Episode #949 companion - After Dark: Dead Frogs
Katie's story of living with type 1 diabetes for nearly two decades. Despite her challenging upbringing and lack of support, Katie has found ways to improve her health and take control of her diabetes.
Katie, a 29-year-old woman from Washington state who has been living with type 1 diabetes for almost 17 years. Katie shares her story, discussing her experiences growing up with a mother who had health issues and her own journey with type 1 diabetes and other autoimmune conditions.
Katie reveals that she was diagnosed with type 1 diabetes when she was 12 years old. She mentions that while she is the only one in her family with type 1 diabetes, there are other autoimmune issues present, such as thyroid problems on her mother's side. Her grandmother, aunt, and mother have all had thyroid problems, suggesting a genetic predisposition to autoimmune issues.
The connection between autoimmune issues and type 1 diabetes is further explored in the discussion. Katie mentions that doctors believe her family's history of thyroid problems may have contributed to her development of type 1 diabetes. While she does not recall her family members having problems growing up, she recognizes the significance of their autoimmune issues in relation to her own diagnosis.
Katie also shares that she was diagnosed with hypothyroidism a few years after being diagnosed with type 1 diabetes. This additional autoimmune condition further emphasizes the genetic predisposition to autoimmune issues in her family. She recalls being initially prescribed medication for hypothyroidism but later being told that she was borderline and no longer needed it. However, a couple of years ago, she resumed taking medication for hypothyroidism.
The podcast transcript provides insight into the challenges faced by individuals living with type 1 diabetes and additional autoimmune conditions. It highlights the importance of understanding the genetic factors that contribute to the development of autoimmune diseases and the impact they can have on an individual's health.
Katie's story serves as a reminder that autoimmune issues can run in families and that having one autoimmune condition may increase the likelihood of developing others. It also emphasizes the need for comprehensive healthcare and regular monitoring for individuals with type 1 diabetes and other autoimmune conditions.
Overall, this podcast transcript sheds light on the experiences of a type 1 diabetic with autoimmune issues, highlighting the complexities and challenges associated with managing multiple autoimmune conditions. It underscores the importance of ongoing medical care, genetic awareness, and support for individuals navigating these health conditions.
Missed diagnosis of hypothyroidism
The podcast transcript begins with the individual discussing their experience with hypothyroidism and how it was initially missed and misdiagnosed. They admit to not paying close attention to the lab work and not fully understanding the symptoms at the time. When they switched physicians, the new doctor questioned the need for medication and advised them to stop taking it. This led to a decade without the necessary medication, during which time they continued to experience hypothyroid symptoms.
This missed diagnosis of hypothyroidism is a common issue in healthcare. The symptoms of hypothyroidism can be vague and easily attributed to other causes, leading to misdiagnosis or dismissal of the condition. In this case, the individual's symptoms were not properly recognized or addressed, resulting in unnecessary suffering and a delay in appropriate treatment.
The individual mentions that it wasn't until years later, when they started researching their symptoms, that they realized hypothyroidism may be the cause. They decided to get retested and started taking medication again. This highlights the importance of self-advocacy and taking an active role in one's healthcare. It is crucial for individuals to educate themselves about their conditions and seek second opinions if necessary.
The podcast also touches on the fear of being a parent and having their children experience similar missed diagnoses or mismanagement of their health conditions. This fear is understandable, as the individual experienced a decade without proper treatment due to a misdiagnosis. It emphasizes the need for ongoing monitoring and communication with healthcare providers to ensure that conditions are properly managed and any changes in symptoms or lab results are addressed.
The transcript also mentions the individual's experience with type 1 diabetes. They describe the typical symptoms they experienced, such as weight loss, excessive thirst, and frequent urination. They also mention a significant decrease in their physical fitness, which was attributed to the undiagnosed diabetes. This highlights the impact that undiagnosed or mismanaged health conditions can have on overall well-being and quality of life.
In conclusion, the podcast transcript highlights the missed diagnosis of hypothyroidism and the challenges associated with managing multiple autoimmune conditions. It emphasizes the importance of self-advocacy, ongoing medical care, and genetic awareness in order to properly diagnose and manage these conditions. The individual's experience serves as a reminder of the complexities of autoimmune diseases and the need for comprehensive and attentive healthcare.
Teen struggles with diabetes management
Teen struggles with diabetes management can be a challenging and overwhelming experience. In the podcast transcript, the individual shares their personal journey with diabetes and the difficulties they faced in managing their condition, particularly during their teenage years.
The podcast begins with the individual recalling a significant event in their childhood that prompted their parents to take them to the doctor. They attended a middle school football game with a friend and her parents, where the individual consumed an excessive amount of Coca-Cola due to extreme thirst. This raised concerns among the parents, leading to their visit to the doctor.
The individual's diagnosis story is described as relatively positive, with an adult who was not their parent recognizing the symptoms and urging their parents to seek medical attention. They were taken to the pediatrician, who tested their blood sugar and found it to be well over 600. This prompted an immediate visit to the emergency room.
However, there is a notable incident during this visit that highlights the lack of understanding or awareness surrounding diabetes. The individual's parents convinced them to go to the doctor's office by promising them a sugary drink from Starbucks afterward. Surprisingly, the pediatrician allowed them to stop at Starbucks and consume the sugary drink on the way to the hospital, despite the individual's dangerously high blood sugar levels.
This incident raises questions about the level of knowledge and understanding regarding diabetes among healthcare professionals at the time. It is possible that the pediatrician either did not fully comprehend the severity of the situation or believed that allowing the individual to have one last sugary drink would not have a significant impact.
The podcast also touches on the challenges the individual faced in managing their diabetes during their teenage years. They mention struggling with management and experiencing mental health issues. The individual's notes mention non-compliance, family dynamics, and diabolemia, which is a term used to describe the intentional manipulation of insulin doses to control weight.
The individual reflects on their teenage years and identifies a seizure they had during a sleepover as a significant turning point. This seizure may have instilled a fear of experiencing low blood sugar levels, leading to the individual intentionally keeping their blood sugars higher. This fear, combined with the challenges of adolescence and the pressures of managing a chronic condition, likely contributed to the difficulties they faced in managing their diabetes during this time.
