#621 One Happy Camper
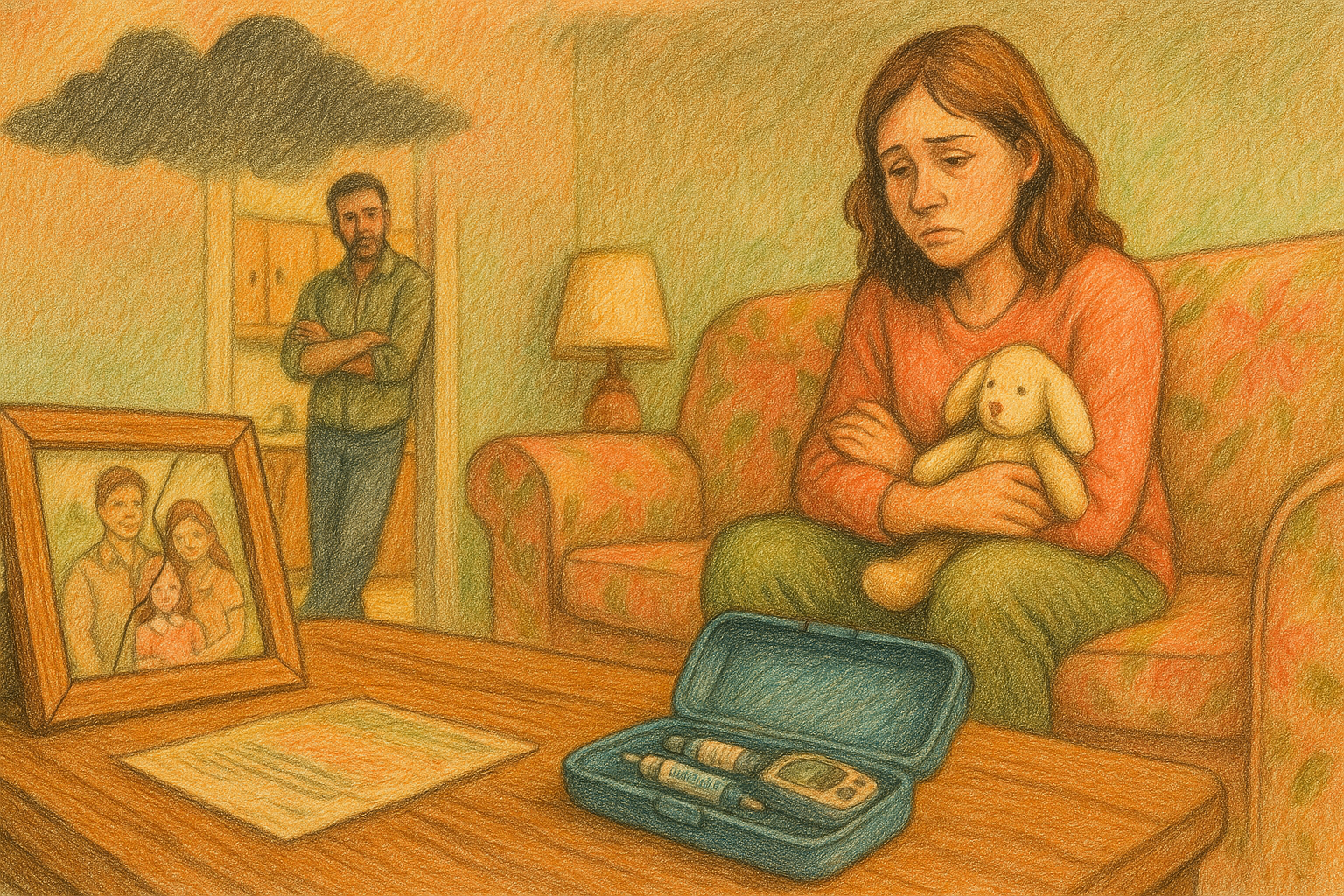
Kelsey is an adult type 1 who loves diabetes camp.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 621 of the Juicebox Podcast.
Today, you have the great pleasure of listening to me speak with Kelsey. She's an adult who's been living with type one diabetes for quite some time, and she has a passion for helping people with type one. When this was recorded, Kelsey was the Community Relations Coordinator for the Chris Dudley Foundation. She since has moved on to be the Director of Operations at Gales Creek camp foundation. Kelsey likes helping people with type one diabetes, and she loves diabetes camp. I think she might even like, now you'll find out. I'm not gonna spoil it all here. Please remember, while you're listening that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan. We're becoming bold with insulin. If you're a United States resident who has type one diabetes, or is the caregiver of someone with type one, please do me a favor and go to T one D exchange.org. Forward slash juicebox. And join the T one D exchange registry. Taking the survey only lasts a few minutes. You can do it from your phone. It's super simple to do. Hold on, I got away from music. Wow. It's completely HIPAA compliant. 1,000,000% Anonymous, and it's going to help people living with type one diabetes and benefit the Juicebox Podcast. I would really appreciate it if you went to T one D exchange.org. Forward slash juicebox and filled out that survey today. Thank you very much. Just one more thing. This show is sponsored today by the glucagon that my daughter carries. G voc hypo Penn. Find out more at G voc glucagon.com. Forward slash Juicebox.
Podcast a Mac. Yes, you go to the Apple in the top left corner of the screen. Uh huh. Go to System Preferences. Sound. bottom middle.
Kelsey Duman 2:25
Bar bottom, it'll show up. There it is.
Scott Benner 2:28
Then the sound effects tab. midway down, it says play sound effect through and there's alert volume slider slide all the way to the left. Okay, don't close that. Because after you're done, you're gonna want to remember to slide it back to where it was and close your system preferences. So you will hear the next time you get an email, but we're not going to hear it again for the next hour.
Kelsey Duman 2:50
Okay, it says there's one chapter that says play user interface sound effects? Yep. Does that still be checked? Yeah,
Scott Benner 2:57
it's just the slider, you're just basically turning the volume down. And then you won't get those notifications. I mean, you'll still get them you just won't be able to hear them. Okay, you slide it back when you're finished and and quit the preferences near right back restarted. Awesome. Okay. I'm just afraid if you close the Preferences now that offer hours now you have 300 emails in here. But that's perfect. Thank you. Yeah. Okay. So when you're ready, and I know you're probably not nervous, or you know, you should be that we've talked before. Yeah, well, that was what I was thinking too. But just introduce yourself and we'll start off.
Kelsey Duman 3:40
Awesome. Well, my name is Kelsey Duman and I have had type one for gosh, 22 years now. And I work with diabetes camps, and kids and teens and families with type one. And I am a big fan of the Juicebox Podcast. So I'm excited to be here today.
Scott Benner 4:01
Well, then I feel badly starting off with in a way that could be taken as creepy. But if you've had diabetes for 22 years, and I'm looking at this photo of you, are you 24. Like what's going
Kelsey Duman 4:09
well, thank you. I appreciate that. I'm actually 29 No, please. So I was diagnosed when I was seven,
Scott Benner 4:16
seven. Gotcha. Okay, so you said a second ago, which I'll just leave in so people have contacted you're not nervous because we've spoken to each other before? Yes. So what came first? The Chris Dudley or the egg? Did you book him? Before yourself? Yes. Before him.
Kelsey Duman 4:40
I booked him. Well, I it was kind of at the same time actually. I had reached out to Scott to see about being on the podcast and if it was something that you know if there was some little nuggets of info that the listeners would be interested to hear from me and one thing led to another and I brought up the podcast, Chris He was excited to join as well. So
Scott Benner 5:01
okay, so Chris's episode is all edited, and it's in the queue. Yay. It'll be up very soon. Maybe next week. Awesome. Nice. And then somebody will hear this six months from now and go back and look for it. Like, it's the second like, it just happened. But right. Back in June, you just did something that captured my imagination. You said I reached out to Scott, do I feel different to you talking to you, then the entity that you believe you're emailing? Or is that just a misstep of words? Hmm.
Kelsey Duman 5:34
I don't know. That's a good question.
Scott Benner 5:35
That's a cool maybe are multiple people to multiple people. Maybe you guys.
Kelsey Duman 5:40
I mean, it's so funny with podcasts being such you know, a phenomena right now. You you imagine someone when you hear their voice, right? And then you get to talk to them more in person, or we had talked over zoom and you're like, oh, wow, there's like a person behind the voice.
Scott Benner 5:55
I don't seem that much different. Like when I'm not being recorded, right? No, not at all. I mean, I don't think I am but when this had been an odd time to be few been like, Yo, no absolute you're kind of a prick. And I didn't even know who I am. Truth hurts, right? Oh, no, I'm gonna have to take that in. Well, okay, so you diagnosed when you were seven? You said? Yes. That's pretty young. Any in the family? diabetes wise?
Kelsey Duman 6:25
No, I actually, it's crazy. My entire life. I've been told, you know, there was no family history, yada, yada. And then just like a year ago, my dad was like, Well, I think maybe my leg Great Aunt once removed hat. It was like, what? Where's this coming from?
Scott Benner 6:43
Who's a great, I don't even know how to track that.
Kelsey Duman 6:46
I know. Me neither. I was like, does that truly count as like genetic connection? So make the baby I guess is the answer. But not that not that I really know of.
Scott Benner 6:59
So basically, like his sad third cousin who couldn't get a date one Thanksgiving that he meant. He right. Yeah, the 70s.
Kelsey Duman 7:06
Exactly. Exactly. Well, but yeah, I have two brothers. And they both don't have it. Neither my parents. So
Scott Benner 7:14
I just thought of a question I don't think I've ever asked before. So what does it feel like to? Does that feel separating? That you're the only one?
Kelsey Duman 7:25
Oh, um, you know, not for me personally. And my dad and my mom, both were super involved in different ways. Growing up with type one, and I think it almost made it more of a family affair, if you will. And so it didn't, it didn't feel separating from my family. My mom was really hands on with the management part of things. I mean, she had like carb counts memorized on every single thing. And then my dad was super good about working with me on advocacy stuff. We went to the JDRF children's Congress when I was 11. And got to go talk to our nation's leaders about funding diabetes research. And so he was really formative in kind of how I've accepted having type one. So I think they really need it more of a positive and something that they saw as just something that helps shape our family. And so it never felt like I was just out on my own island.
Scott Benner 8:33
Empowering,
Kelsey Duman 8:34
even Yeah, absolutely. Absolutely.
Scott Benner 8:37
What what did management look like 23 years ago? When did you start regular mph?
Kelsey Duman 8:44
I did start regular mph. quickly changed though. I got on a pump when I was 10. So by the time I really can recall management. I was on a pump. I do remember the one time my mom mixed up my regular and NPH. And we were just like, what do we do? You know, you get you can't mix him up. She like did the wrong dose of one. And I think I remember that because there was so much panic in that moment. But yeah, by the time I could really remember and by the time I really took some ownership of it, I had the old school animist pump that was like the size of a brick. And obviously no CGM. It was all testing. I always think back of my least favorite part of growing up with diabetes was the log book. And you had to write down your blood sugar every time you tested and record your exercise and oh my gosh, killed me.
Scott Benner 9:52
I think the podcast exists partially because I didn't want to do stuff like that. And I thought I could really figure it out. I wouldn't have to write anything down and anybody about it ever again? We made this ownership of diabetes. When did that transition begin for you? Do you recall?
