, and then I got her on the pump. It's just been the last last month that she quit with any money. Okay, is it getting? Yeah. And then her needs went? doubled.
Scott Benner 1:16:10
No kidding. That quick. Yeah, that's what we add to it. It's hard to like, people come to me all the time. Like, it can't be like, it was just this. And now it seems so much more like a it can be like it just, it can happen. It can happen quietly and slowly, or it can happen quick and loud. You know, there's no say in how it's going to end if you have a honeymoon that you're that you're living with.
Leanne 1:16:31
Right. So like, for instance, you know, like I said, She's, she's got hormones going on right now. And she's in range 97.5% of the time.
Scott Benner 1:16:42
That's great. You're doing terrific. Are you thinking about the Omnipod? Five, are you gonna stick with a loop?
Leanne 1:16:48
I'm gonna stick with loop. I like the flexibility of it. The better control the tighter control. Now, you know, I'm glad that they have the Omnipod fives for you know if she goes off to college or whatever. That will be an option for her. Or if something happens to me. That's an option for her.
Scott Benner 1:17:08
Yeah. Well, yeah. Because you had to did you did you set that whole thing up yourself? Like, download the? Yeah, okay. Yeah, I gotta be honest, I couldn't do it.
Leanne 1:17:19
It was it was a challenge. I set that up. I set up Nightscout. I set up the loop follow. And then of course at school yesterday, she somehow reset her phone. And so she was stuck with her basil. And I just update yesterday. And so she was stuck with her basil. And I was like, the school called me and I was I just been there. Drove 50 miles up to get my grandson because he was not feeling well. Got back home and had to drive back up there to get her. But I do see 50 Pull that pawn off of her right now.
Scott Benner 1:18:04
It's gonna take you too long to get there. She took it off till you could get there. Right so she wouldn't be getting the extra insulin she didn't need. Right. Interesting. But you're like, oh, yeah, like MacGyver over there.
Leanne 1:18:16
She got up to 154 before I got there, it took me about 25 minutes.
Scott Benner 1:18:21
Okay. So put a new pump on put new settings with it.
Leanne 1:18:26
Well, I had no I had to bring her whole phone home and
Scott Benner 1:18:31
reprogram
Leanne 1:18:32
it. Reprogram.
Scott Benner 1:18:37
With this kids go to school. 50 miles from your house.
Leanne 1:18:40
No, they're 25 miles out. But I was in town yesterday when they call Oh, and you
Scott Benner 1:18:45
were farther away when it happened. I got it. Yeah. All right. I don't pretend to understand where you live. It sounds like you live in the middle of a forest.
Leanne 1:18:52
I live in a in a place called hum tulips, Washington.
Scott Benner 1:18:55
Wait a second. Don't go anywhere. I was about to say goodbye. But now it's not happening. That's a real place. You didn't make that up. I'll be Damn, that's a real place. So is there another meaning to hump tulips? Or do you live in Tulum? Washington, what's going on?
Leanne 1:19:17
Well, there's a couple of different meanings for hump to UPS, but
Scott Benner 1:19:24
alright, I'll figure that I'll figure that out later. Oh, my god. I can't thank you enough for doing this with me. I really appreciate you taking the time. Well, it was fun, though. I had a great time. Are you kidding me fun. This is the best podcast I've ever done in my life. I expect to be nominated for an award for this. I don't know where but I want it to happen. I had a wonderful you really are. You were just unexpectedly delightful and insightful. I didn't know what to expect. I would like to have more conversations with type twos and a If they're listening, I want them to know that what I expect is that most of the conversation is going to be you saying, I don't know. You know, but I think I think there's some value in hearing that other people don't know. Because, you know, then someone listening, whether they have type one or type two, maybe they'll feel a little less, like a failure for not understanding, you know, and maybe that's the first step to kind of finding your, your balls and, and going for it, you know?
Leanne 1:20:28
Right. You know, it's, it's hard. It's, it's really hard when when you do feel like a failure, because you're doing everything they tell you to do. And you're not getting anywhere. You're pedaling backwards because there's damage being done to your body. My doctor told me to just make sure my my morning blood sugar's were 150 That was your goal. That was the goal. Yep.