In conclusion, the podcast transcript highlights the struggles faced by teenagers in managing their diabetes. It sheds light on the lack of understanding surrounding diabetes among healthcare professionals and the impact it can have on the individual's management and overall well-being. It emphasizes the importance of ongoing medical care, self-advocacy, and genetic awareness in properly diagnosing and managing diabetes. The individual's experience serves as a reminder of the complexities of diabetes and the need for comprehensive and attentive healthcare.
High school led to hiding diabetes
High school can be a challenging time for any teenager, but for those with diabetes, it can bring additional obstacles and pressures. In the podcast transcript, the speaker discusses their experience of hiding their diabetes during high school and the detrimental impact it had on their health and well-being.
The speaker recalls starting high school and feeling the need to hide their diabetes from their peers. They didn't want to be seen as different or have their condition be a topic of discussion. This desire to fit in and be like everyone else led them to hide their diabetes and not properly manage their blood sugar levels.
As the speaker entered high school, the number of students increased, and they felt more pressure to hide their diabetes. They didn't want to be judged or treated differently because of their condition. This fear of judgment and the desire to blend in led them to hide their diabetes even more.
The speaker also shares their struggle with guilt and shame when their blood sugar levels became high. They felt like they couldn't control their numbers and were unable to bring them down. The longer they ran high, the harder it became to lower their blood sugar levels. This cycle of guilt, shame, and feeling out of control further contributed to their desire to hide their diabetes.
The speaker admits that at the time, they didn't fully realize the impact of their actions. They didn't recognize the consequences of not properly managing their diabetes and the toll it was taking on their body. They felt the need to constantly hide their blood sugar levels and avoid testing altogether if the numbers were high.
This pattern of hiding and neglecting their diabetes led to a vicious cycle of feeling wrong, guilty, and ashamed. The speaker tried to bring their blood sugar levels back down but would quickly give up when something went wrong. This cycle of trying and failing only reinforced their negative feelings and avoidance of managing their diabetes.
The podcast transcript also hints at the development of an eating disorder later in high school or early college. The speaker explains that their body had become accustomed to running with high blood sugar levels, and whenever they tried to bring them down, they would experience physical discomfort and fluid retention. This further complicated their ability to manage their diabetes and added another layer of struggle to their already challenging situation.
In conclusion, the podcast transcript highlights the struggles faced by teenagers in managing their diabetes. It sheds light on the lack of understanding surrounding diabetes among healthcare professionals and the impact it can have on the individual's management and overall well-being. It emphasizes the importance of ongoing medical care, self-advocacy, and genetic awareness in properly diagnosing and managing diabetes. The individual's experience serves as a reminder of the complexities of diabetes and the need for comprehensive and attentive healthcare.
Neglected diabetes management leads to complications
Neglected diabetes management can lead to severe complications, as evidenced by the experiences shared in the podcast transcript. The individual interviewed describes a decade-long struggle with high blood sugar levels, resulting in various health issues such as shooting pains in the legs, fluid retention, lethargy, and constant nausea. These symptoms indicate the detrimental effects of uncontrolled diabetes on the body.
Despite the individual's efforts to do the right thing and manage their diabetes, their body seemed to signal that something was wrong. This internal conflict between what they felt and what they knew intellectually created a challenging situation. However, they pushed through, unaware of the potential harm they were causing themselves.
For a decade, the individual's A1C levels ranged between 10 and 14, which is significantly higher than the recommended range of 6.5 or below. This prolonged period of uncontrolled diabetes likely contributed to the development of complications. The individual mentions experiencing postural orthostatic tachycardia syndrome (POTS), characterized by dizziness upon standing up too quickly. They also underwent retinopathy treatments for their eyes, indicating damage to the blood vessels in the retina.
Considering the frequency of diabetic ketoacidosis (DKA) episodes, it is surprising that the individual did not have more severe complications. DKA occurs when the body lacks insulin and starts breaking down fat for energy, leading to the production of ketones. It is a life-threatening condition that can result in coma or death if left untreated. The individual admits to self-treating their DKA episodes with large doses of insulin to bring their blood sugar levels down. This dangerous practice could have potentially caused severe hypoglycemia, which can be equally life-threatening.
The individual's management of their diabetes was characterized by a cycle of neglect, DKA, and temporary normalization of blood sugar levels. They would eat whatever they wanted without dosing insulin, leading to high blood sugar levels and subsequent DKA. This pattern of behavior demonstrates a lack of understanding and control over diabetes management.
One striking aspect of this story is the individual's resistance to seeking help and their desire to keep their struggles hidden from others. As a teenager, they felt like a failure and believed they would never be able to figure out how to manage their diabetes. This mindset likely contributed to their denial and the lies they told about their blood sugar levels. This highlights the emotional toll that diabetes can have on individuals, particularly during adolescence when self-image and independence are crucial.
The podcast transcript also raises questions about the support system available to the individual. While they mention having family around, it seems that their resistance to letting others in hindered their ability to receive the necessary support and guidance. Diabetes management requires a multidisciplinary approach, involving healthcare professionals, family members, and the individual themselves. In this case, it appears that the individual's resistance to help hindered their ability to effectively manage their diabetes.
In conclusion, the podcast transcript highlights the struggles faced by teenagers in managing their diabetes. It sheds light on the lack of understanding surrounding diabetes among healthcare professionals and the impact it can have on the individual's management and overall well-being. It emphasizes the importance of ongoing medical care, self-advocacy, and genetic awareness in properly diagnosing and managing diabetes. The individual's experience serves as a reminder of the complexities of diabetes and the need for comprehensive and attentive healthcare.
Lack of support affected her
The podcast transcript reveals the detrimental effects of a lack of support on the individual's ability to manage their diabetes effectively. Throughout the conversation, the speaker reflects on their own experiences and the challenges they faced as a teenager living with diabetes. They express their frustration at the lack of understanding from healthcare professionals and their own resistance to acknowledging the impact of high blood sugar levels on their mental state.
One of the key points raised in the transcript is the alteration of the individual's mind due to high blood sugars. They discuss how elevated blood sugar levels can lead to feelings of irritability and short-temper, which became their normal state. However, they also admit to not wanting to believe that their diabetes was affecting them as much as it was. This denial and lack of awareness further hindered their ability to effectively manage their condition.
The individual's father, on the other hand, recognized the impact of high blood sugars and referred to it as the "high blood sugar monster." He understood the connection between uncontrolled diabetes and the individual's experiences and behavior. However, the individual themselves did not want to acknowledge this connection and resisted the idea that their diabetes was affecting them as much as it was.