Kelsey Duman 10:08
Yeah, um, you know, I always I talk with parents about this a lot at camp sessions, because that's a huge question, right? Like, when do you let your kid take some ownership? How do you do that? What if they don't want to. And I feel like for me, it was kind of a slow burn, if you will. I think once I was on a pump, it, it my mom was really good about giving me those little nuggets of ownership. Even as far as like, Okay, here's what your carbs are, here's how much insulin you should take, you put it in the pump, I'll double check it just in case because you're 10. But you put it in the pump, and you press the go button. And so just those little bits of building blocks. I would say high school was definitely when I started to take more of a lead role in my management. And my I always think back my parents, you know, when you're, you know, having a daughter with type one when you're in middle school, and you're getting invited to sleepovers, and the parents are like, Okay, well, how do we manage this, especially back then when there was no Dexcom share? There, I didn't have a cell phone type of thing. And so their rule was you can go to whatever sleepover you want, when you can prove that you can wake up in the middle of the night and test your blood sugar to make sure you're still good to go. They put it on you. Yeah, yeah. And it was, I mean, I felt like that was fair. Because if you know, that's what I needed to do to be responsible enough to take this next step of going away on sleepovers. And it took me a little while to wake up and not just turn off the alarm and roll over, but to actually wake up and test and yell down the hall that I was 150 You know, that's so
Scott Benner 12:00
that's lightful and important to talk about, actually, that you can't just make an ask of a kid and expect that, you know, by next Thursday, it's all going to be buttoned up and going the way you want it to like it could take weeks or months of you turning off that alarm and being like I can't do this and until until you find your your rhythm within a little bit.
Kelsey Duman 12:19
Yeah, for sure. For sure. And there was they had good compromises, you know, it wasn't like oh, you can't go hang out with your friends because you can't do this because you have diabetes.
Scott Benner 12:37
G voc hypo pan has no visible needle, and it's the first premixed autoinjector of glucagon for very low blood sugar in adults and kids with diabetes ages two and above. Not only is G voc hypo pen simple to administer, but it's simple to learn more about. All you have to do is go to G voc glucagon.com Ford slash juicebox. G voc shouldn't be used in patients with insulinoma or pheochromocytoma. Visit G voc glucagon.com/risk.
I don't do this often. But I saw post on my Facebook page the other day. By the way, Juicebox Podcast type one diabetes, private Facebook group 20,000 members go join. There was a post about the T one day exchange it said if you're not on the T one day exchange, you like making some extra money every now and then. And you love contributing to type one diabetes research. Go join. This person says I've done three studies in the last six months currently being paid to upload a couple of pictures every day and take a survey for 16 days. Easy peasy. And it's for the greater good of T one D tech. I'm sure Scott has a direct link so you can benefit the podcast as well. Well, she's 100%, right I do T one D exchange.org forward slash juicebox. When I tell you about the T one D exchange, I never bring this part up because it doesn't come to fruition for everyone. But it is a sincere possibility that the T one D exchange may offer you other opportunities after you take the survey. So you have to be a type one who's from the United States or the caregiver of a type one in the United States. You have to go to T one D exchange.org. Forward slash juicebox fill out the survey takes less than 10 minutes. It's HIPAA compliant and anonymous. And then you're in they'll follow up with more stuff if there's opportunities available and if not, you've done a great thing you're helping people with type one you're helping the show. So I'm just taking the survey is a big help. But there may be more. Anyway, I don't usually talk about it like that because I just want you guys to do it because you want to do it but you see people are excited about there's a lot of comments in this thing about other people who have done it? And I just thought maybe I should tell you t one D exchange.org. Forward slash juicebox. Go fill out the survey.
Yeah, they didn't lock you in a dungeon if you couldn't do it, right, right,
Kelsey Duman 15:17
right. Like I could go spend the night at my cousin's house because they my aunt was trained and everything. But it just seemed like it made sense. Even, you know, 1213 that, if I wanted to go off on my own, I had to learn to do this stuff on my own. So I wake
Scott Benner 15:31
up every night to test your blood sugar.
Kelsey Duman 15:36
So my parents in the beginning woke up, I think almost every night at 12. And three, yeah, they then you know, they kind of found their own rhythm. I think because I started waking up. So early to test myself. In the middle of the night, it became almost this like, habit. And I actually when I was like, 17, or 18, my endocrinologist sat me down and was like, you can sleep through the night, it's gonna be okay. But it almost became this anxiety of like, well, I have to wake up at 12 and test and see what I am. And my I had an amazing endocrinologist growing up, and she she was like, almost giving me permission to you know, as long as you're at a good range, before you go to sleep, you got to trust your body.
Scott Benner 16:23
To describe that a little bit. If you if you were to get up every night at midnight and test and always have a good number, like, you know, good meaning you felt comfortable about it. Right? What would stop you the next night from not getting up? Is it just like, This is gonna be the day?
Kelsey Duman 16:40
Yeah, you know, honestly, I think I really needed that almost permission from my doctor. Because my mom had said, you know, you're not getting enough sleep, you're, you're also a teenager, right? Like, so it's like, you know, your body's growing, you have to get more sleep than you have been getting. And it was, I mean, it was really tough, honestly, to let myself trust my body and trust the Basal rates that we've, you know, looked over and over. So,
Scott Benner 17:12
yeah, I agree. I just I was wondering how it struck you. So how do you? I mean, we kind of glossed over it a little bit. So do you work at a lot of different camps? Or do you work specifically for the Chris Dudley foundation.
Kelsey Duman 17:25
So right now my full time job is with the christeli Foundation. But I love being involved with as many diabetes camps as possible. I actually got my undergrad degree in psychology and camp management. So it was super fun to be able to apply some of my education to it. And then right now, I'm getting my master's in nonprofit management, which, as any camp lover would know, many of them are nonprofits. But I work really, really closely with another diabetes camp here in Oregon called Gales Creek camp. And they host nine camp sessions all throughout the summer. And then I've worked closely with riding on insulin, which is a ski and snowboard camp for kids with type one. And then I work a lot with the diabetes camping and Education Association, which is kind of the hub of all the diabetes camps.
Scott Benner 18:22
So what's the, in your, in your mind? What's the goal of diabetes camp? For the attendee,
Kelsey Duman 18:30
for the attendee, the goal of diabetes camp is, and this is broadly speaking, right? Because a lot of them focus on different aspects, but giving kids the tools and the self confidence to not only live well with type one, but really embrace type one and, and use the skills that brings into your life to take them further and other aspects of their life.
Scott Benner 18:58
Okay. I have to just take a detour for a second I love your generation because you have I think three times in the first 16 minutes that we've spoken made sure not to generalize your answer you'll say well in my you know experience or for me or in this set, it's very you guys don't generalize like older people are just like if you asked me a question, I will answer it answer it empirically as if the answer in the whole world and I know that's not like particularly right and I do try I think I'm doing a better job of not answering that way and talking like that as I get older but you guys are so aware of it. Like that's it's nice. I don't know another way to put it really I just but I hear it every time like it hits Oh, interesting a little tap on the back of my head like oh, she was really careful they're not to generalize any well and I
Kelsey Duman 19:49
think I'm sure you've noticed this, you know, talking to all of these different people with type one who are who work in type one. Like it everyone's journey is so different with type one, you know, you can just realize in the sense of we all wear a pump or we all take insulin, but I mean, everybody has their own experiences and their own outlook on life with type one.
Scott Benner 20:09
No, no, absolutely. I don't think you're wrong in the least. But I think you're 1,000,000%. Right. I'm just so aware of it when it happens, which makes me think back to when I was younger, we must have just blurted out the first thing that occurred to us. That was the new role. Right? Yeah. I don't know. That's interesting. So So okay, so you come to camp, basically. Is there any way in your mind that this podcast is virtual camp?
Kelsey Duman 20:37
Oh, absolutely. Okay. Absolutely. Yeah. I mean, it's so cool growing up. So I started going to camps, diabetes camps, right after I got diagnosed. Gales Creek camp who I work closely with, do a family camp. And so I was diagnosed in May, when I turned seven. And that July, my family and I were at family camp. And so like, I have just grown up through the system, if you will. But as I've gotten older recently, you know, the diabetes online community has just taken off. And it's so cool to see aspects within podcasts or Facebook groups of that diabetes community that when I was younger, it felt like camp was the only place to find that now in these new formats of support.
Scott Benner 21:23
Yeah, I think that all the time. I don't, I don't ever say it out loud, I guess that I don't see the difference between all those things just listed, get Facebook, right, listen to this, go into camp, it's the idea of first seeing that there are other people have diabetes. And there they are right in front of you. They're not weird. Like, you're not the only handsome person with type one. And everybody else is just you know, hunched over and a ball, you know, that I don't I don't mean like that feeling that even you could maybe even feel like, well, those other people are sick, but I'm not. Right. And then you see other just completely normal people walking out and you and you see yourself in them. And that's comforting. And inclusive, it makes you feel it makes you feel like surrounded in a good way. And then you hear people's ideas. Now I've had people come on here and tell me that some of the I had somebody on recently talking about a, an eating disorder. And I don't think the episodes up yet, but the person said that all of the you know, I'm making air quotes, best eating disorder tips came from camp, because that's where that's where they learned how to manipulate their insulin, and everything from other people who were already doing it in a time where it's just years ago, not that it couldn't happen, right today, but But years ago, when it was harder to like, track your data, even, like they taught her how to like, like, you know, cheat and or log books or test tests, when they knew, you know, they were, they were to certain number or use urine strips, but put one or put water on them. And they would come back just reading like normal, like, right, that kind of stuff. And so, in my mind, as I'm being told that story, I think it would be easy for people to listen that and think well, so you can sped. But I just think that in every walk of life, you have the opportunity to take the good or the bad from something, there's always going to be a mixture, right, it's up to you what you're going to take from it. So while that person's recollection was that camp taught me how to do things I wasn't supposed to do. I don't really believe that I think that, that there are ants, especially in today's world with the internet, the you know, as as completely readily available as it is, you could find out anything, like I could run, I could learn anything in the next five minutes if I wanted to. So you kind of have to want it, I think,
Kelsey Duman 23:50
for sure. And I think, you know, being at camp, you are in a cabin in the middle of the woods, usually with kids your own age who all are experiencing the same thing. And that's what you have in common, right. So it's crazy, like some of my best friends are from camp and they're people that I probably if I met them on the side of the road wouldn't have become best friends with them, just because we're so different. But you have those shared experiences and the same daily challenges. And it just you connect on that different level. And so obviously, those conversations are going to come up. And like you said, you take what you want from it. So obviously not great that camp was a source of damaging information for her in that sense. But you're there's also, you know, probably tenfold the amount of good information that kids can take. I would know and and just those tips. I mean, you're talking about the tips of of I'm assuming probably dying bulimia Yes. But the tips of you know what to do when you're feeling like you know, diabetes just sucks and I don't want to do that. This anymore. And you know, I've had conversations with kids that are struggling with eating disorders, but they feel like there's that safe space where they can talk about it. And whether they're approaching it from a, this is what I'm doing. And I'm not sure if, like how I feel about it, or I need help. And no one else understands how I'm doing this to myself. And so I need to talk to someone who really understands diabetes to really get this. It just creates that that almost internal community. And you're out for a week and most of the camps don't allow kids to have their cell phones with them or internet or anything. So you're with the people you're with. And it just creates that that open space of just talking through those things.
Scott Benner 25:46
How do you negotiate that? Because that seems like such a great idea to leave your cell phone at the door kind of how do you how to even hear comedians talk about it now like if you go to see comedy live, they'll they they there's a there's literally an industry around bagging people's cell phones at live events. So interesting, so that your phones Stay safe, and it's and protected. And they can get back to you because you can't come into the into their performance with a cell phone because the comedian doesn't want to be up there thinking you're about to take four words that they say and turn it into some, you know, misrepresented or something like that. They want to be free to talk. So I love the idea of those kids coming into the camp, leaving their electronics behind. But how do you do that when their electronics are their insulin pump? Were there CGM to?
Kelsey Duman 26:33
Yeah, yeah. I mean, that's a huge concern among parents, for sure. But there's, like I said, I work with the diabetes education and camping Association. And they've done a great job of kind of helping camps figure out ways where you don't need your cell phone to access your Dexcom. So right, if a kid has a T slim pump, they ask the kid to put take the Dexcom off their phone, turn in their phone, and then rely on the Dexcom that's on their pump. I think what you said in the beginning there of how do you negotiate that with like these teenagers who are glued to their phone any other day of the week, and they're showing up at this place where maybe they've never been, and now you're asking them to give up their like, safety blanket. And I think sometimes it's a little tough, but I think kids can be more logical than we give them credit for. And so when they understand that, you know, like at christeli basketball camp, we're going to be playing basketball all day, like the only breaks you're going to get are for meals and snacks and to test your blood sugar if you feel low. So they kind of get like, Well, okay, I'm going to be busy. I guess I won't have time I don't want my phone to fall out on the court and break. And actually, at christeli basketball camp, we have them turn it in, kind of like you're talking about with the comedy guys and put them in a bag, put their name on it. And then it goes in the camp store. And there's an hour period in the afternoon where they have some free time they can shower, they can go to the pool, and they're allowed to check their phone out just to check in with mom and dad or whatever. Yeah, notice. Yeah, exactly. Right. But we've noticed that a lot of them just leave their phone there. Right. And it's I think it speaks to how we've built that community and that kind of positive energy of like, building connections with the people who you're with, because they are showing us that they'd rather hang out with their new friends then get on their phone and go on Instagram or Tiktok or whatever.