Scott Benner 1:20:55
Try not to die right away, but you won't live too long. But yeah, we're gonna do that whole,
Leanne 1:21:01
and I just kept thinking, who's gonna take care of all these?
Scott Benner 1:21:06
No kidding. I mean, honestly, that's a lot of kids out. How, by the way, how old are you? 50
Leanne 1:21:12
I'll be 52. Tomorrow,
Scott Benner 1:21:14
tomorrow. And how young is the youngest kid? Oh, eight. Okay. All right. Yeah. All right. Well, you need to make it near 60s At least just to get that one out of there. Right. Yeah. And for how about for you, by the way, like, you know, I'm sure there's things you'd like to do. Chief among them not be aching, just all day long and in pain from just cleaning the house and stuff like that? You deserve to live? Well?
Leanne 1:21:41
Well, I you know, I my goal. When I started having children. My goal was to be done and have all the kids out of the house by the time I was 40. Yeah, yeah.
Scott Benner 1:21:54
Got that pretty wrong.
Leanne 1:21:57
Well, now I'm going for 6565
Scott Benner 1:22:02
I'm hoping to own something that I enjoy once before I die. Like that's how I think about it. Like I have all the money goes out the door. For all the things for the kids. Every once in a while. I'm like, I wonder what I would have done with that money if they weren't here. Like what I've just saved it maybe that would have been nice or bought something nice or gone on a vacation. Like I haven't been on it. You said you went on a vacation I got jealous was like oh, that sounds
Leanne 1:22:27
we go somewhere every just about every year. You know what be it be at home to Alaska, or you know, I took him I took him on a six week vacation to Las Vegas.
Scott Benner 1:22:42
You went to Vegas? What do you do in Vegas for six weeks with kids?
Leanne 1:22:47
Well, we we rented a house and had a pool and just hung out. just hung out.
Scott Benner 1:22:54
Damn, that sounds like the right idea. Alright, I'm doing that. So just take an Airbnb or something you just jumped in and why not kidding. I'm thinking I'm kind of crazy like that, though. You know? Oh, listen, whatever kind of crazy. You are is working fine. So you're you're okay, you know. That's amazing. All right, I'm gonna let you go. Thank you so much. Can you hold on for one second? Oh, thanks.
First, I want to thank Leanne for sharing her type two story. I'd also like to thank Dexcom, makers of the Dexcom G six continuous glucose monitor and Omni pod makers of the Omni pod dash. I'm also going to remind you to go to dexcom.com Ford slash juice box to learn more about the Dexcom G six. And check out that free 10 day trial possibility. While you're on the internet, you can also go to omnipod.com forward slash juice box, see about the possibility of their 30 day free trial the Omni pod dash, we're just get started right now just jump in baby. If you're using insulin, these devices are for you. The next time you see a type two story pop up on your feed, it will be with John. But we need more people to share their stories. So I need you to reach out. If you have a type two story that you want to tell. Find me. Okay, go to juicebox podcast.com. And there's a link there where you can send me an email. I hope to hear from you. Don't forget if you have type one diabetes and you're a US resident or you're the caregiver of a type one and a US resident, you can go to T one D exchange.org Ford slash juice box right now and take a survey that will take you fewer than 10 minutes that will help people living with type one diabetes and support the podcast and make you feel good because you're doing good stuff. And does other stuff do you'll read about it when you get to the link T one D exchange.org forward slash juicebox. Please subscribe and follow in the podcast app that you're Listening in right now that's all I've got for you I'll be back very soon with another episode of The Juicebox Podcast
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#664 Defining Diabetes: Dictate the Pace
Scott and Jenny Smith define diabetes terms
Scott and Jenny Smith define diabetes terms In this Defining Diabetes episode, Scott and Jenny explain Dictate the Pace.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 664 of the Juicebox Podcast.
On today's episode of defining diabetes, Jenny Smith and I are going to define a phrase that I use every day managing type one diabetes, many of you may think of it as a sports thing. But for me, it applies to type one and insulin management in general very, very well. So today, Jenny and I will define dictate the pace.
You know, if you'd like to hire Jenny, she works at integrated diabetes.com, head on over there and check her out. Before you do that, please remember while you're listening that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan, or becoming bold with insulin. If you have type one diabetes, and are a US resident, or are the caregiver of a type one, and R US resident, please head over to t one D exchange.org. Forward slash juicebox. Take the survey, you'll be helping people with type one diabetes, and supporting the show.