The podcast host also shares an anecdote about talking to someone whose husband had uncontrolled diabetes. The host reflects on how the individual's high blood sugars likely impacted their decision-making abilities, highlighting the importance of recognizing the mental and emotional toll that diabetes can have on a person. They note that this aspect often gets lost in conversations about diabetes management.
The speaker then compares the slow progression of the negative effects of diabetes to a shadow creeping over someone as the sun goes down. They use the analogy of a frog in a pot of water slowly heating up to illustrate how someone can become accustomed to a detrimental situation without realizing the full extent of its impact until it is too late. In this case, the individual slowly became accustomed to the negative effects of diabetes on their mental state and overall well-being.
The lack of support from the individual's family is also highlighted in the transcript. The speaker admits to pushing their family away, particularly during their teenage years when they were volatile and out of control. They describe their mother as unstable, verbally abusive, and lacking support. This lack of support and stability in the home environment further contributed to the individual's struggles with managing their diabetes effectively.
In conclusion, the podcast transcript highlights the struggles faced by teenagers in managing their diabetes. It sheds light on the lack of understanding surrounding diabetes among healthcare professionals and the impact it can have on the individual's management and overall well-being. It emphasizes the importance of ongoing medical care, self-advocacy, and genetic awareness in properly diagnosing and managing diabetes. The individual's experience serves as a reminder of the complexities of diabetes and the need for comprehensive and attentive healthcare.
Lack of support, mental health
The podcast transcript reveals a lack of support and understanding surrounding mental health issues, particularly in relation to diabetes. The individual shares their experience of growing up in a household filled with constant arguing and a lack of emotional support. This environment made it difficult for them to cope with the challenges of managing their diabetes.
The lack of support from their parents is evident in their accounts. The individual describes their mother as someone who would either ignore their problems or change the subject because it made her uncomfortable. This lack of empathy and understanding created a barrier between the individual and their mother, leaving them feeling isolated and unsupported.
Similarly, their father's approach to their diabetes was focused on control rather than understanding. Instead of trying to communicate and support the individual, their father would simply tell them to "just do it" and inject themselves with insulin. This lack of emotional support and understanding from both parents further exacerbated the individual's feelings of isolation and depression.
The individual also mentions their struggles with mental health, specifically an eating disorder. They describe how they would limit their insulin intake to manipulate their blood sugar levels and control their weight. This dangerous behavior highlights the lack of awareness and support for mental health issues in relation to diabetes. The individual did not have the necessary resources or guidance to address their mental health struggles effectively.
Furthermore, the individual's relationship with their mother deteriorated further after their parents' divorce. The mother expected the individual to take her side and turn against their father, which strained their relationship even more. This situation highlights the impact of divorce on mental health and the importance of providing support and understanding during such difficult times.
In conclusion, the podcast transcript highlights the lack of support and understanding surrounding mental health issues, particularly in relation to diabetes. The individual's experience emphasizes the need for better education and awareness among healthcare professionals and families. It also underscores the importance of providing comprehensive and attentive healthcare, as well as fostering an environment of empathy and support for individuals managing diabetes and mental health issues.
Leaving toxic relationships improves well-being
Furthermore, the transcript reveals the detrimental impact of toxic relationships on one's overall well-being. The individual's experience with their mother showcases the emotional and psychological toll that such relationships can have. The constant arguments, gaslighting, and invasion of privacy described in the transcript demonstrate the toxic dynamics that were present in this particular relationship.
Leaving toxic relationships, as the individual in the podcast did by cutting off contact with their mother, can significantly improve one's mental health and overall well-being. The individual speaks about how removing themselves from this toxic environment allowed them to gain perspective and understand the negative impact the relationship had on their life. They were able to find peace and stability in their mental health, which ultimately improved their relationships with others.
The support and understanding provided by the individual's partner also played a crucial role in their journey towards well-being. Their partner recognized the toxicity of the situation and actively intervened to protect the individual from further harm. This support and validation were instrumental in helping the individual realize that they deserved better and that they were not alone in their struggle.
Leaving toxic relationships can lead to a newfound sense of freedom and empowerment. It allows individuals to prioritize their own well-being and surround themselves with people who uplift and support them. In the case of the podcast transcript, leaving the toxic relationship with their mother allowed the individual to focus on their engagement and the happiness they were experiencing in their personal life.
It is important to note that leaving toxic relationships may not be easy or straightforward. It often requires courage, strength, and support from others. However, the benefits of leaving toxic relationships far outweigh the challenges. By removing oneself from toxic environments, individuals can create space for personal growth, healing, and ultimately, a higher quality of life.
In conclusion, the podcast transcript highlights the transformative power of leaving toxic relationships. It sheds light on the negative impact of toxic dynamics on mental health and emphasizes the importance of prioritizing one's well-being. By leaving toxic relationships, individuals can reclaim their sense of self, find support from others, and ultimately improve their overall well-being. It serves as a reminder that everyone deserves to be in healthy and nurturing relationships that contribute positively to their lives.
Struggles with mental health and diabetes
The podcast transcript delves into the struggles faced by the speaker in relation to their mental health and diabetes. It reveals the detrimental impact of being in a toxic relationship and how it can exacerbate existing mental health issues. The speaker expresses gratitude for someone who stepped in and made them feel validated, as dealing with someone toxic can often make one feel crazy.
The speaker acknowledges that some of their mental health issues stemmed from the toxic relationship, but also recognizes that their depression and other concerns were largely influenced by their neglect of their diabetes. The fear and hopelessness surrounding their diabetes management led them to believe that they would never improve their blood sugars and would suffer from complications. This despair affected their relationships with others, as those close to them could see the impact of their deteriorating health.
The host of the podcast empathizes with the speaker, acknowledging that their parents also played a role in their struggles. While understanding that the speaker's mother may have had limitations, the host emphasizes that she was the person the speaker had to rely on, and her absence had a significant impact. The host also acknowledges that the speaker's father was going through his own difficulties, but still had a responsibility to support and help their child.
The speaker reveals that once they took control of their diabetes management and got their blood sugars under control, many of their issues began to dissipate. They found a great relationship with their father and met their husband shortly after deciding to take charge of their health. The speaker's depression improved as their diabetes management improved, and their life started falling into place.
The host acknowledges that the speaker's depression was a natural response to the challenging circumstances they faced. It is understandable that someone in their situation would feel depressed, given the lack of support and the overwhelming nature of their health struggles.