Scott Benner 28:42
No, I mean, that that aspect of what you're saying is magical. The idea that they wouldn't have a phone too. I mean, because what does a phone really do? Right? It stimulates you in a way that real life almost can't, you know, and, and so it feels better. It's more comfortable. It's soothing. You know, it's all the things that talking to a person should be or playing basketball or something like that. But um, I'll use my daughter as an example, if you took Arden's phone from her. She's she's done. Like she's looping, right? So Right. She can't like, you know, would you ask her to go on MDI while she was there?
Kelsey Duman 29:16
Oh, that's true. Because you're looping Yeah.
Scott Benner 29:19
To be near her.
Kelsey Duman 29:20
Yeah, that's a great question. You know, what's interesting with the last couple years of COVID interruptions, is we haven't had the chance at least to Crystal the basketball camp to have a looper at camp. Yeah. And like, I know, Chris himself loops and so he's all for it. But because we haven't had camp the last couple years, we haven't had a chance to see what that would look like. And I think I think honestly, the if it was, you know, only up to me which there's a whole team of medical professionals that would make these decisions, but from kind of a Camp Director mindset, if you will, I obviously if she needs her phone as her pump, she needs it right. Like that's a non starter. And so I think it would be a, a question of okay, so can you, you know, turn off the data, keep on your Bluetooth and and I looped for a little bit, but it's been a while. And really just whether she has her phone and it's just functioning as the pump and CGM, and it's not a, she's sitting on her phone talking to her friends, which she doesn't sound like she would kind of kid that would do. Well, that's,
Scott Benner 30:39
you know, what's interesting is, we've, we've come so far in society where you can't like, I imagine a time where you tell the kids look, you're here, I know, you own a phone, but you don't use it. And then they actually listen to you. Like, right, that to me would be the pinnacle of this, this concept actually teaching people to integrate their This isn't your job at camp, but but it would be nice if people could actually understand how to integrate technology into their lives without allowing the technology to take over their life. Right?
Kelsey Duman 31:09
Yeah, sure. Yeah, well, and I know other camps, like Yale's Creek who I work closely with, they don't have cell service out there. So they don't have to do as much as we do with like, protecting the phones and putting them in their own little box so that the kids aren't tempted with them. Because they're it's you know, if they're looping great if they're not there phones, just kind of an iPod type of a thing. So Kelsey, I
Scott Benner 31:34
think that was an odd Oregon flex you just did there. You're like we have cell service where we're at. You know, I just imagined Oregon to be like, a countless acres of 300 foot tall trees that are four feet from each other and nothing. Is there. I mean, that's pretty much what it is. Yeah, you have you have granola weaved into the dreadlocks under your arms right now. Is that right? Exactly? What? Okay, let me make you the king of the world for a second. Oh, okay. And, and but we'll keep you in your camp. Space. What could diabetes can't be that it currently isn't?
Kelsey Duman 32:15
Oh, gosh. Wow. That's a great question. Of
Scott Benner 32:18
course it is. That's why the podcast is listened to by many, many people. But don't ask the silly questions. I want to know, here's what I think when I'm talking to you. I'll give you a chance to think for a second. Yeah, I think young, smart type one, you're married to type one, which I don't even think we've gotten to yet right? Eventually, you're gonna have a baby. It's gonna like how we come out with an insulin pump on its forehead or something like that. So what, like, Do you dream or like, Well, you're in fairness, some people go to work, and they like facilitating and doing a job. And some people will live their whole lives doing that. And some people are at work thinking this could be better. This could be like, Are you a person who thinks about how to make things better? Or are you taking a lot of joy out of making the machine work?
Kelsey Duman 33:05
No, for sure. I definitely am always thinking about, you know, how can we change this? How could we improve or expand? Really? Yeah,
Scott Benner 33:14
we're getting more out of it even like, make Yeah, something. Maybe there's an I always think this about everything. Like maybe this thing has a purpose that we don't know yet. And like, What could this thing do? If it was all together like this, if we if we like wiped away all the norms that were in our heads, and the way we think things are supposed to be? Like, what's the opportunity here? We're bringing kids together, they're at camp with an, you know, oh, you know, operated by a type one who was a long time NBA player. So super exciting. Plus, you're in Oregon, and you have cell service. You people are like, literally like kings, you know, Thrones with your cell service. We're like, what? What's there that that's right in front of you that you don't see or that you see, but it's hard to get to happen. Like, that's what I want to know, like, how do you make it more than it is?
Kelsey Duman 34:07
So the first thing that comes to mind, and I'm sure there's so many different routes I could take with my thought process in this. But, you know, kids go to camp, and then they age out. And that's it. Right? And it's interesting because I'm sure and you I mean, Arden 17 Right. Oh, in a couple of days. Oh, wow. Well, Happy Birthday Arden. Um, but like you're gonna get to that point that I, you know, have gone through as a young person with type one where you're transitioning from high school to college and then college to the real world. And there's so much change in that for anyone. But then you add type one on top of it and it's there's so much to just kind of wrap wrap your head around psychologically and physically and Basal right why's that that's like a huge transition point for young adults with type one. And I think I mean camps amazing. And as a kid, it was, at least for me like a huge amount of support and really helped me accept type one and embrace type one and use that to my advantage rather than it being something that hinders me. And then I was lucky enough to be so passionate about camp that I immediately went into being a camp counselor for the whole summer. And so I kind of just fell back into that support, because I was working in it. But there's so many kids who, you know, turn 18, they can't be campers anymore, they maybe don't, like have that passion or have the availability to work a camp all summer. And now they're just set free on their own. And I just think that there's such an opportunity there for camp to continue, whether it's an adult camp, which I know some people do host, but just to kind of extend that support, because as a kid, you're there's so much that stays the same, right, like from elementary school to high school so much that changes also, but your biggest changes are right after high school. So I think just finding ways to apply the magic or the science, if you will of camp to that next step.
Scott Benner 36:31
Yeah. So, so a way for young adults to be connected to each other, even if they can't go show up in the woods together for eight weeks. Right? Right. Yeah. Especially when they're now trying to figure out management stuff. That's not going to be completely obvious to them at first. Right, right. You need other people to speak to. Yeah, yeah. That's, I just think that's the key to this whole thing. Yeah, that not everybody is going to have all the ideas that they need, or, you know, they'll miss one little piece, and how great is it to be able to blurt it out. And I'll tell you what I believe, as the podcast grows, numbers are important. So it's not necessarily that everyone speaks, it's it's necessarily that everyone can see it. Because because if you take, if you take 50 people and ask a question, you might not get the answer. If you ask 50,000 people, you're gonna have somebody with some lived experience. Yeah. And their odds go way up, it really makes things easier. Because then people chime in, I think people are your fault a little bit by social media. There's, there's this idea that everybody that you see talking is everybody that's there, right. But I know like the rule of 10s exists in a big way, you reach 100,000 people to find 10,000 people to do something of those 10,000 people, only 1000 of them will take the next step of those 1000 Only 100 It really is true. Most people lurk, they stand back and they watch. And so, but when you hit in their sweet spot, they just jump. There's a person, they'll probably hear this, that I don't think I've ever heard from before. And then the other day, I asked about buying a more comfortable chair to record the podcast in and he was just like, so excited. He's like, I finally have something to contribute here. I know about this. And like, here they are, you know? Yeah. And meanwhile, no one else answered. Really. Right. And it was like it was I found the one person is like, I have real solid thoughts on this. And here's some links. And here are my thoughts. And this is what I think you should be looking at. And I think that works for everything. You know, here's my graph. What does it look like to you? Well, to one person, it looks like too much Basal to another person, it looks like you're not doing well with your meals. And then you have a conversation, you find a vector of attack. And three days later, the person comes back because Oh, I did it. It's all done. Yeah, like three days to go from a graph. That is horrifying to I did it. And yeah, meanwhile, people are going off to doctors for 612 18 months just to get their Basal rates from point three to point six. Right. Yeah. And, and, and that's demoralizing. That wasted time in there. I find really frustrating. So connections to people are really important.
Kelsey Duman 39:29
Yeah. And I think to your point, on the flip side a little bit, you know, there's so many people on social media or wherever giving advice or talking about their story. And I think there's a danger of feeling like, Well, what do I have to offer? Because there's so many people once you get plugged into those resources, there's so many people who have something to say, and it can maybe feel like, well, what am I going to say that's going to be any different or make any sort of impact but somewhere out there is someone that needs needs to hear what kind of chair to buy. And no one else is talking about that. And something even if it's just a little snippet that you say, can completely change their mindset?
Scott Benner 40:08
Well, you know, it can help with there being too many voices is and I tripped on this by mistake, but I think the podcast curated the Facebook group. So there are people who had already been through, you know, hundreds of hours of the podcast, and they were now far enough along the path to know what they didn't know. And that stops the extraneous people from coming in and saying something is really not very valuable are completely formed. And so people know, there's enough people here who do know, I don't need to give my my half baked answer here. Because I don't really know. Because you know, when you don't really have all the answers, you're like, Well, what I'm seeing is this when someone can come in and just like break it down for you. Right? It's there's, I don't think it's something you can't build it on purpose. But you can build it with intent, like you can start with something small with the right intent, don't lose track of the good intent. For me, it's super simple, like everything I do. I try to help people. But that's it. I only have one goal, like, is this going to help somebody? If it's not, it's not worth time? Yeah. And then the things that people find valuable. They kind of, you know, they they come towards, and then that grows it. And then the growth creates the whole thing, but you're limited when you do it. In the real world. You're limited by bunk space, or money or something like that. Where's the thing I build is free, basically. Yeah. For them. And for me, I mean, I don't put any great, great finances into it. Right. But But, but but it does then lack the human interaction. Right. Right. So Right. So if you had a wish, what would you wish for camp that it didn't have limits as far as people are? But would you? Oh, absolutely.
Kelsey Duman 42:00
I mean, I think the camping industry as a whole is sometimes viewed as whether it's diabetes camp, or not just viewed as unaccessible. For some people, whether that's because of finances or traveling, or you know, if there's a camp that's close to them. In and that's, I think, sometimes a tough pill for me to swallow, because I'm like, I want everyone at camp, everybody needs this. And I think just continuing I mean, diabetes camps have great resources. As far as scholarships, I'm pretty sure all the diabetes camps I know of have a baseline rule of we will never deny anyone based on finances, like we'll find a way. And a lot of camps have, you know, Lions Club members that'll drive kids to camp if their families don't have cars. So there's ways to do it. But I just don't think that it's always viewed that way. And so kind of changing that narrative and meeting the expectation as well. Of campus for everyone, like everybody belongs at camp, and it should be available to everyone. And everyone should feel like it's a safe space, a open space. And somewhere that they truly feel like they belong. And I think just like anything in our world today, like the camping industry has a ways to go with that. But kind of like you said, with the right intent, and then meeting the actions that are actually going to meet those expectations. I don't think it's an unreasonable ask by any means. Yeah.
Scott Benner 43:43
That's cool. I do you think this is an industry you're gonna stay in? Huh?