This episode of The Juicebox Podcast is sponsored by us med. US med is the online diabetes supplier that you've been looking for. They have a dedicated 800 number for Juicebox Podcast listeners. And you can call today to get your free benefits check 888-721-1514 Or go to us med.com forward slash juicebox. US med wants to bring you better service and better care than you're accustomed to. All right, Jenny, I would like to talk about an idea that I keep in my head around diabetes that I don't think you're gonna see on any in any diabetes textbooks. But I like to dictate the pace. And I think of that as a sports metaphor. In my mind is usually a boxing metaphor more than anything else.
Jennifer Smith, CDE 2:24
I was thinking running, but Okay, okay.
Scott Benner 2:27
Well, yeah, that's a good idea that, you know, you could jump out ahead. And once you have the lead, you're in control of maintaining the lead. Right. Okay. It is a simple idea. Normally what I say it's funny, I'll retell this very quickly. I was in front of like, 500 people one time. And I said, you try to imagine that you invite somebody out to speak at something and they get up on the stage in front of all your people. And he goes, has anybody ever been in a fistfight? You know, the people who are running the event go, what is the guy on stage talking about? And he's here to talk about this. Better this guy? So you hear somebody in the corner, go, he's got a podcast, people seem to like it. I don't, it's not my fault. But I say they said this one time, like, who's ever been in a fistfight? And this little kid I swear to you is like six years old, just jumps up out of his seat and puts up his hand and I'm like, I'm like, You should not be hitting people. It's like, Is anyone else any grown people been in the fight? So this man finally like, kind of put his hand up, but he was embarrassed. He's an older guy, time he goes, I've been in a couple fist fights. And I said, Would you rather hit the person first, or get hit first? And he did not hesitate? He's like, I want to hit first. And I said, Yes. And I was like, that's how I use insulin. I'm like, you've got to hit first. Because then everything that happens after that is dictated by the pace that you've set. Yes. And more importantly, what I hear people talking about all the time with insulin is they act like it's happening to them, you know, they just diabetes is happening to them all the time. I don't know, I get high, I get low. I don't know why, like, right. In that scenario, diabetes has dictated the pace. Yes. And now you're the person frantically trying to catch back up again. In my opinion, you hit first. And that way, at the very least, even if what happens next isn't exactly what you want it to happen. At least you know, you made it happen. And you can kind of step back and make sense of that I Bolus five units for this meal. And, you know, a half an hour afterwards. I'm 65. And it's not coming up. Right, right. I didn't get a spike. So I think my Pre-Bolus was okay, but I'm a little low. And what that tells me next time is well, maybe I'm gonna try four and a half units for that meal next time. But at least you know what's going to happen next. Because you know, if you if you let diabetes go First, if you don't Pre-Bolus your meal, as an example, even if you've got the right amount of insulin, now you're shooting up. And you've added variables, mathematical variables that your brain cannot find or figure out anymore, right? You could kind of get ahead of the idea of I think this meal is 45 carbs. And I think my insulin to carb ratio is this. So it's five units. But once you don't Pre-Bolus, once you give those carbs the opportunity to get out in front. Now, it's dictating the pace, and it's changing the rules as it's going, because no longer you just trying to cover these carbs, you could have started at a beautiful blood sugar. But if you didn't, Pre-Bolus Now, you're not just trying to cover these carbs with this insulin, but you're trying to stop this rise, you're trying to take this momentum out of this rise, and you've got to correct a number and keep the food covered. All without creating a low later. Right. But if you just go first, if you punch first, what happens next? You made happen? Right?
Jennifer Smith, CDE 6:00
And then you can figure it out from there, like you said, yeah, if it's, you know, if it's your first sort of adjustment to a ratio, or you've really decided to get more precise about your carb counting, and you're trying to figure out your insulin dosing now that you are being more precise, or whatever it is, you're putting in effort, and whatever outcome is because you made a decision to do something this way. And it like you said, it makes it a lot easier than to say, okay, you know, I got low after this meal where I know, everything I put in should have been right, maybe now that I'm counting more appropriately, maybe my Bolus ratio is actually too aggressive. Maybe it doesn't need to be as much insulin, or maybe I Pre-Bolus. Really, really long. And that's the reason now I'm actually too low. Yeah. So you know, it gives you points to sort of reference and go back to, to make a better call the next time. If you give enough time, it's kind of like your example, I know, you always use the tug of war game, right? Between insulin and food and insulin and carbs. So you want insulin pulling a little bit bigger. And, and, and sooner, and then you have more control of the out of why things are turning out the way that they did, right?