Looking towards the future, the host asks the speaker if they believe their life will significantly differ from the challenging first part. The speaker confidently responds that they know it will, indicating that they have overcome their struggles and have a positive outlook for the future. They also express understanding and empathy towards their parents, recognizing that they were likely scared for their well-being and unsure of how to handle the situation.
The podcast transcript ultimately highlights the importance of leaving toxic relationships and prioritizing one's mental and physical well-being. It emphasizes that toxic dynamics can have a severe impact on mental health and overall quality of life. By removing oneself from toxic relationships, individuals can find support, reclaim their sense of self, and improve their overall well-being. It serves as a reminder that everyone deserves to be in healthy and nurturing relationships that contribute positively to their lives.
Supportive husband helps with diabetes
In the podcast transcript, the speaker discusses their experience with their mother's mental health issues and the impact it had on their family. They mention that their father tried to help their mother, but nothing seemed to get through to her. Despite their efforts, the speaker expresses that they had to make the difficult decision to end their relationship with their mother in order to prioritize their own well-being. This decision was not easy, but they came to the realization that they couldn't expect something from their mother that she didn't have to give.
The speaker also mentions that their mother used alcohol as a coping mechanism, but there was no drug use involved. This highlights the complexity of dealing with mental health issues and the various ways individuals may try to cope with their struggles.
The conversation then shifts to the speaker's own journey with diabetes and their supportive husband. The speaker expresses gratitude for their husband's involvement and support in managing their diabetes. They describe him as being there for them whenever they need help or support, without overstepping any boundaries. The husband even offers to take over the responsibility of managing the speaker's blood sugars for a night, showing his willingness to alleviate some of the burden.
The speaker also mentions that they do most of the cooking in their household, indicating that their husband's support goes beyond just managing their diabetes. The speaker's husband's involvement in their diabetes management and their overall relationship highlights the importance of having a supportive partner.
The podcast transcript ultimately highlights the importance of having a supportive partner in managing chronic illnesses like diabetes. The speaker's husband's involvement and support not only help them with the practical aspects of diabetes management but also provide emotional support. This support contributes to the speaker's overall well-being and their ability to effectively manage their diabetes.
The transcript also serves as a reminder of the impact toxic relationships can have on mental health and the importance of prioritizing one's own well-being. By leaving toxic relationships and surrounding oneself with supportive individuals, individuals can find the support and understanding they need to thrive. The speaker's decision to end their relationship with their mother, despite the difficulties, showcases their commitment to their own well-being and serves as an example for others facing similar situations.
In conclusion, the podcast transcript highlights the significance of having a supportive partner in managing chronic illnesses like diabetes. The speaker's husband's involvement and support play a crucial role in their ability to effectively manage their diabetes and overall well-being. Additionally, the transcript emphasizes the importance of leaving toxic relationships and prioritizing one's own mental and physical well-being. By removing oneself from toxic dynamics, individuals can find support, reclaim their sense of self, and improve their overall quality of life.
Conscious parenting and personal growth
Furthermore, the podcast transcript delves into the topic of conscious parenting and personal growth. The speaker reflects on their own childhood experiences and the impact it had on their perspective of parenthood. They express a desire to break the cycle of unhealthy family dynamics and be a better parent.
The speaker acknowledges the need to be conscious and intentional in their parenting approach. They want to take the positive aspects of their own upbringing and combine them with new knowledge and understanding to create a healthier environment for their future children. This demonstrates a commitment to personal growth and a willingness to learn from past experiences.
The conversation also touches on the potential challenges of breaking these patterns. The speaker acknowledges that there may be moments where they unintentionally repeat behaviors from their own upbringing. However, they express confidence in their partner's ability to provide guidance and support, ensuring that they stay on track and make positive changes.
This discussion highlights the importance of self-awareness and self-reflection in the journey of conscious parenting. It is not enough to simply want to be a better parent; one must actively work towards personal growth and be open to feedback and guidance from trusted individuals.
The podcast transcript also emphasizes the role of external influences in personal growth. The speaker mentions the impact of listening to the podcast and how it led them to explore new options for managing their diabetes. This demonstrates the power of seeking out information and resources that align with one's goals and values.
Overall, the podcast transcript showcases the intersection of conscious parenting and personal growth. It emphasizes the importance of self-awareness, intentionality, and support in breaking unhealthy patterns and creating a healthier future for oneself and one's children. It serves as a reminder that personal growth is a lifelong journey that requires ongoing reflection, learning, and adaptation.
Importance of insulin pump settings
One specific topic discussed in the podcast is the importance of insulin pump settings. The speaker highlights that regardless of the specific insulin pump being used, whether it is Omnipod 5, Control IQ, or looping, it is crucial to have the correct settings in order to achieve desired outcomes.
The speaker mentions that they have tried multiple insulin pumps, including the 670g, the Tandem t:slim, and the Omnipod 5. They initially chose the Tandem t:slim because they believed its algorithm was more advanced. However, they eventually switched to the Omnipod 5 due to its tubeless aspect, which was more convenient for their active lifestyle as a runner.
This discussion emphasizes that the choice of insulin pump should not be solely based on the algorithm's capabilities but also on personal preferences and lifestyle factors. It is essential to consider factors such as tubeless vs. tubed pumps, ease of use during physical activities, and overall convenience.
The speaker also shares their experience of forgetting their insulin pump on multiple occasions, which highlights the importance of finding a pump that fits seamlessly into one's daily routine. Forgetting to reconnect the pump after showering or changing clothes can have serious consequences, such as diabetic ketoacidosis (DKA) or the inability to bolus insulin when needed. These incidents serve as a reminder of the potential risks associated with improper pump settings or forgetfulness.
Furthermore, the speaker's experience of forgetting their pump on the night before their wedding rehearsal demonstrates that unexpected situations can arise, and it is crucial to have a pump that can be easily managed and integrated into one's life. This incident also highlights the need for support and understanding from loved ones when managing diabetes, as the speaker's family dynamics were discussed in the podcast.
The speaker expresses gratitude for their current situation and reflects on the journey they have taken to reach this point. They acknowledge that while they may have made different choices in the past, it is impossible to know if the outcome would have been any different. This sentiment emphasizes the importance of acceptance and self-compassion when navigating the challenges of living with diabetes.