Kelsey Duman 43:48
Yeah, absolutely. I kind of a weird, a weird, not weird experience, but a meaningful experience when I was like, 16 I just kind of had this moment of like, what do I want to do with my life and I just ever since then, I keep coming back to camp. And I'm, you know, in my master's program right now for nonprofit management. And people are like, Oh, I'm going to work for Make a wish or I'm going to work for you know, these big nonprofit organizations. And I just keep coming back to camp and I'm learning great tools to help me in that but it this is definitely the industry that I feel called to serve in. So
Scott Benner 44:30
So I I've never said I've definitely never said this out loud. It's getting to the point where there's so many episodes I'm like, I really don't think I've ever said this, but my first foray into being helpful to people never got out of the planning stages. But okay, I did like I applied to be a charity. I guess I've got one c three or something like that. Right. And yeah, my idea was to set it seems ridiculous. Now I'm saying it out loud. Just because it seems odd. attainable without somebody without an influx of money. But I wanted to start a place where newly diagnosed or lost people could come and live with their families and be brought up to speed very quickly. Oh, that's awesome. Right? That was my that was my idea. I obviously do it now, online like this, right, like through radio. But that was my first idea is that there would be a structure somewhere that you could come and live at. And then And then because you'd be getting up in the morning and eating breakfast and going outside and being active or sitting down and doing school or whatever you'd be doing, you'd be living at that place for a short amount of time, in a way that you could end up having as many real life experiences around diabetes and insulin as possible, where someone would be with you the whole time to say, Okay, do this, do that do this because I see it. Now. If I followed, you're not that you would need that. I'm just saying you. But if I followed your CGM, and you and I were in close texting contact, like for two or three days, and you were having an issue, I'm confident we can clear the issue. Right, right. And so I thought if people were like together, and what is it, they really get from that? Whether you're in that texting situation, or you're together, it's a sounding board from a person who very likely does know the right thing to do in this situation. And so that that weeds out all of the, the extraneous noise in your head, like, Well, maybe it's this or maybe I should be doing that. Instead, it's just someone that goes, no, no, look right here. There's not enough insulin here. Right? You put it in, and then you watch the good thing happen. You learn really quickly. That was my that was my first idea. It is not easy to have a nonprofit I don't. There are so many things about it that scare me. And the one thing that really pushed me away from it was the Board of Directors, I got very scared of the idea of someone being over able to override my vision. And so that I dissolved that soon after that.
Kelsey Duman 47:06
Well, I mean, I think the idea is awesome. Like, honestly, the first thing I think of is it's like a Kickstarter camp, right? Like you get diagnosed, you go to Scotts camp for newly diagnosed, and you get kind of this simplified education. And now you're off to the races.
Scott Benner 47:25
In my mind, it's still doable online. Yeah, I do bring it up to a couple of people like, like, imagine someone like Jenny, who's at a desk. And instead of like, being with people, I don't know, imagine you could pop right onto a zoom, and say, Hey, this is it, then we're about the breakfast, blah, blah, blah, here it is. And she could actually look at it. And you can talk for a couple of seconds and work through it. Because still, like one of the, one of the restrictions of her job, or and I've, you know, where I've helped people were one of the restrictions is that sometimes people don't know, everything they should be telling you. So they leave out this one really like salient detail. And you're like, I don't understand why this didn't work out. And three days later, though, mentioned that, you know, they had oatmeal, you're like, oh, geez, you just said carbs. You didn't say it was oatmeal. You know, like that kind of thing. The evilness of all right, but it's there, like in my maniacal part of my brain, like, I'm picturing myself in a room, like with an infinite number of monitors, able to, like bring people up to speed really quickly. But there's got to be a real way to do that. Like, there's got to be a way to take that cartoon idea and make it more of a reality. Yeah, if I ask you, cuz you're gonna have a mastery by then you'll have real thoughts.
Kelsey Duman 48:48
Pretty soon, December.
Scott Benner 48:50
Right? And I don't even think like it shouldn't. It should be. It should be through your health care system. Yes. Like you should, you should be diagnosed. And you should leave with like a voucher. Like I used to get my mom on Mother's Day when I couldn't afford a present. Right? And it should tell you that when you're ready, somebody is going to walk through every aspect of your day with you into and then and then, you know, for a certain amount of time, and if you're really stuck, then you get moved to a different person. Like don't be mean like maybe somebody who's I don't know, it's there. Trust me. It's there. But no, I yeah, I'm all in I love it. The model is definitely not some nice person. Well, meaning doctor sees you for 14 minutes and send you home. That's not how it should. Right. So
Kelsey Duman 49:39
well. And you had mentioned, you know, it should be part of healthcare, and I've had people tell me, like, Why doesn't my insurance cover my camp tuition? And it's like, oh, man, I wish it did right. Because there's so much value in those experiences at camp like I gave my first shot to myself at camp. It's like huge right and a seven year old with type one. It's like The reality though of working with insurance companies to get them to cover a camp tuition. I mean, I can barely get them to cover my Dexcom supplies. Like,
Scott Benner 50:09
I'm pretty certain that Arden I mean, I know our it'll be 17 in a couple of days. I'm fairly certain she's never given herself an injection. Oh, I use diabetes for third 15 years. Right? And I don't think he's ever even come up.
Kelsey Duman 50:26
Yeah, well, and I mean, that speaks to the, the change in, in how good technology is now to like, she's gotten to have diabetes, I guess in this world where it was only a dream. When I was first diagnosed. I remember the doctors told my parents when I was diagnosed, will there'll be a cure by the time she turns 18. I'm like, well, it's 11 years later and still waiting on that gear. But now you I mean, I show my parents like my T slim that's connected to my Dexcom and they're it's like mind blowing to them because they went from this massive insulin pump and injections to this tiny little sleek touchpad
Scott Benner 51:09
plus their their indigenous people to a tree community. They really have never seen stuff like exactly. I have probably given Arden 10,000 injections, right? Yeah, but she's never like challenge she's ever really ever hold held the syringe. I mean, I'm sure she has, but I can't remember it. Right. So
Kelsey Duman 51:29
I still remember, I and I must have been seven and a half. So it's crazy to me that I remember this moment. But I remember being in my parents house, and I was holding the poker to my meter, right? Because there was no Dexcom back then. And I was like you can do it. Kelsey, you can do it. Like in my little seven year old mine. I'm like, you can poke your own finger. And I like counted to 10 and I poked my own finger and I was so proud of myself and how I
Scott Benner 51:57
looked the first time I did it to myself. And I was in my 40s I was like this is gonna hurt. I know this is gonna hurt. Is this gonna hurt? I don't want this to hurt. People say it doesn't hurt. Oh, it's not bad. Yeah, yeah, that's it. Like it's sort of over. But very, I love the idea of like a little kid just being like, I can do it. I can do it.
Kelsey Duman 52:18
Yeah, hype yourself up. Yeah. What, um,
Scott Benner 52:22
this is an unfair question that you're gonna probably answer, you know, with a disclaimer, but why do you seem so normal? And like, did you have any? I don't, I don't know how I mean, it says, Do you have any impediments? And while I've now spoken to so many people who have diabetes, and people seem to fall in like these two specific buckets, like, really burdened by it, don't really seem to mind it. I don't, I don't. Yeah, you know what I mean? Like, what is that? For you?
Kelsey Duman 52:53
I mean, I obviously hear some disclaimer coming right out the chute. I've definitely had my ups and downs with diabetes. College was tough, right? Like, I remember having this moment where I was like, Oh, if my blood sugar doesn't ride to 50 all day, I feel so much better. And I do better in classes. And it's like that lightbulb moment of you're like, Well, that was pretty obvious. I should have figured that out. But you get distracted. And so yeah, I've definitely had my days just like anyone else where you're like, diabetes sucks. I don't want to do this anymore. But truly, and, and I'm coming right back to it. Like, I feel like camp was that game changer for me. Of an I owe a lot of that to my parents, because as soon as I got diagnosed, they sent me to camp. But that was I think I was privileged to learn early on that there were other people who had the same struggles as me that there, you know, were resources that I could turn to when it was tough. And I, I fell in love so much with that camp community that I almost became grateful to diabetes for giving me that, that support system. And I mean, gosh, I we didn't get to have our wedding in 2020 because of COVID. But when we were planning it, five out of my seven bridesmaids had type one and I met them all at camp. Our best man was a friend from camp. So I feel like I've gotten so much good out of having diabetes because of those camp connections. That it's it's kind of hard to resent it so much just because I have so much to be grateful for with it. And, you know, Camp also helped me capitalize on some of the skills that diabetes brings into your life and really identify like, Hey, I, you know, had to be responsible at a young age, but now I have that responsibility skill that I've had since I was seven you know, so kind I feel like I mean, camp was definitely the game changer. And it helped teach me that there are parts of diabetes that I can be grateful for
Scott Benner 55:08
right. Now I agree with you. I think that it's there's something about the struggle that's valuable. If the struggle doesn't kill you. Yeah, like that kind of pressure. And there are some people I think, who are, are built differently, wired differently. And that the same struggle that might enrich you could stop them. Yeah, yeah. And it's just it's fascinating to see that how random it appears.
Kelsey Duman 55:39
Yeah, well, and I think to your point, it almost feels like a bit of a duty, if you will to, because I, I fell into that camp of like, feeling okay, and really embracing this and using it to my advantage, it feels like I have a responsibility to work with people who don't feel that way. And see if I can help be that support system that whether it changes their mind or just supports them. Because it's, I mean, like you said, there's two different kinds of people. I feel like with type one, and you either embrace it, or you deal with it, and that doesn't always end up great. Yeah,
Scott Benner 56:20
I feel like that to Kelsey. If we were only 30 years closer together, and I had diabetes. I could have marriage. Worse, I can't live in a tree though. My hands. Oh, true. Have the thumb under the branches the right way? Way I'm sure you do from growing up in Oregon. Right, right. How did you meet your husband?
Kelsey Duman 56:41
So speaking of things I can be grateful to diabetes for? Yeah, so my husband has type one. We actually met at diabetes camp. Shocker. I know. We met in 2016. And he actually never went to diabetes camp as a kid. But he is a basketball coach. And obviously, Crystal, the basketball camp is a diabetes basketball camp. And he had been applying for quite a few years to come and work the camp. And there was just never an opening. And they needed a coach one year and he came to Camp. And of course, all of our camp friends caught wind that we were maybe interested in each other. And they set up a whole camp skit for the talent show of how we were going to start dating and Oh, man. Thanks, can your camp friends really get involved in your personal life? Oh, great. Yeah,
Scott Benner 57:36
I felt like you were about to say this one time at diabetes camp. Right. Okay, for years that he couldn't get the job. Were you with somebody at that time anyway? I'm trying to imagine imagine if he got the job sooner. But you were with somebody. So you didn't intersect? Well?
Kelsey Duman 57:52
Oh, yeah. No, the timing was just awesome. I mean, like he and I both had been dating other people until about two years prior to that. So we both kind of had our time to be single. And then by the time he came to camp, it was like, wow, I'm really glad that this worked out now. type of thing.
Scott Benner 58:12
How much did having diabetes for I don't know, if you can't really speak for him. I'm already in my head. Like, you're gonna be like, I can't speak for him. But. But how much does it mean for the two of you to have type one? Or doesn't it matter?
Kelsey Duman 58:31
So good question, man. Scott coming in with the hard hitters.
Scott Benner 58:34
Like if he got cured tomorrow, would you be like, I don't even like him as much now.
Kelsey Duman 58:42
No, I mean, it's interesting, because we both have had very different experiences with type one. I feel like we're both in that camp of like, accepting it and embracing it. But like, we both have very different management styles. I feel like now that we're married, we're kind of getting on more of the same page with that, but like it. I mean, I think it it definitely helps. But it's never been like a forefront of our relationship.
Scott Benner 59:10
You weren't looking for a guy with type want to get married? No, no. Okay. You just said something. I'm gonna pin you down on it. Now you both have different styles, who styles?
Kelsey Duman 59:23
Different parts of different like when I first met him, he might hate me for saying this, but he'll be fine. Don't worry.