Scott Benner 7:24
Yeah, I mean, people are gonna put it into whatever perspective they can, that's what I want. I mean, you might not be interested in the same things I'm interested in. But you know, another way to think about it is if you like baseball, and you're pitching, you need to strike the first time, right like is nothing worse than starting with a ball. Now, let's want to know, and you're already behind. And now you're just like, Oh, now everything gets finer, it gets tighter, you have to be perfect, because you're running out of chances. And but if you start with a strike, you're ahead. Now if the guy should hit the ball, and he gets a hit, that's good, good on him. Tough luck for you. But at least you're not fighting with this guy down to balls, no strikes, like like you're dictating the pace you're like are if you beat me, you beat me. But if you don't beat me, we're playing this game on my terms, I'm getting ahead of you, you're the one who's at, at a disadvantage, not me. And once you get that advantage, the worst thing you can do is give up the high ground. Like you always make the opponent fight from down low, right. And that's what you have to do with the diabetes, it's what you have to do with the blood, I think of it as the blood sugar, probably, but you come at it hard. And then you're now dictating the pace, and then it might try to do something else. And maybe it'll even do something that you don't like, but you don't switch places with it. When that happens. This is such a weird idea. But, you know, you strike first, you're ahead, it strikes back, you don't go into defensive mode, you push back again, right, you keep the high ground, always keep yourself in that position. This may be more of a an intellectual exercise than it is an actual physical exercise, when you're not managing insulin, but whether you think of it as a mindset or as an actual action that you're going to take in my mind, the minute you start, you know, I'm I'm joking my sports metaphors all over the place, but the minute you start covering up your face, I mean, think of every fight you've ever seen when I cover up, um, skirt, you know, like you gotta keep moving forward.
Jennifer Smith, CDE 9:39
Right? I kind of think about it in a little bit. I guess in I think about it in terms of how insulin works, right? As we talk time and again about rapid insulin and really dictating the pace means you understand how long it actually takes insulin to start I'm working. And so I kind of think of it being a runner, I think of it like, a warm up, like a Pre-Bolus, to me is kind of like a warm up. I don't leave my house at, you know, huge, like, I don't sprint out of my driveway, right? And my muscles are gonna be like, Okay, we're done now, thank you so much. I need to get things going. And that's why I think about my Pre-Bolus is kind of like that warmup time, until like, insulin is really now like, it's ready. And this is this is the time to put my foot in. Because it's gotten enough time to get its momentum, right and get moving. So that's kind of how I think that's beautiful.
Scott Benner 10:46
Really, because that's like, that's like thinking about it like starting a Have you ever seen a locomotive start moving? Or have you ever been on a cruise ship? Like a job? Okay, if you hire Alright, well, listen, I'm sad to tell you I've been on a cruise ship. And it's, you're up against the dock, and the things not moving, right. And they unmoored it, and then it starts to move. And it's many minutes before you recognize that the ship is moving. Right. So like, it's the old adage, it's like turning the turning a turning a ship takes forever, that kind of thing. But when you just talked about it as warming up to run, I've seen a a freight train, pull pull out of a station, and it starts to move, like it's trying to go and it doesn't move right away. And then it starts very, very, very, very slowly. I mean, almost imperceivable to your eye at first, and then it's moving at a snail's pace. And then it almost looks like it's walking away. But I'll tell you what, 15 minutes from now, that thing's got it moving like a rocket, you know, and you can't stop it. That's a perfect way to think about the insulin. It really is. You can't just you can't just push the button on your pump, and start eating. By the way, especially with some pumps, I'll use Omni pod as an example on the pod puts insulin in on the slower side. Like if you're making a big Bolus, it isn't magically, it isn't magically in 30 seconds from now you might look up a couple of minutes from now you've only got five of the 10 units in
Jennifer Smith, CDE 12:28
and as a good example, how many pods each click is point 05.