In conclusion, the podcast transcript underscores the significance of insulin pump settings in managing diabetes effectively. It highlights the need for individuals to consider their lifestyle, preferences, and support systems when choosing an insulin pump. Additionally, the speaker's personal experiences serve as a reminder of the potential risks and challenges associated with improper pump settings or forgetfulness. Overall, the podcast encourages listeners to prioritize their health, make informed decisions, and be proactive in managing their diabetes.
Embrace imperfection and keep growing
The podcast transcript also emphasizes the importance of embracing imperfection and continuing to grow. The speaker shares their journey of hitting rock bottom and realizing that they needed to make a change. They admit to being scared, but also recognize that this fear was a turning point for them. They made a conscious decision to no longer engage in self-destructive behaviors and to take control of their health.
The process of overcoming their struggles was not easy. It required a lot of work and effort. The speaker acknowledges that there were setbacks along the way and moments that felt like failures. However, they did not give up. They kept pushing forward, learning from their mistakes, and making adjustments as needed.
One of the key mindset shifts that the speaker had to make was unlearning the belief that certain blood sugar levels were inherently bad or good. They had to accept that blood sugars can fluctuate and that it is okay. Instead of dwelling on high blood sugar levels and beating themselves up over it, they learned to address the issue, fix it, and move on. This mindset shift allowed them to let go of perfectionism and the idea that everything had to be perfect in order to be successful.
The podcast host also shares their own experience with starting the podcast. They admit to not knowing what they were doing initially, but they took the leap and just started. They didn't wait for everything to be perfect before beginning. Instead, they learned and adapted as they went along. They embraced imperfection and allowed themselves to grow and evolve.
The underlying message of the podcast is clear: embracing imperfection is essential for personal growth and success. Perfectionism can be paralyzing and prevent individuals from taking action. It can lead to self-flagellation and a constant feeling of not being good enough. By letting go of the need for perfection, individuals can free themselves from this mindset and focus on progress instead.
Embracing imperfection also allows for learning and growth. It allows individuals to try new things, make mistakes, and learn from them. It encourages a mindset of continuous improvement and adaptation. By accepting that things will not always be perfect, individuals can approach challenges with resilience and a willingness to learn and grow.
In conclusion, the podcast transcript serves as a reminder of the importance of embracing imperfection and continuing to grow. It highlights the personal journeys of the speaker and the podcast host, both of whom have faced challenges and setbacks but have persevered and grown as a result. By letting go of perfectionism and embracing imperfection, individuals can free themselves from self-imposed limitations and open themselves up to new opportunities for learning and growth.
Monetizing podcast through unique experiences
One of the interesting topics discussed in the podcast transcript is the idea of monetizing a podcast through unique experiences. The speaker and the podcast host engage in a conversation about potential ideas for creating a special experience for their listeners and fans, while also generating revenue for themselves.
The conversation starts with the speaker suggesting the idea of having a meal together with a listener as a giveaway. They discuss the logistics of this idea, including the cost of airfare, accommodation, and security. They also consider the possibility of turning it into a larger event if more people participate.
Throughout the conversation, the speaker emphasizes the importance of keeping the money for themselves rather than donating it to charity. They express a desire to monetize their podcast and maximize their own profits. However, they also mention the possibility of offering exclusive content for a monthly fee, such as unedited episodes with cursing.
The podcast host, Katie, actively engages in the conversation and suggests additional ideas, such as creating a series where people can vent and complain about diabetes. This idea is met with enthusiasm by the speaker, who sees it as a cathartic experience for both the participants and their diabetic spouses.
While the conversation is light-hearted and humorous, it touches on the topic of monetizing a podcast through unique experiences. This approach allows podcasters to offer something special to their listeners while also generating income. By creating exclusive events or content, podcasters can incentivize their audience to support them financially.
The podcast transcript also highlights the importance of creativity and thinking outside the box when it comes to monetizing a podcast. The speaker and the podcast host brainstorm various ideas and consider different scenarios, demonstrating their willingness to explore new possibilities.
In conclusion, the podcast transcript serves as a reminder of the importance of embracing creativity and exploring unique experiences to monetize a podcast. By offering special events or exclusive content, podcasters can generate revenue while providing added value to their audience. The conversation between the speaker and the podcast host showcases their enthusiasm and willingness to think outside the box, inspiring other podcasters to do the same.
Podcast discusses potential giveaway idea
The podcast transcript begins with the speaker discussing the idea of a giveaway or prize for their podcast listeners. They mention that a monetary prize is not legal, so they need to come up with an alternative. The podcast host recalls hearing a podcast where the speaker had done something similar, offering the prize of being able to ask certain questions about diabetes. However, the speaker clarifies that they are thinking of something bigger, where they would fly to a location and spend time with the winner.
The speaker expresses concerns about potential issues that could arise, such as contracting COVID-19 or upsetting someone. They mention the possibility of a kid's head falling off if they get sick, which leads to a humorous exchange between the speaker and the host. Despite these concerns, the speaker still expresses a desire to make this giveaway idea a reality.
The podcast host suggests the idea of surprising the winner by showing up at their house, similar to what Ellen DeGeneres has done in the past. The speaker agrees and suggests holding a raffle where people can enter for a chance to win the prize. They discuss the amount of money that would be reasonable for the raffle entry fee, settling on $100. They also mention the possibility of doubling the prize if the speaker's friend Jenny joins them.
The conversation then shifts to the topic of podcast editing. The speaker mentions receiving an email from a company offering to edit their podcast, but ultimately decides against it. They express a desire for more time in their day but also acknowledge that they prefer things done their way.
The podcast host then asks about the speaker's daughter, Arden, and how she is doing. The speaker shares that Arden is doing well in school and has been producing impressive artwork. They express pride in their daughter's dedication to her artistic pursuits.
In conclusion, the podcast transcript serves as a reminder of the importance of embracing creativity and exploring unique experiences to monetize a podcast. By offering special events or exclusive content, podcasters can generate revenue while providing added value to their audience. The conversation between the speaker and the podcast host showcases their enthusiasm and willingness to think outside the box, inspiring other podcasters to do the same.
Community for type 1 diabetes
One of the key takeaways from the podcast transcript is the importance of community for individuals living with type 1 diabetes. The speaker mentions a private Facebook group called "Juice Box Podcast Type 1 Diabetes" as a place where people can find support and connection. This highlights the significance of creating a community where individuals facing similar challenges can come together to share their experiences, seek advice, and find a sense of belonging.