Scott Benner 59:30
I'm gonna hate you one way or the other. So let's just get Yeah, exactly. When
Kelsey Duman 59:33
I first met him, he was like he was he didn't have a or no, he had a CGM, but it was the Medtronic one and it was old enough that he had to calibrate it three times a day. And he said he held out his finger and he was like, I poke on this side of my thumb in the morning and the top is lunch and the side is dinner. And then I move on the next day to my pointer finger and I was just looking at him like what are you talking about? But you but he's also a math teacher. Right? So he's got that like logical, very organized mind that I don't. And I joke with him I'm like, so do you change your Lancet everyday too, because this isn't gonna work if you do.
Scott Benner 1:00:18
Well, you know, a math teacher and a camp counselor, one day, you guys will amass 10s of dollars to in your savings account. Yeah, tell me about it. So there's something there too, right? Like that. That feeling of helping people? He must have that as well. If he's a teacher.
Kelsey Duman 1:00:39
Yeah, for sure. Teacher and he coaches football and basketball. So we definitely both have. I think that more than like, obviously, we both have diabetes, which is a huge thing to have in common. But I think even more than that, it was the you're here at Camp to help people just like I am. You love working with kids and your daily like, life just like I do. And it both just happened to be because of diabetes. Yeah, that we met.
Scott Benner 1:01:07
So it's very nice. It really is kind of lovely. And, and sweet. But you guys got married during COVID? What did that mean? For different bedrooms? Or how did you
Kelsey Duman 1:01:18
know so we our wedding was planned for May 23. And we had this like 250 person wedding at Camp it was going to be at camp because that's where we met. And we had it pretty much all planned. And then like three weeks before it, you know, COVID was like still around and we're like, well, crap, what do we do? So we had to just pivot the Word of 2020. And we actually did a 10 person wedding because that was the max people that you were allowed to have gathered at that point. And it was just our immediate families. My brother married us my his sister was there who was going to be one of my bridesmaids, and then our parents. And we did it at my parents house in the middle of the woods.
Scott Benner 1:02:11
nowhere else to go. Right. Exactly.
Kelsey Duman 1:02:15
Yeah. And so it was it was it was a wonderful wedding. We, you know, we it was still at that point in COVID. Where people didn't really know like, what to do how careful to be like we didn't have I mean, Derek and I had but like, yeah.
Scott Benner 1:02:34
But we didn't have Yeah, when you're on your wedding day, your dad. No.
Kelsey Duman 1:02:39
And my parents were like very concerned about it. As we're all of us. And with Derek and I both having type one we were like, you know, at that point, like no one knew what was going to make it worse or better or safer. Or this
Scott Benner 1:02:53
this sweet story turns into a weird headline seven days later. Right? Exactly.
Kelsey Duman 1:02:59
And we were so nervous at that point. Like, no, our parents are older and oh, gosh, it could uh, it was in that like those those few months where it was like, what's going on? What
Scott Benner 1:03:10
is COVID? When does? When does camp come back? When's the next time Chris is running the camp.
Kelsey Duman 1:03:15
So we're doing unfortunately, this year, we have to do virtual camp again. Oregon just lifted a bunch of restrictions. But being a diabetes camp, we need a lot of prep time and doctors to hire and nurses to hire and so we're doing virtual camp end of this month. And we're super excited. I will tell you I thought the kids would be like, nope, everything's opened up. Nevermind I don't want to do virtual camp. But I keep getting emails from parents about how excited they are. And we just shipped off 75 boxes of like fun swag and gifts for them. So we're doing that this year, and then next July will be knock on wood fingers crossed back on the courts in Virginia, Oregon. In the middle of the woods.
Scott Benner 1:04:04
We'll be rolling that's really cool. Although Yeah, I guess a virtual camp you can't like meet a girl and kiss her behind a cabin or something like that. That's got it that's got to be rampant. How old? Are these kids?
Kelsey Duman 1:04:15
They are 10 through 17 some of them maybe some of them maybe? Yeah, I keep a close eye
Scott Benner 1:04:20
that you know a lot of a lot of adults. I know some of their best stories start with when I was in camp. And yeah, boy and I don't mean best stories like they learned math. Oh, boy. Well, I guess that's um, that's all kind of part of it. Where do you fall on? I mean, I The answer is obvious here. But I'm asking you literally because I saw somebody post this and on Facebook this morning I saw a young 22 year old I think guy say that. He was always family oriented and then was diagnosed at Brown this age and now it's scared to have a family? And do you? Are you scared of a family?
Kelsey Duman 1:05:04
You know, I'm not, I wouldn't say my husband or I are. And I think part of that is we just are, that's something that both of us have always wanted, is to have kids. The other part of it is, and this might come off odd to some people, and maybe this is just how I justify it to myself. But I, I feel like and even having a husband, I always thought this, but having a husband with type one obviously increases the odds of our kids having type one. But I guess my philosophy is, well, if they have type one, at least they'll be in a family that gets it knows how to manage it, and has like the resources like if my kids get to go to diabetes camp someday, I know they're going to be fine. And so at least, God forbid they get type one, but at least we'll know the signs to catch it early. And we'll have all the tools to make it as good of an experience as possible. So
Scott Benner 1:06:02
no, I think that's the I think there are a number of different ways to think about it. And I don't find one to be any more or less viable than the other. And for a lot of people say what you just said, and I think it's a I think it's comforting to hear, honestly.
Kelsey Duman 1:06:17
Well, and I mean, as much as there's extra odds that they will get type one, I have a couple other friends who both parents have type one and their kids don't. Yeah, so it's kind of like, well, it could not happen.
Scott Benner 1:06:30
I just think that you're trying to control. I don't know, randomness is a weird decision to make, like, if you think I think if you think you'd be so overwhelmed. If your child had type one, no matter how that would overwhelm you with need to do something or guilt or whatever would be that would I also think it's possibly different for people who are having a different time, like managing, like, if you're if a reasonable time managing, it seems more manageable. Right. But, but if I also like I like it when people know their limitations, too, and they say, Yeah, this would overwhelm me, this isn't something I should do. Absolutely. But you know, for November. I'm talking out of order in the timeline, but there'll be an episode November of a from a woman who, you know, adopted children, they wanted children couldn't have children adopted children. And then one of the children ends up with type one diabetes, and the other one ends up with something else, just this right. Through this randomness, and no way. Yeah. So. So I mean, there's an example. Right? Like, you don't get to decide how it works out. Right, you know, so you're either in to make a family and you're in for whatever comes next. Or that's not for you. And I think either way, is reasonable, just I think knowing that is probably the ultimate truth is it to me to see how I'm so willing to just speak like healthy, like what I think is the exact right thing. To me, that's the ultimate truth. Like, you're not going to get a clean. Like, like go the whole time. There's nobody I know who doesn't have something going on. If it's not. If it's not health, then it's money. And if it's not money, then it's bad family situations, if it's not, and the real unlucky people get multiples of those things. Yeah. Yeah. I don't think there's anyone walking around who wakes up in the morning. It's like, Hmm, everything's perfect. Right? I'll just go about my perfect day and do my perfect things. And if people are expecting that out of parenthood, I mean, from my perspective, you're making a huge mistake. Right? Yeah. So are you gonna make the babies are you like, what's the play? Because I mean, you're not old Kelsey, but you know what I'm saying?
Kelsey Duman 1:08:51
Yeah, I mean,
Scott Benner 1:08:54
when you're 65 going like, right? Oh, golly.
Kelsey Duman 1:08:59
No, I mean, I definitely think the plan is to try naturally. And I mean, if for some reason that doesn't work, like you mentioned, the, the person who adopted I've always I met this family through camp one year that they had a daughter with type one. And then they had found or not found this girl, but like, someone had come to them and said, Here's this girl, and she also has type one. And we know you know how to manage it. And she needs a family. And they were like, cool. Let's have two kids with type one, like, come on in. And I just thought that was so cool. So that's something that I would definitely consider as well.
Scott Benner 1:09:35
There's somebody who's been on the show who I think does. Oh my God, the word just left my head. Where's the word? DMA Kelsey. Where's the word when you're a person? And then a kid comes and leaves you there for a little while? With the ID sir. Thank you. Wow, that was terrible. Um, yeah, this person has been honors postures kids with type one. Oh, that's so cool. difficult, but you know, I think rewarding and valuable. Listen, I'm adopted. If somebody, if somebody didn't give me up for adoption, when they thought they couldn't take care of me, you and I are not having this conversation right now. So, you know, people need to find whatever path works for them. But, you know, there's a lot of good things that can come from making a family. So yeah,
Kelsey Duman 1:10:21
that person, the the person you mentioned, that fosters do they have type one themselves? They do? See, I mean, how cool is that for those kids, right? Like, you come from foster care where you're probably not meeting many other people with type one. And now you get a safe home. And someone that gets it, right, like, that just takes so much burden off those kids.
Scott Benner 1:10:42
If I remember the, if I remember the example, right, it was difficult in the beginning, beginning but a really swift change for the kid, you know, so that's really cool. Alright, so go adopt a bunch of babies just make sure they can hang in a tree, you know? Yeah. And we're good. forage on the ground for nuts and mushrooms and things like that, that grow it? Yeah. Where do you really live? Is it like, a metropolis or something like that? Or?
Kelsey Duman 1:11:09
So I live in Albany, which is like an hour south of Portland
Scott Benner 1:11:14
feel like area? My name from New York isn't? Yeah, probably. But it was they were out of names.
Kelsey Duman 1:11:22
Yeah, exactly. There's had to start copying pasting. But I mean, it's, I mean, it's definitely green here. But I'm in like, a little suburb area.
Scott Benner 1:11:31
But you're high all the time. Blood sugar wise, maybe. Oh, my God. So there you go. That's what I know about Albany, weed and trees. And I, I might be wrong about all of it. Right. I so is there anything that we haven't talked about that you hoped that we would have? I really I find myself before you answer that question. You You have so many different interesting perspectives, that I jumped around a lot trying to dig into all of your areas of expertise. But I don't know if you did you know, you'd be good on the podcast.
Kelsey Duman 1:12:08
I mean, not really. I knew after I talked with you, when we we talked with Chris, I was like, He's, you're just really easy to talk to. And I love the questions that you ask. And so I was like, I'm sure he'll ask questions that I can dig deep for good answer.
Scott Benner 1:12:24
Does it make you feel uncomfortable or comfortable to know that as I sat in this chair, I was like, I don't know who I'm talking to today. And then I looked up and I was like, Kelsey, I think that's the Chris Dudley girl.
Kelsey Duman 1:12:36
No, that's awesome. Yeah, I mean, yeah. And I love I mean, I love that you can just jump on with anyone and have a conversation about this stuff that speaks to your expertise in the podcast realm,
Scott Benner 1:12:49
I find people so interesting. So I have so many questions that I don't get to ask. Like, if I asked all the questions, I was thinking, every episode would be three hours. Right? Like I yeah, I have so many questions about. I want to I want to ask you more probing questions about about camp like, what, um, what would you say to somebody who doesn't? Like camp? Like, it's not for everybody?
Kelsey Duman 1:13:32
I love that question.
Scott Benner 1:13:33
What are you gonna answer that question? For I'll preface it by telling you this for years after Arden was diagnosed for like, you know, there's a really popular diabetes camp and she was like, no, no, no, like, that's not Arden's vibe. It's not just diabetes. Like you couldn't you couldn't send Arden to lollipop camp. She'd be like, I'm not up for that, like, you know, so. I don't even know what it is something about being outdoors that much maybe she's particular about the people she hangs out with. Yeah. I don't know. But what what do you what do you say to people, when I'm assuming people show up at their door, the parents are like, super excited for camp and the kid gets out of the carny. Like the kid doesn't look very excited. Like, Oh, yeah.