Scott Benner 12:33
Really, as its Bolus, click
Jennifer Smith, CDE 12:35
05.
Scott Benner 12:36
If you isolate
Jennifer Smith, CDE 12:39
zero 5.0 5.0. I mean, it takes a while I've I've counted them. I did it. When I first started years and years ago on Omnipod. I asked my trainer, I was like all these little cliques. She said, Yeah, if you wanted to, you could count them up and see how many go into like a one unit Bolus because they're all point zero five,
Scott Benner 13:00
you were the exact right kind of dork for this podcast.
Jennifer Smith, CDE 13:05
I like it. That's okay. I'll be a door. No, I
Scott Benner 13:07
mean that. I mean that in a wonderful way. Yeah. So in my mind, when if you hear me say, like, dictate the pace, this is what I'm talking about. I'm talking about, you can you can picture it any way in your heart, you want to if you're a UFC fan, once they're down on the mat, jump on top of them and keep punching them in the face until they give up like do not stand up, turn your back and get kicked in the back of the head. You know. And I do think that in practical terms, when you're making a Bolus, it's, it's easy to push the button and just think it's going to be okay. But if you're using the CGM, my goodness, 30 minutes afterwards, take a look at it. You know what I mean? 45 minutes, take a look, you know, if you have your setting set to alarm on your Dexcom, for example, like Ardens is 70 and 139 7121. I'm following her. If 30 minutes later, she's 115 Diagonal up. And I'm starting to look at a real harsh up. This might not be going the way I think it's going to go. But if you don't look or if you have your high alarm set at 180 You know, then by the time you want to know soon enough, it's too late now. And now you're and you're immediately chasing at that point when you find out too late. Now you're chasing now you're from a previous episode now you're showing up 15 minutes after the bank has been robbed. Right? So we want to the information is your friend. You know people talk about like data in court, whatever you want. But this thing is telling you what's about to happen or what is happening. And if there's a moment where if you react correctly, you maintain control. And there's a time that you wait too long for that. control changes hands. And now you've given up the high ground. And what that means practically speaking with diabetes, is you're about to spend the next three to four hours, beating your head against the wall, drinking juice, or bolusing, or whatever's going on. Because you let this thing get the better of you. And in my mind, a couple of well placed glances. A little bit of effort upfront, saves three and four hours of what actually feels like a tragedy when it's happened in the middle of your day. Like it really, you hear people and especially overnight.
Oh, it's terrible.
Jennifer Smith, CDE 15:34
I think the overnight is the biggest complaint.
Scott Benner 15:36
Yeah, yeah. Because when you going to sleep now, it because in your mind, you're like, Okay, well, I Bolus this one ad. It's not going to be low in an hour. But if I fall asleep, am I going to wake back up, and then you start doing that thing where you're like, I'll just sit up till 230. And then at 230, it's 150. And you're like, Oh, I guess it needs a little more. And all of a sudden, it's four in the morning. And, you know, it just it paying attention upfront, doing the little things, keeping the timing of the insulin on your side, dictating the pace, however you want to think about it. A little bit of effort upfront saves a ton of problems on the back end. Right? That's all and some of it
Jennifer Smith, CDE 16:15
is also you know, some experience obviously goes into it too. I mean, I would certainly say that it takes a little bit of time to know how to manipulate things, right. I mean, I had a horrible pods like the other night like horrible. Obviously slept through high alarms. I mean, in my heart Hi, alarms are not like terribly high. I slept through a lot of alarms woke up in the morning. I think it was like 250 to 50 am. And I knew before even looking at my CGM I knew that I was high. I knew I was high. And I look at it and like, Okay, this is always lovely at this time of the night right and I Bolus took an injection to Bolus because my news sites I knew at a blood sugar like that we're just not going to get over this Hi, I Bolus are navigated up my low alarm just a little bit in case of need to kind of catch what was falling. And it woke up in the morning at 84. Nice and flat. I felt like I jumped up. Like nobody was there to see me. But that's okay. I did my own little happy dance.