Living with type 1 diabetes can be a challenging and isolating experience. It requires constant monitoring of blood sugar levels, insulin injections or pump usage, and careful management of diet and exercise. Having a community of people who understand these struggles can be incredibly valuable. It provides a space where individuals can feel understood, validated, and supported.
The private Facebook group mentioned in the podcast transcript offers a platform for individuals with type 1 diabetes to connect and engage with others who are going through similar experiences. This online community allows members to share their stories, ask questions, and provide support to one another. It serves as a virtual support system that can be accessed at any time, providing a sense of comfort and reassurance.
Additionally, the podcast host mentions various series within the podcast that focus on different aspects of diabetes management. These series, such as the "Diabetes Pro Tip Series" and the "Bold Beginning Series," provide valuable information and insights for individuals living with type 1 diabetes. By offering this content, the podcast aims to educate and empower its listeners, further strengthening the sense of community and support.
The availability of resources and information within the podcast and the private Facebook group is also highlighted in the transcript. The speaker encourages listeners to visit the website and explore the different sections to find what they are looking for. This emphasizes the importance of accessibility and providing a wide range of resources to cater to the diverse needs of individuals with type 1 diabetes.
In conclusion, the podcast transcript emphasizes the significance of community for individuals living with type 1 diabetes. It highlights the importance of finding support, connection, and understanding in a community of like-minded individuals. The private Facebook group and the various series within the podcast serve as valuable resources and platforms for individuals to share their experiences, seek advice, and find comfort. By embracing community, individuals with type 1 diabetes can navigate their journey with a sense of support and empowerment.
Listen here or on your favorite audio app
This article was generated by AI.
Guest Post: Diabetes Glastonbury
Diabetes Glastonbury
Read Rob’s post from day one and two
If you don’t know, Glastonbury is a gigantic music festival in the UK. Over 5 days it deatures 2,000 different acts on 90 different stages. A town with the population of Buffalo NY is built in the Somerset countryside and lasts for just a couple of weeks before the fields are handed back to the dairy cows. You can’t make a plan because things distract you as you try to carry it out, you always want to be in two places at once, there’s mega-walking to do (I racked up 50,000 steps over 3 days) and the very best things (Jennifer Mahammadi’s talk on day 2 for me) are a complete surprise.
Glastonbury tickets 2020: Deadlines, sale dates and everything you need ...
Okay, so maybe it’s not exactly like Glastonbury
Happily, like the Sunday of Glastonbury, Day 3 of the Diabetes UK Professional conference are a bit more relaxed. The opening session was about early onset Type 2 diabetes. Not really my thing, but Professor Helen Murphy spoke of the importance of preparing women with diabetes for pregnancy. A lot of us worry about that for ourselves and our daughters and it surprised me that I hadn’t come across this idea. Here’s the message: If you’re planning to get pregnant (i) take 5mg of foli acid daily (ii) get your HbA1c down as low as you can, ideally below 43 (6.1%) (iii) check with your primary care doctor about medications that aren’t great during pregnancy such as blood pressure control tablets or statins. These things massively improve the odds of a successful pregnancy, to roughly the same level as the general population.
HbA1c<43 = Best chance of healthy baby. And get some folic acid.
Later on we heard about the future of CGM use in diabetes care. Personally, I found it a bit frustrating in several ways. The medics still aren’t getting just how revolutionary Dexcom and Libre have been for us. The HbA1c U shaped mortality study was referenced a lot. In a nutshell this massive 10 year study in China found that mortality increased when HbA1c fell below 5.7% and it also increased when HbA1c was over 6.7%. The study impresses because of it’s 10 year duration and the 35,000+ patients who were part of it.
But in referring to it the medics are overlooking a pretty gigantic factor: In 2012 Dexcom released the G4. In 2015 Abbott release Libre. These devices had had an utterly dramatic impact on the lives of those of us with Type 1. They make the Chinese study unhelpful at best and actively misleading at worst. Despite at least 2 people with Type 1 setting out to the conference just how much difference these things can make, the message still isn’t getting through. In terms of mortality below HbA1c <5.7, it’s akin to relying on a study performed before insulin was discovered in 1922.
It’s scary that the sexiness of big science seems far more important to some doctors than the value of providing treatment to individual patients. Hey ho. Rant over.
Median HbA1c down from 73 to 61 in 13 years – Well done HCPs! (And patients? Maybe?)
The final session of the day was presented by Professor May Ng, Dr Tom Crabtree and Dr Clare Hambling. Tom spoke on the success of the NHS England pilot to see the effect of closed loops on HbA1c in practice, May of the reduction in HbA1c among children using these systems and Clare on how they might be rolled out in practice. An idea she trailed was that of a national (international) helpline expert in all the different systems. Doctors sign up to practice medicine rather than IT but my own experience of AID is that it’s the techy side that’s the bigger problem, not the medicine. Comfortingly May also identified that whilst the UK is doing really well on diabetes care Sweden is doing even better. She didn’t mention the U shaped mortality study…
Complications: HbA1c really, really matters
So, that’s it from me at this year’s Glastonbury Diabetes Professionals Conference. It was an incredible privilege to be amongst these impressive HCPs. Their brilliance and commitment to the cause was beyond question. There’s going to be a lot of patients getting better care next week as the connections and ideas exchanged this week feed back into front line practice.
BOB
Rob (Bob Dee) Darbyshire
Guest Post: Grande Challenges!
Grande Challenges!