Kelsey Duman 1:14:17
Oh, yeah. Uh, yeah. So I love this question, because those kids show up at camp and you can just tell they don't want to be there, whether they're like, bawling their eyes out, or they're just like, not talking to anyone. And I'm like, you're my guy, like, I'm gonna go talk to you. Um, but like you said, it's not for everyone. And that's okay. Right. Like, I think the biggest thing is for people to recognize is that not all camps are the same. So like riding on insulin, awesome. Ski and Snowboard camp. looks very different than gills creek where you are out in the woods and hanging out in cabins and going on hikes and doing arts and crafts. Similarly, like So the basketball camp completely different, right? You're playing basketball all day. So I know kids that hated other camps but love deadly camp because they love basketball. And it's their interest is there. And so I think the what I would say to those families or those kids is to not rule out all camps just because you're not interested in one. And to really look into what camp entails because there is kind of that connotation of oh, well, summer camp, you're going to be out in the middle of the woods, you're not going to have you know, running water or what have you. But it's so different for every other camp riding on insulin is at the ski lodge, it's usually just a day camp. But you still get those camp vibes of connecting and doing something that you're interested in or trying something new with people who understand diabetes. And I think, I mean, writing on insulin, I think you can get just as much out of it as you do from day overnight in a traditional summer camp. So I think that would be my first bit of advice for people who are like, ooh, camp. But my other bit of advice would be just to try it. Right. And that's tough for some kids. But I, I've seen so many kids that just do not want to be at camp, and then they leave on Friday crying because they don't want to leave. Yeah. So I think there's a lot of, if you can get your kid to just try it, then there's a lot of development. And the campers or the counselors, and the staff are so well trained. Like we know, there's kids coming in who don't want to be there, like we're ready for those guys. And gals. But, yeah, I just, I think it's worth trying it. And if you don't like it, you know, that's okay. There's other like the podcast or the diabetes online community, there's other ways of support and other ways of meeting people that you can connect with, that are just as powerful. But I think it's worth a shot. If you can give it a try.
Scott Benner 1:17:06
It's cool that you've got it thought through like that I because I know, personally from the podcast that you have this feeling that there's this thing, and you've already made it, and it exists and you've seen it do so much good things for so many good, so many good things for so many people. And then somebody says I don't have time to listen, or you're like, ah, like it's it crushes you at first, and then you realize it's just not going to be for everybody. Right? And you know, nothing ever. Right? It's difficult though, once you've put so much effort into something for someone to go camp ill. And you're like, wait, no, no, no, no, no, I'm getting I got married a guy, okay. Like, you know, and the same thing. You know, somebody will post a, a graph, they clearly don't understand a lot of what they're doing. Right? I'm like, I think if you listen to these three episodes that would clarify it. And sometimes every once in a while someone will respond. I don't have time for that. And I'm like, I don't know what you want me to do then like like, right, like I already gave the world thing. This is it? Yeah. You know, like, if you want to go use it if you don't want it. I don't know what to do for you. Like, right, like, I can't, I can't come to your house. Although, right. Those are times where you think like, I bet I could wish I could roll up to somebody's house and just like help. And then like, if I could just get an hour with them. Like maybe if we get the 10 million downloads, I'll give myself away that can't be leaked. We'll do a raffle. Yeah, I actually tried to do that once for one of the sponsors. Oh, and I and the legal aspect of it did not like the idea. So Gotcha. Interesting. Yeah, it didn't work out. But I had that idea. I'll tell you off that I have so many, like, thoughts that I don't get to share on here. But if you can, can you hold on for a second? After we say goodbye? I'd like to ask you. Yeah, absolutely. Do you think people are pissed right now that they're not going to hear what the next question? Yeah, they're like, Wait a second. Guess what, everybody? Yeah. All right. Well, thank you very much for doing this. I really appreciate you taking the time.
Kelsey Duman 1:19:12
Yeah. Thanks so much for having me, of course.
Scott Benner 1:19:20
A huge thank you to one of today's sponsors, G voc glucagon. Find out more about Chivo Kibo pen at G Vogue glucagon.com Ford slash juicebox you spell that GVOKEGL You see ag o n.com. Forward slash juicebox. If you've enjoyed this podcast or any of the other ones, and you'd like to say thank you, it's super easy to do that. You can just go to T one D exchange.org. Forward slash juice box and fill out the survey.
Alright guys, there's not gonna be the high jinks at the end here. I'm completely beat. I just got done interviewing JC Petrovac and Trang Lai, from Omni pod. They announced the FDA clearance of the Omni pod five right on the Juicebox Podcast. And I'm beat from that still was very exciting. Oh, it's in Episode 621. Right before this if you're interested, because yeah, I mean, that thing. Everybody's been waiting for the on the pod five. The FDA just said go. So here we go. There are tons of details in that episode, go check it out. I'm super excited for Arden to try on the pod five. I am quite certain many of you are as well. Actually, I have a link Omni pod.com forward slash juice box five, if you want to get on the list. If the interests list, they're keeping a list of people who are interested because there's going to be a limited market release for the next. I don't know how long. They didn't say exactly. But it's again in the episode. I'm getting away from myself here. Anyway, if you want to let the good people at on the pod know you're interested in the Omni pod five, their new algorithm based insulin pump. Go to Omni pod.com forward slash juice box five. It's just the number five usually you guys go to alibaba.com forward slash juice box. Right now if you want to ask about that. It's juice box five. Honestly, I think my other Link gets there too. I'll look real quick. Like I said there wasn't going to be hygienic sit down on the pod.com. Forward slash juicebox. No five. scrolling, scrolling, go to page two have to scroll. No, that's not it. Huh, interesting. Get started. No. I guess you need the five. For now. I'm going to talk to somebody get it all put on one page for you. For now. On the pod.com juicebox five, go get on the list. Tell them like I'm interested. The interested list. I'm sure there's another name for it. But that escapes me right now. Anyway. Let me button this up. Thanks so much for listening. I'll be back soon with another episode of The Juicebox Podcast. I did it. We're done. I gotta I gotta go to bed.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#620 Exclusive Omnipod 5 Interview
Omnipod 5 receives FDA clearance!
Shacey Petrovic, President/CEO and Dr. Trang Ly, SVP and Medical Director spend an hour talking about the FDA approval of Omnipod 5. Tune in to learn about the approval, how the automated system works and so much more. This is an exclusive conversation that will only be heard on the Juicebox Podcast.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 620 of the Juicebox Podcast.
It isn't often that I bring you a podcast episode that was recorded on the same day that you're hearing it. But today is a special special event. It is Friday, January 28. And this morning at 6am insolate, makers of the Omni pod dash announced that their automated insulin delivery system Omni pod five has received clearance from the FDA. If you're like me, you've been waiting for Omni pod five for quite some time. And this is a very, very happy day for you. I can't wait for my daughter to try it. And I know you might feel the same. So I thought you might want to hear directly from JC Petrovac, President and CEO of insolate. Joining JC and I today is Dr. Trang Lai, Senior Vice President and medical director at insolate. We're going to talk all about on the pod five get as many of the listener questions that I compiled in in this hour as we can I lose AAC after an hour, but trying hangs on for another 25 minutes to talk about insulin pumping with the Omnipod five. Please remember while you're listening that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise. I want you to be able to listen straight through so no ads today, but please do remember to support the advertisers of the Juicebox Podcast. If you're interested in getting a Dexcom use my link. If you want a great blood glucose meter, check out the Contour Next One at my link. If you want to get an omni pod, please use my link. If you're going to take the T one D exchange survey and please do it's super simple to do and it supports the podcast. Use my link Are you looking for glucagon try the G vo hype open at my link. And don't forget about touched by type one my favorite diabetes organization dexcom.com forward slash juice box on the pod.com forward slash juice box contour next one.com forward slash juice box Chivo glucagon.com forward slash juice box T one D exchange.org. Forward slash juice box and touched by type one.org. There are links in the show notes of your podcast player and links at juicebox podcast.com. To these and all of the sponsors. When you use the links you're supporting the show. Last thing before we get started with chasing and trying if you're looking for a great community online, my Facebook group Juicebox Podcast type one diabetes is a private group with over 20,000 members just like you it's a great place to chat, learn or just watch what people do Juicebox Podcast type one diabetes. At the end of the episode I'm going to give you a link special for Juicebox Podcast listeners where you can go learn more about the Omni pod five. This episode is the only place where you'll be able to get this link today. If this is your first episode of the Juicebox Podcast and you're enjoying it, there's so much more that you might love. Subscribe now in the audio app that you're listening in. And if you're listening online, get yourself an audio app and find the Juicebox Podcast Subscribe and follow today for more great content like this.
Shacey Petrovic 3:24
Scott, great to be with you. I'm JC Petrovac, the President and CEO of insolate.
Dr. Trang Ly 3:28
Hi, Scott. I'm trying Lai as senior vice president medical director at insolate.
Scott Benner 3:35
The person to me that wants to make the most of the hour wants to just jump in and start asking questions. But I think it would be wrong just not to ask you like what this feels like. Because I know the process has been long. And it was made more difficult by COVID. And I just wonder how you're feeling this morning.
Shacey Petrovic 3:51
I could not be more excited. And I know I can speak on behalf of trainers. She is also incredibly excited. You know, excited. This has been you know, the better part of a decade in the making and 1000s of people have been involved across the company across the diabetes community. And you know, many, many technical challenges hurdles it just was it was not a straight road. And so to tackle all of those challenges, be here really pushing the field forward with an incredibly novel technology that brings a lot of firsts to market and that we know has the potential to dramatically improve the lives of people living with type one diabetes. I mean it is for me, it's it is it is very much the proudest moment in my career. And so I'm really really thrilled.
Scott Benner 4:42
That's amazing. It really is trying do you have any feelings on the process?
Dr. Trang Ly 4:48
Yeah, I'm super excited and it's been a long time in the making, but I cannot wait to get this product out to patients.
Scott Benner 4:56
Excellent. Well, I can't either I'm gonna say from you know, the But I don't know if there are many people that speak to as many people with diabetes as I do. And I just think that what it's going to accomplish for just the general public of people who use insulin in general, it's going to be, it's going to be, I mean, life changing, seems trite to say, but I do think that's right, I watched an algorithm work in my house, I can't wait to try this one. And I know what it's going to do for people who struggle and who feel more of a, I mean, not just the health impact, I guess, but a psychological impact of having diabetes that sort of all over the place all the time and not having to think about that my daughter is getting ready to leave for college, you know, and so are a lot of other people's sons and daughters. So it's a really exciting time. All right, so I guess, I'll give you my understanding, you'll make sure I have it right. You know, there are, you know, algorithms you have won. And I want to know how it works. So I, I just I want to know, nuts and bolts how it goes. So I'm looking for just maybe a high level overview of what the system does, and then we can pick through it a little more.
Shacey Petrovic 6:08
Sure. Yeah. Well, I mean, I think, you know, we probably don't need to start at the high level, you and your, your listeners know better than anybody, just how hard diabetes is and how much work it takes to manage. So Omnipod five, and the smart adjust technology, which is the algorithm are really designed to be an incredibly easy to use system that reduces the amount of work that a person has to put in to manage their diabetes. The system itself is, consists of the same kind of small, wearable, waterproof pod, but there's been a lot of really exciting technology packed into that pod. And one of the big technical challenges of the program actually was getting the smart adjust technology onto the pod. You know, it's it's a very sophisticated algorithm, lots of processing power, and the team worked very hard to get that technology onto the pod. So that smarter just technology automatically, the pod connects automatically, with the Dexcom G SIX sensor, it takes a reading every five minutes, and it adjusts insulin every five minutes. The algorithm predicts where your blood glucose is going to be an hour from now, and then adjusts insulin in five minute increments to prevent against highs and lows both during the day and overnight. So you know, one of maybe try and can speak a bit to the uniqueness of the algorithm relative to others that you may have had experience with Scott. But what I can say as the clinical data was extraordinary, and demonstrates really improved glycemic control, improved time and range, lower agency and minimal hypoglycemia. So kind of the trifecta of the clinical results we're looking for for people with diabetes. Well,
Scott Benner 7:57
that must be true, because no fewer than three people in my Facebook group said I'm in this trial, they better not take it from me now that it came to market. So people seem excited and happy with it, for sure. You have a trend? What are your thoughts on on how it works?