Scott Benner 17:31
Well, I'll do it with you. Because knowing that that's what needs to be and at 230 in the morning, getting your ass out of bed and changing that pop up. Give me your shot. That's not easy to do. But what it did was it saved your next day. It did really poorly. You If you ignore that you wake up you're 300 Yeah, spend five hours fixing that easily. And you feel oh, it was 301
Jennifer Smith, CDE 17:53
I was 301 that I can't remember the last time I saw a number that hi i so it was I mean, very clear to me where my pump had actually like pooped out. Yeah. And in terms of knowing you're talking about before, kind of like that black hole. Kind of there was clearly a black hole that started because I could tell where the black hole ended up causing the rise up to happen. And it just kept going from there wasn't
Scott Benner 18:25
gonna stop No kidding. Yeah, I mean, and you said something earlier to like, you really do need to. Like if this is for somehow this is your first episode of the podcast. Oh my God, please don't start here. You know, like, go back to 210. Listen through the pro tips. Try the defining diabetes series. Like you don't want to jump in at ninja level and try to start rolling. You really will mess it up. There's a lot to understand on top of that, but once you're caught up, listen, I think of the podcast is a compendium like my assumption is if you're listening to this episode, I mean, I don't even know this is probably in the late six hundreds. You know, my thought is that you've heard the stuff before this. So yeah, okay. Well, I really appreciate you taking the time to do this with me. Thank you so much. Always fun, thank you I cannot be the only one of us who is incredibly frustrated with the company that sends the diabetes supplies to our house. I just can't be I mean, if the experience that I've had so far and all these years is even a little reminiscent of what you're going through, then you may be looking for something better. You may be looking for us Med, a company who prides themselves on white glove service. They want you to get better service and better care than you're accustomed to. US med is the number one distributor for freestyle Lee Bright systems nationwide. They are the number one specialty distributor for Omni pod dash, the fastest growing tandem distributor nationwide and the number one rated distributor index com customer service surveys. With over 1 million diabetes customers served since 1996. US bed carries everything from insulin pumps, and diabetes testing supplies, the latest CGM, they always provide 90 days worth of supplies and fast free shipping. US med accepts Medicare nationwide and over 800 private insurers. Come on, give them a call 888-721-1514 Get your free benefits check. Find out why they have an A plus rating with the Better Business Bureau Wouldn't you like some white glove service? I know I would. The phone number again is 888-721-1514 and that number is just for Juicebox Podcast listeners or you can go directly to us med.com forward slash juice box and get that free benefits check there. At that link. You can also see reviews for us met better service better care. There are links in the show notes of your podcast player and links at juicebox podcast.com to us Med and all the sponsors
if he enjoyed this episode of the podcast, there are many more defining diabetes episodes. There's a list of them a complete and full list of them at Juicebox Podcast type one diabetes on Facebook, that's the private group that you might want to join. I am now going to try to list all of the defining diabetes episodes in one take without misspeaking. I'm not going to do the episode numbers you're gonna have to get those from the Facebook group Okay. All right give me a second here on me. Let me center myself
you're ready you're I go. Start started episode 236 With Bolus then Basal honeymoon a one C time and range standard deviation extended Bolus algorithm non compliant glycemic index and load Pre-Bolus Trust will happen low before high Bertel diabetes stop the arrows ketones insulin resistance and over Bolus feeding insulin bumping nudge rage Bolus compression lows and interstitial fluid. fat and protein rise Dawn phenomenon smudgy effect feet on the floor instant sense damn instant sense damp insulin sensitivity why can I say sense of insulin low insulin sensitivity factor adrenaline highs insulin deficit growth hormone stacking insulin hydration Lata diabetes moody diabetes crutch crutch crush it and catch it see peptide and beta cell insulin onboard pump break barriers and today's episode dictate the pace. Once again. There are lists available on my social media. Check it out. Tell you what I'm gonna put it up on Instagram today then you'll be able to find it there in the Instagram wall or still I don't know what you kids call that story. Now that story. Now I don't know wherever you put the pictures. And it'll be on both my Facebook pages the private one Juicebox Podcast type one diabetes and the public page bold with insulin. Actually the defining diabetes series as well as the diabetes Pro Tip series is available at diabetes protip.com and juicebox podcast.com as well as those other places aforementioned. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. Hey, if you're listening in a podcast app follow and subscribe follow and subscribe follow in subscribe.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!