I thought Day 2 of the Diabetes UK Professional Conference might be easier. Maybe get some lunch and not spend so much time on my feet. I was a bit wrong. (Read Day One from Rob)
Ethnicity as a risk factor in T2
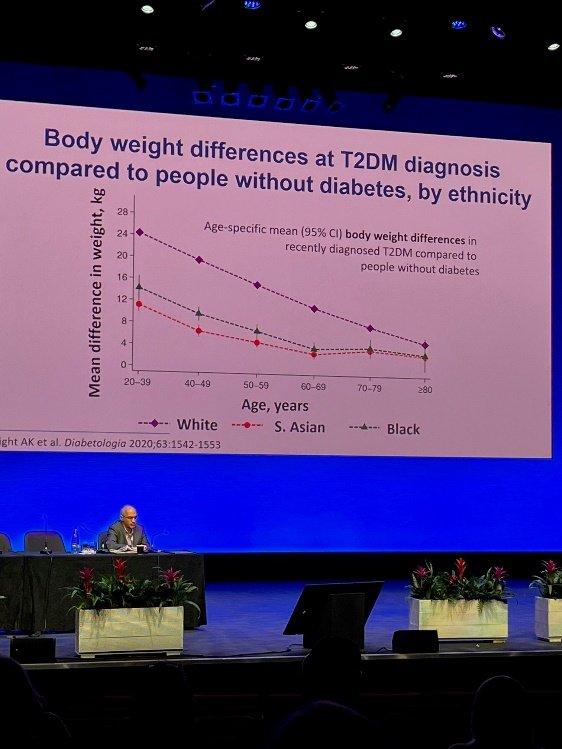
Today, I was able to spend more time in the presentations (and not just because I needed to sit down) mostly about diabetes causation and – drum roll - a cure. The day opened with an impressive lecture about the genetic links to diabetes. For me the takeaway was that Black and South Asian people develop type 2 when they’re skinnier than white people.
The rest of the morning I spent chatting with the awesome reps at Insulet and Dexcom. I got my hands on a Dexcom G7. It’s a real upgrade on my current Libre 2 because of the volume of real time data I could get out of it without a third party app. It’s small, really small, and much easier to apply than the G6. It may not seem important, but the box footprint is way smaller than the Libre 2 or the G6. This may sound trivial but with 3 Libre 2 users in the house, storage space is a genuine issue if we all get our scripts at the same time. Now I just need to persuade the kids to switch to Dexcom.
Omnipod 5 really is coming to the UK. And from what I heard, it may even be here sooner than we thought. The UK launch is going to be a “soft” one to avoid medics being hassled by all the current Dash and Eros users looking to upgrade. Cost shouldn’t be a barrier in the UK but appropriate staff training might be: HCP’s won’t be handing these out until they’ve been trained to use them.
The G7 is really, really tiny
After lunch we learned of the “Grand Challenge”. The Steve Morgan Foundation has donated an enormous £50 million to the prevention of T1 diabetes, and its cure through the development of robust stem cells that can grow into Beta Cells (without dying too quickly – that’s the barrier right now) and the development of smart insulins... that might be taken orally. As challenges go, “Grand” is an understatement.
Research on prevention seems the most advanced of these three things right now. Anyone who saw the slide I posted for the first day of the conference will recognise the increased risk of Type 1 among those with a family member already diagnosed. So far, as you can hear on Juicebox Podcast Episode #452, they’ve been able to delay the onset of Type 1 by around 2 years through the drug Teplizumab . As for a cure, it is progressing. As the implanted cells live longer and longer in their new homes, they present different problems over time. Slowly but surely, these problems are being overcome. As ever, we can look forward to a cure in ten years time… But real advances are being achieved already.
I finished the formal part of the day listening in to the discussions on eating disorders in diabetes. A shocking 40% of female teenage girls with type 1 in the UK suffer from a degree of diabulimia in which they consciously control their wait by avoiding injections. And it’s complex. We were addressed by the awe inspiring Jennifer Mahammodi. Jennifer was diagnosed at the age of 12. Her mother found it hard to help her manage with the result that there were a series of DKA hospital admissions – and Jennifer learned to associate those admissions with a time of caring and security, until she entered a cycle of almost fortnightly hospital admissions before being placed back into another foster care placement. Ultimately, living alone in social housing at the age of 19 she suffered, alone, a Christmas Day DKA episode so severe she could barely see. Thankfully, the adult care team at King’s College Hospital were able to provide psychological support and get her to a very much better place. It was a deeply moving address: amongst dozens of battle hardened HCPs there were very few dry eyes and it was the only address that I saw receive a standing ovation.
To cap off the day, I was invited to attend the presentation of a research award to Professor Roy Taylor. He’d been quite a presence at the conference putting questions to different panels with incisive intelligence and a dry wit. He pioneered the remission of Type 2 through rapid weight loss. As one of his colleagues pointed out to me, even if the diabetes isn’t remitted, weight loss is still a good idea for most Type 2s.
BOB
Rob (Bob Dee) Darbyshire
Guest Post: Diabetes Nerd Heaven!
Diabetes Nerd Heaven!
This week I’ve been lucky enough to get an invitation to Diabetes UK’s Professional Conference. As a poor muggle with no medical training beyond half a century of trying to tame the beast that is our collective family blood sugar, it’s quite a privilege. And it’s also a huge privilege to be able to share it with the Arden’s Day Blog. I’m hoping that some information about what goes on between the doctors when they think we can’t see them will be a helpful for insight for JuiceBoxers in the UK and around the world.
This year’s 3 day conference is taking place in Livepool’s Exhibition Centre and Arena. We’ll be kicked out on Friday to make way for Eurovision. Apparently, King Charles and Queen Camillahave been down to have a look at the venue this morning. As far as I know, they didn’t stop in for any of the lecture sessions at the conference. That’s a shame – they’d have learned a lot! It’s a huge event, with 4 or 5 simultaneous presentations. It’s been an 11 hour day for me there, and I’m looking forward to Manchester City vs Arsenal and an early night before the sae again tomorrow.
So – to business, A huge part of this event is networking. Over 2,000 Consultants, Junior Doctors, Diabetes Specialist Nurses, Academics, Practice Managers and so on and so on gather in Liverpool to renew friendships and share their experiences informally. So far, I’ve only managed to create one awkward silence by revealing that I’ve no medical training. But neither have I been asked how I achieve an HbA1c of 39 (5.7 in US numbers). Make of that what you will.
And I’ve learned! The first presentation of the conference was on “Nature or nurture” – the causation of diabetes. This comes up a lot as a question amongst us JuiceBoxers. Much of the chat was about Type 2 which is a really, really complicated question. For us Type 1’s Professor Ines Barrosso of Exeter University spoke of her research into the genes that are associated with Type 1. They’re now pretty clearly identified and partially explain this set of statistics:
The actual stats on family likelihood of developing T1, courtesy of Professor Barroso
But – and it’s a biggy – If one identical twin develops Type 1, there’s only a 40% chance that the other one will. And from that we can conclude that whilst there is a genetic component, there is also an environmental one. So it’s still your fault that you or your child lives with Type 1? You breast fed them, or not? You gave them anti-biotics or not? Nope. The “environmental factors” relating to causation of Type 1 are “largely unexplored” per Professor Barroso. What I take from that is that we cannot and must not blame ourselves, whether we have Type 1 or whether we have a child with Type 1. And that we need to support the research charities to find out what those causes are.