Dr. Trang Ly 8:13
Yeah, I think she covered it. At a high level, I think, you know, very similar to what we expect from AIG systems. Now, the algorithm adjusts insulin dynamically every five minutes so that people don't have to make these decisions. And, you know, Scott, just how much better glucose control you get when you're adjusting and had that feedback loop from the CGM. So I think, you know, one of the unique features of our system is the customizable glucose targets that you can set at different times of day. And that really allows flexibility for people who might want to run a little higher at certain times, like maybe when you're going for a sleepover or night, or you know, you might be new to AD and be hyperglycemia unaware, and you might want to run out a higher setpoint. So that it does give that optionality. And yeah, it's a great algorithm, our clinical data proof site,
Scott Benner 9:12
well, I already pitched my marketing idea to you, I think you should give away a coupon for a new mattress and pillow because people are gonna finally get to sleep and they're gonna want to become they don't even know their beds are uncomfortable. They're gonna find out pretty soon.
Shacey Petrovic 9:25
Scott, by the way, we heard that time and time again, from clinical trial participants, you know, not just from people on the system, but from their families, their parents, and so I remember what six years ago when you and I first spoke, you said that that was the most important gift that we could give to you, you know, in terms of your health and your reduction of stress is just a night's sleep. So we're really excited to bring that to people with diabetes.
Scott Benner 9:53
I feel like I I have to tell you the I've sort of been on the inside of this for a little while. I don't know how you guys Take the stress of all this. I'm nervous right now, I have no stake in this whatsoever. And I'm feel like I can't believe this happen. Alright, so So okay, so somebody's going to get on the pod five, right? And they're going to get a selection of pods that will last them a certain amount of time, I'm assuming you're going to offer them a PDM as well. Right? Yes. Okay. Yes. Is that going to look like the dash PDM.
Shacey Petrovic 10:27
I'll let try and talk a little bit about the handheld controller. But every, every new user will receive a handheld controller, along with the system, we're really excited to offer Omni pod five through the pharmacy. And what that enables us to do similar to what we do with Omnipod dash today is allow people to use the system without a long term commitment. And without an upfront cost, like we see with other systems. And so we will provide this handheld controller free of charge. And, and you know, today actually, in the pharmacy Omnipod dash users can try the system for free for 30 days. And this promise that we have and offering the technology through the pharmacy means that people can upgrade without an upgrade fee, or without waiting out there, lock in periods. So that's the benefit of, of kind of getting on dash in the pharmacy. And that's our commitment, you know, in terms of the technology that we bring to the community is that we want to do that in the most cost effective way. Without and in the most consumer friendly way, you know, without making people wait out their contracts or pay large upfront costs.
Scott Benner 11:41
Let me kind of go a little farther on that then. So my two questions are, will they will it not be covered as a durable medical product?
Shacey Petrovic 11:50
It's right, it will be offered through the pharmacy. So not through DME the vast majority actually of our users today with Omni pod dash are going through the pharmacy. And the reason we like that channel is because it is a very predictable low out of pocket costs for our users. And it enables us to offer Omni pod dash today and Omni pod five shortly without that upfront cost and that long term lock in period that people experience in the Durable Medical Equipment channel.
Scott Benner 12:20
No, I'm hearing it. And I'm excited to say that you're also going to be able to run on the pod five from an Android phone. Is that right?
Shacey Petrovic 12:28
That's right. That's right. Yeah, we will launch with compatibility with a number of Android phones. And which means that they that you and your users will be able to download a secure app on their Android phone and can control the system without biocompatible phone without the need for the handheld device. But the experience with the handheld device is fantastic too. And I think maybe trying you can talk to some of that experience with the the handheld controller. Please,
Dr. Trang Ly 13:00
yeah, happy to. So Scott, you asked whether it was similar to dash, the user interface, and it it is it is built on the Omnipod dash platform. And so for our users who are familiar with Dash already, it's a very smooth and easy transition to Omnipod. Five. And in fact, if if you're already on Omnipod dash and A Dexcom G six, you can go through our onboarding, self service onboarding platform to be able to get yourself on to Omnipod. Five. So you know, we are really trying to innovate not just in the product, but the way we serve and train and assist our users in getting on to the technology. So the that was important to us that the user interface was not too different from Darshan. It's a very, very similar setup.
Scott Benner 13:53
Well, there. I have questions from from the audience. Well, I see the Dexcom information right. On the on the on the on the pipe screen.
Shacey Petrovic 14:03
Okay. Yes, you will. Front and center, actually. Excellent.
Scott Benner 14:08
Well, here's, here's a down deep question from somebody, will multiple profiles be available?
Dr. Trang Ly 14:15
And in terms of multiple Basal profiles, yeah. Is that what they mean? Are they
Scott Benner 14:20
Yes, yeah. Okay. So you'll be able to as by way of an example, my daughter can have a profile for different times of the month as an example. Yes, I just found myself being demure for reasons I don't understand. That's not usually how I am. Do different insulins yield different results? Because or does the algorithm adjust to it?
Dr. Trang Ly 14:47
Yeah, the Omnipod. Five was tested using humor log Novolog and admelog insolence and that's what they're cleared for. So we do not test them with other insolence. And so that's the indication. Gotcha.
Scott Benner 15:03
Okay. When I set the, I get the device and I'm super excited and I set it up, What settings do I have access to? Like, what do I have to tell it carb ratios, my Basal rate and, and then what happens from there.
Dr. Trang Ly 15:17
So the, when you set up dash, the exact same setups that you require settings that you would enter into dash, you would require those to be entered into Omnipod five. So that would include all the Basal settings, the insulin to carb ratio, as you mentioned, correction factor, the the key difference is the target glucose. So in Bolus calculators, you generally set up a target glucose so that the user can the Bolus calculator can help assist you in determining how much insulin your system is going to calculate for you for a Bolus. But what our system does is it also uses that information to drive the algorithm. So whatever customized target you choose, say you're choosing one 110, you know, all the time, 24 hours, then the algorithm is always going to be driving towards that target.
Scott Benner 16:15
Let me ask you this, if I tell it my Basal rates one unit an hour, and it realizes it's more like 110 or 1.1? Will it make that adjustment on its own in the way the algorithm works?
Dr. Trang Ly 16:26
That's right, that's what the system will do?
Scott Benner 16:29
Will it tell me that? Well, let's say, hey, chucklehead, I know you think your your Basal is one, but it's 1.1? Is there a little pop up? Or how do I know that that's happening?
Dr. Trang Ly 16:37
No. So it actually just takes care of it for you, you know, one of the philosophically what one of our really, you know, in Yeah, design principles and with Omni pod is really to simplify the experience for our users. And that means not telling you every single time we adjust insulin, if it's unnecessary, so we really want people to live their lives and, you know, not worry about their Basal rates. And we do ask them to Bolus for their meals. So it is a hybrid closed loop system where they are expected to interact with their device for boluses. But in between times, really, they just wearing their pod and their CGM. And the system takes care of them.
Scott Benner 17:29
How do I handle the transition that and if I put it on a prepubescent child, and suddenly they hit puberty, and their Basal rates go from point five to 1.2? Like I don't want the algorithm just keep doing do I want the algorithm to just keep doing it? Or do I have to go back in there and make a change ever?
Dr. Trang Ly 17:46
Yeah, it's a very important question for ARD systems. So we have an activity. And what that does is it adjust to the person's actual insulin use over time. And so if you do that, too quickly, you can, if you add activities too quick, you could deliver too much insulin, say you run into a couple of days where you have in, you know, infusion issues, or you know, your pod falls off, and you're actually delivering a lot of insulin, but, you know, it may it may not be your body may not be as sensitive, and then a couple of days later, you need less insulin, you don't want to a system that is adapting too quickly. And so we think our activity is just right, because, you know, it's worked really well in our clinical trials, and it will adapt over time for a growing child, you know, a teenager going through puberty, all of that. So, you know, that's why you test these systems over a long period of time, to see how well it works. And, and, you know, what, it's important to me when I look at all the different systems is not just how they work in the beginning, but how how they work over a period of time. And, you know, we've got Todman data now to show that the systems have really durable clinical benefit.
Scott Benner 19:03
Can I leave the algorithm and use the pod like a regular insulin pump? If i Yes,
Dr. Trang Ly 19:09
yes, yeah, it will, you can use it in in a very similar fashion to Omnipod dash. So if you didn't have a CGM, it will function just like dash and then with CGM, you will have the ability to switch into automated mode. Okay.
Shacey Petrovic 19:28
And train highlights a really important point, you know, we designed the system with sort of the rallying cry of simplicity. So, you know, toggling in and out of closed loop and open loop, it's just the touch of a button, you know, and we did try to provide just the information that people really want and not the information that most people really just don't need on a very regular basis. I think when we think about these systems and the ability to bring the the, you know, improved outcomes that Omnipod five can can really deliver for people with diabetes, you know, one of the hurdles to more people adopting Omni pod. And AAD has been the complexity and the cost. And so you know, when we set out on this mission, when he said, We've got to solve for the access issues, and we believe pharmacy offers a much better, much easier, much more kind of cost effective opportunity for the customer. And then we've got to make the system as simple to use as possible for multiple daily injection users, for kids for, you know, older people for the masses, essentially. And I think the team has done just a remarkable job taking what is incredibly sophisticated, you know, technology, elegant technology, but making it really, really simple for users.
Scott Benner 20:50
So I think it's important as well, one of the biggest issues that I've seen with other looping systems so far is that the, the, the things you need to know to use them sometimes are a barrier to using them. So it's not easy to just, you know, you start turning the wrong dial the wrong way. And and suddenly, things are upside down. So I think that's absolutely fantastic. I have a couple other questions. And then I'm gonna jump onto another. Another topic, minimum fill is 85 units. That's right,
Shacey Petrovic 21:19
same pod, just a lot more technology. And
Scott Benner 21:23
are there modes? Like, is there a deep sleep mode exercise mode? Or is it just how does that work?
Dr. Trang Ly 21:30
Yeah, so it has an activity feature. And during when you activate this feature, what happens is their target glucose goes to 150. And also our algorithm delivers less insulin as well. So that's our feature for reduced algorithm, insulin delivery,
Scott Benner 21:51
is there an increase? Setting, there isn't like a Thanksgiving setting or something like that.
Shacey Petrovic 21:59
You can target a higher setpoint for Thanksgiving, which is a great idea.
Scott Benner 22:04
So sort of bare bones like simple works, does it learn? Yes. Okay. It absolutely does. Yes. And but it learns over, like a short shelf life, like my like, point is that if I start wearing Omnipod, I keep saying I don't have diabetes, if someone starts if someone starts wearing Omnipod, five, let's say three months from now. And you know, they wear it for five years, is it like a supercomputer five years from now? Or is it just sort of like learning in the, in the now like, it learns from the past pod and applies what it knows from the past pod to the current pod? Yeah,
Dr. Trang Ly 22:39
it learns from the last several pods, in fact, Scott, and it updates accordingly, depending on how much the device is actually delivered insulin, rather than based off of Basal rate settings. So you know, what was important for us was, we don't want you or your daughter wouldn't be constantly having to tweak the algorithm in order to get optimal glucose control, it was important that we reduce the burden for people and families by growing with the user and augmenting that insulin delivery over time based on the information that we have. And so there is an activity. And probably the most dark example of that was actually, during one of our studies, which involved actually adults with type two, where we saw very quite large increase. So you know, these were people who had sub optimal glucose control when they came in, and the doctor put them on, you know, roughly 30 units a day, actually, it was 27 units, in fact, and then, over a couple of weeks, we actually, you know, the system because of persistent hyperglycemia, ramped that up to about 60 units over time. So it does have that ability to detect that persistent hyperglycemia react to that, and then kind of reset that baseline of required insulin delivery.