Type 2 is a different story. The impact of obesity is well understood. And there’s a genetic component. But for anyone who wants to say that one totally excludes the other – and this is the internet, we all know how it works – here’s a stat: The Pima Indians of Arizona and Mexico are the ethnic group with the highest incidence of T2 in the world, at 50%. But they’re a divided people. Those that live in Arizona, within the relative affluence and cheap calories of the USA, have rates above 50%, but their cousins in Mexico, in more straightened circumstances? 5%. The genes are playing their part, but so is lifestyle.
And other amazing things in brief:
• Get your doc or diabetes educator to give a talk in your child’s school. Not only will the kids learn something, but it’s a great way for kids who may not know each other to acknowledge each other as people living with Type 1. Having an ally in my year at school, or a couple of years above or below, would have gone a long way to addressing the loneliness I felt at school.
• Omnipod 5 really is coming to the UK. I can’t reveal when – because I don’t know exactly. But I can say that I won’t be ordering any more boxes of pods if I can get my healthcare team to switch me to a G6.
• Closed loop is coming as an “official” NHS supported tech in the UK. But don’t all rush for it at once. Rolling it out to every individual who may be eligible is going to take time.
• Dr Tabitha Randell of Nottingham University Hospital is a mega-star. Her patients are averaging an HbA1c in the 50s with minimal hypos. It won’t be a surprise to any JuiceBoxer that she’s a fan of getting a CGM on early and using a little bit more insulin, not a little bit less.
In terms of my wider experience of the HCPs, it’s become clear over the last 24 hours that the value of our “lived experience” is obvious to the clinical community. There are repeated statements about the need to listen to patients, ask what they want and ask how the medics can help. There’s real recognition, albeit with mixed levels of sensitivity, that the real experts in this condition are the people living with it. But… The Medical Establishment, like all great institutions, remains keen to look after itself before looking after the people it is supposed to serve. The word “safeguarding” is used in reference to patients, and deployed in a genuine effort to avoid damaging them. That’s great. But when it’s used to prevent those of us living with diabetes from damaging each other or ourselves it starts to be a bit weird. The internet exists. We sit alongside each other in clinics. We receive a monthly supply of a potentially lethal drug. We aren’t family pets that might or might not play nicely with other doggies. Peer support is coming as a pillar of care in the UK. It’s exciting. It requires clinicians to use judgement, tact and creativity to support it. From the guys I’ve met today, I think they’re going to be fine.
More tomorrow. Thanks for reading!
BOB
Rob (Bob Dee) Darbyshire
Guest Post: IronMan World Championship with Kris Freeman
I knew the IronMan World Championship course in St George would be hard... and it was. The 112 mile bike course had 7000 ft of climbing and the run featured unbroken climbs and descents that were several miles long. Shade was nearly nonexistent and the temp maxed out at 92 degrees in the mid afternoon.
My race plan was to start relaxed in the water, go slower for the first 60 miles of the ride than felt necessary and then see how fast I could go for the rest of the race.
My insulin strategy can be seen in the photos. I ran 1.3 units per hour until :15 minutes before my race (started at 6:45). Then I ran .6 u/h for three hours, .5 units for one hours, .4 units for one and a half hours and .25 units for :45 minutes at which point I tore the Pod off. The numbers in the photo are all .05 units lower than stated above because I was wearing a 2nd Pod that was delivering .05 u/h which is the minimum setting. In addition to the basal setting I also took a 4 unit bolus at the swim/bike transition with a syringe I pre filled before the race.
My swim was solid enough and I had no problems with my first transition. The terrain for the bike was very "western" with climbs that went on for miles followed by high speed descents that had me averaging better than 40 mph for several miles at a time. I took feeds at every aid station and probably consumed 12-16 twenty-four ounce bottles of Gatorade endurance 96 ounces of water, and a liter of Coke. I also took 8 Salt Stick electrolyte tabs. Choosing to conserve energy early ended up being a great call as my "easy" pace ended up being plenty fast and I never ran out of gas on the bike.
My transition into the run was also smooth if not super fast. I took the time to put vaseline coated socks on and chugged a full quart of water. However, my race got real hard a few miles later. I was overheating and I knew that I had to cool down or I wouldn't finish. There were aid stations every 1.5 miles and at each one I put ice in my hat and down the front and back of my suit. This was the first day of the year that I had worked out in any weather warmer than 70 degrees and my body was not happy with me. My half marathon split was far slower than I'd hoped (1:50ish) but at this point survival was the top priority. I bled tlme at each aid station but the ice and gatorade I was getting were the only things keeping me going forward. With 10 miles to go I was pretty sure I was going to get heat stroke at some point and I really wanted to get to the finish before that happened. I was stumbling and tripping over nothing as I ran on. My stomach was very nauseous and not at all happy about feeding. Even so, I forced about another gallon of Gatorade/water/Cola down my throat along with another 5 salt tabs for a total of 13 during the race.
I finished the marathon in 3:48 which was a good 20 minutes slower than I would have liked. But it wasn't for lack of trying. In the pictures you can see me striding across the finish and then taking a sharp left to get a cooler with insulin and fresh Pods from my coach. I went directly from there to the medical tent where I lied down on a Cot and proceeded to writhe around as doctors and nurses asked me how I felt. I had finished the race with a glucose of 140 so diabetes was not the main issue. I had all the symptoms of heat stroke including tingling/numb hands and feet and I began to dry heave. As the doctor decided to hook me up to an IV, I asked for a puke bag and started filling it. Fortunately the IV started to make me feel better pretty rapidly and I left the med tent under my own power about 40 minutes later.
All things considered the race went pretty well. It wasn't perfect but given the difficulty of the course and the heat it could have been worse. The consensus among the athletes I talked too was that this was the most difficult IronMan sanctioned event in the world. I finished in 10:13 which was good for a 19th place age group finish and 136th overall. I haven't been able to verify this but I think that these are the best finishes ever for a person with diabetes at the World Championships (If anyone knows differently please let me know). My result also requalified me for the 2022 World Champs in Kona this October though I chose to decline the opportunity. - Kris Freeman
Episodes of the Juicebox Podcast featuring Kris Freeman
#26 Olympian & person with diabetes Kris Freeman