Scott Benner 24:11
It's interesting that you use that as an example because the other day in my group, a gentleman with type two, told me that he had found the podcast got himself an omni pod. Since then, his a one C is incredibly lower his time and range is crazy. He's lost, like 70 pounds, you know, and I didn't even make the podcast for people with type two diabetes when I wasn't till years later when I thought, I think this is as valuable for anyone using insulin. So I can't wait for it to help. Like there's such a such JC tell me for a second about seeing all the benefit in front of view. And, I mean, I know you're your next leap. I have the same leap to I have a completely different business than you but I have this thing. I know it's valuable. And how do I tell you about it? How do I get you to listen do an episode right? Like, is that nerve racking? Are you excited about that, because this is,
Shacey Petrovic 25:05
I am really, really excited, you know, there's there, we know that there is tremendous enthusiasm in the marketplace for this technology. We've already had, you know, 1000s of clinicians participate in webinars and sign up for education around it, I get outreach multiple times a day from people in the community that want access to the technology. So we're in a strong kind of strong foundation right now from which to really build awareness around the benefits of the technology. And our job now is to, you know, move into limited market release. And that will enable us to ensure that we test all of our systems, our processes, our trainings, to prepare for what we know is going to be tremendous demand for the technology. And once we've done that, we will really start to ramp up awareness and education in the community around Omnipod. Five and its benefits, you know, but you know, I stand here on the cusp of all of that, and I, I just am looking to the next several years, and we've got, we've probably got a decade in front of us, of improving outcomes for people with diabetes, first, for people living with type one diabetes, which is what this system will be indicated for ages six to 70, we will follow on that with what we call our preschool indication, down to age two. So we will be expanding our benefit for people living with type one down to really young, young people. And then we will, you know, we have work underway evaluating the algorithm in the type to user. So to your point, we're going to follow with multiple phone platforms, multiple centers, more and more patients who can benefit from this technology. So we're at the cusp of years of impact, but this this moment, we're we're about to bring this technology to, you know, the vast majority of people living with type one diabetes. You know, like I said, it's the better part of a decade in the making. And it's our job now to take the incredible technical and clinical work that training and our technology teams did, and, and help educate people on how this can change their lives. And, you know, forever, we've been changing lives really by, you know, improving the user experience, and to now take that and be able to add the incredible improved outcomes that we saw with Omnipod. Five, it's just, you know, it is very, very exciting. There's some anxiety because we know that demand, I'll tell you what the anxiety is there, because we know demand is there. And because we have moved to a business model where we don't have any constraints, you know, we're not making our customers wait four years for the next technology. And we're not charging upgrade fees. So technically, anybody who wants this technology can get it as soon as they have access to it. And that's the anxiety inducing thing. Are we prepared for that? But I know we're prepared for
Scott Benner 28:00
that. If you went one more word of that sentence, I would have launched into my Omni pod promise that that I know by heart. How long do you expect the LMR to be?
Shacey Petrovic 28:11
Well, we, we haven't really defined it because we do have to take the latitude to learn, you know, the whole purpose of a limited market release, which is not an FDA requirement. It's just a best practice in industry. But the whole purpose of this is to ensure that we are ready for larger demand. So for example, trying reference that the the easiest and fastest way to get on to Omnipod. Five is to be an Omnipod dash user with a Dexcom six user Dexcom six experience, because what that means is you will be able to essentially train via online tools and not have to meet with any sort of clinician or support. So that's one training pathway. But we know that plenty of people who today use multiple daily injections will be interested in the technology. We know that Omnipod users without Dexcom, GS six experience will be interested. And we know that people using traditional tube pump therapies will be interested. Each of those are different training pathways, and we have to test those and make sure that everything is in order.
Scott Benner 29:13
So I'm gonna ask an incredibly unfair and difficult question because you're literally this is the morning I don't know if people realize this or not. But you guys announced this like three and a half hours ago. And we're
Shacey Petrovic 29:23
Yes, you have impeccable timing set.
Scott Benner 29:26
I said, I said to somebody this morning, I was like, how did we randomly pick Friday and it worked out like oh my god for like a week, we kept saying like, are we gonna have to record this and it didn't happen, and we pretend it happened, and I'll put it out later. That'll seem weird. So this is an incredibly it's an unfair question, but it's a technology question that happens all the time. I'm not asking you what's next. But I'm hearing questions in my own head as you're talking. And I'm hoping that you're doing that stuff behind the scenes, for instance, integrating with G seven and like, my heart is like, I hope there are people in a room working on that. Lowering the target glucose, like, in my heart, I hope that you're like going to take a big deep breath, go on vacation and then be like, alright, FDA, we're doing it again. You know, like, I don't know, but but I think people will, you know, you're making a great point, like, I want to preface it by saying, if you're on MDI, right now, if you're using a pump that doesn't do this, no brainer, right? Like, it's an absolutely a no brainer. But I sit here in front of you, my daughter has a one, C has been between five, two and six, two for eight years. And we know how to do that, like so. But we do that with the do it yourself, algorithm. And before that, we did it manually. I can do it with an algorithm, I can do it without an algorithm, but my daughter's leaving for college and in my heart, here's what I think I look at the two of you. And here's what I see. I see the ladies that brought me algorithm on the pump, no link between a controller and a phone, and the pump. And my daughter doesn't have to be an app developer to use her, because I'm pretty sure if I sent my daughter to school with a laptop, and I was like, Okay, now listen, if something goes wrong with the loop, here's what we're gonna do. Because she'll be like, I'm not doing that then I was like, okay, so I love I love the system idea. Like, I cannot literally wait to get it like I would drive to Boston right now, if you told me I can have a box of it, you know what I mean? But and I think for the vast majority of people, that's exactly what it's going to be. But what do you do? If you're a five a one C, but you want the automation? Like, is there a way to live with that time?
Dr. Trang Ly 31:42
Yeah, I, you know, I think I hope that your family tries this, and really see the benefits of not having to worry about all the technical things of putting it together and, and give you the peace of mind that you've been after all this time. I, you know, in our clinical trial results for our adults and adolescents, down to age 14, a third of our patients had a time in range greater than 80%, which is really just quite remarkable. And for our kids, so the six to 14 group actually are two to six year olds as well. The mean, a one C was 6.9%. And but you know, what that means is that half the patients had an A one C with a six in front of it, which is just mind blowing, compared to, you know, where, where we are today in clinical practice? And so, yes, I definitely think that you know, that all the things that is driving good control with your daughter, it's likely, you know, to be attributed to things like diet, and exercise as well, not just the automated insulin delivery. And I think that she'll get really great results on our system.
Scott Benner 33:07
To be fair, and I want to be fair, part of the way we accomplish that is that we, with some frequency, leave the automated system and make adjustments to kind of stay ahead of things. So that's why I asked about that earlier. Look, seriously, I can't wait, I'm super excited.
Shacey Petrovic 33:23
And I think what we want for, you know, somebody like you and Arden is to be able to get that outcome with a lot less work. You know, I mean, that's, that is one of the major benefits of Omnipod. Five is just the reduction of burden all those hundreds of decisions and, you know, the constant interaction, that we can take some of that away from you so that you can get great outcomes without having to put in so much work.
Scott Benner 33:49
I can't wait, I'm genuinely. So G seven is probably going to, it's probably gonna pop fairly soon. And so I'm assuming you're working on that. Do you have thoughts about that, that you could share with people? Or no,
Shacey Petrovic 34:03
yes. So as I mentioned, you know, this is the start of what I think is going to be a really exciting several years of innovation. So we have shared publicly that we've got great partnerships, we have a wonderful partnership with Dexcom. They have an incredibly exciting pipeline. And we are hard at work integrating with their future technologies like g7. The same thing is true for Abbott, another great partner of ours, we're hard at work integrating with their sensor pipelines. And then of course, we've also mentioned publicly that we are hard at work integrating with future phone platforms like iOS. So all of that is underway. And the last thing I would say is we are hard at work also to bring this technology to people across the world. So we're starting with, you know, launch here in the United States. This clearance is a great milestone as we think about bringing the technology to other parts of the world, because it just is the final step in the clinical and regulatory hurdle and then we can start the work actually The work is already underway to really bring this technology to other markets outside the US.
Scott Benner 35:04
I've already gotten a message this morning from a person in Canada, a person in Sweden and a person in Australia. Please ask about us. So anyway, there it wasn't, you didn't have to ask also, you did me, I'm just gonna take my little whiteboard and erase where I wrote iPhone, question mark. Is there any kind of timeframe for iPhone that you have in mind, we have not
Shacey Petrovic 35:29
shared that publicly, what we have shared is the work has been underway for quite some time. So we our goal is to follow as quickly as we can. But you know, one thing we do is prioritize the user experience, which means we have to build a native app in both operating systems to ensure that we deliver the best possible user experience. So it is and the systems do work differently. You know, the operating systems work differently. So it is not a small technical undertaking. But that works been underway. We've got a very talented group of software developers and others working on that and and certainly understand that, you know, our customers want it and we're going to get it to them as quickly as we can.
Scott Benner 36:09
Excellent. A question about the sensors trying on day one, or with a failing sensor? How does the algorithm handle spotty information? Or how does the user handle it?
Dr. Trang Ly 36:21
Yeah, so I think the, the, the sensor issues that we used to see have definitely vastly improved. And I just really love the GC sensor every time I see the data coming in. And actually, you know, those sensor failures are definitely infrequent compared to what they used to be. So our algorithm has all the safety mitigations built in for loss of CGM signal. So it will actually use the prediction to deliver insulin for a certain period of time. But it actually depends on what the previous prediction is. So say, You were crushing low and you were predicted to be you know, 60 or less, and you were low, then the algorithm would actually suspend. And even if you didn't have the CGM come in, it would actually stay suspended for an hour. So there are a number of safety mitigations in place. And then when the CGM value comes back, it will actually just revert back and not like make you do stuff to put yourself back into automated mode. So you know that the whole user experience is really important to us. And, and you know, we're very lucky to be working with GSX, which is a really great sensor.
Scott Benner 37:36
That's well thought out. That's that's an excellent virtue of it for sure. Line of sight. So my, my satellite needs to see the Earth or my cell phone doesn't work, right. Does the CGM and the pod need to be in line of sight of each other? Or how does that
Dr. Trang Ly 37:51
work? Yeah, yeah, it does have to be within line of sight. And you know, I'm really proud of our engineering team. Scott, you know, when we first started the clinical study, I was a little bit nervous, I have to tell you about the connection between CGM and pod, because as you know, and can appreciate, it's all about how well those two devices talk to one another as to how good your glucose control is going to be. But you know, we have a fantastic antenna in our pod, the connection is remarkably good. Between the two in children and adults who were you know, CGM, obviously, for the 10 days, and then the pod button change every three days. So even with all of that, you know, every day use we have overall connectivity is
Scott Benner 38:42
excellent. Do you happen to see difference with people's body masses? Is there a change there?
Dr. Trang Ly 38:47
Yeah, there is. So it, so Bluetooth doesn't work well through body. But I have to say that because of the changes we've made to the antenna, the connectivity is excellent. It is one of the reasons why we have such good clinical trial results. Actually.
Scott Benner 39:08
Tracy, can I ask you what you've taken away from this process? I mean, about between making a product and the FDA like or do you have a notebook on the side of your desk that you're gonna that you were like, remember this next time? Or, I mean, honestly, Blizzard? Uh, I can't imagine it wasn't a learning experience. But like, was it valuable?
Shacey Petrovic 39:30
Yeah, it was incredibly valuable and incredibly valuable learning experience, I would say. I mean, I would never speak for the FDA, but I would guess it's a learning experience on both sides. Because this you know, we were designated as a breakthrough technology. This is brand new innovation that has never been delivered before. So phone control. This is the first time ever that somebody will be able to control their insulin delivery system, their Omni pod with a mobile a smartphone. You know, just the technology of getting the algorithm onto the pod, which, by the way, you know, when we started this venture seven years ago, the technology didn't exist yet, you know, the in train will tell you and the early clinical trials, people were walking around with backpacks of, you know, tablets, etc, it was a different system, but we knew the technology was in the pipeline of, you know, Chip companies, etc. And so we knew it was coming. And we had to take a bit of a leap of faith. And so, you know, it is really incredible to see the FDA lean in create pathways like breakthrough technology, like interoperability to help us bring new groundbreaking innovation to people living with diabetes. And for us, you know, incredibly learning experience, because nobody had done it before. We were taking advantage of new pathways, we were kind of working through what that needed to look like the FDA was extremely helpful in sharing their perspective on what needed to be in place, you know, clinically, and in terms of technical documentation and testing, to be able to feel confident that we could deliver this technology to the community. And so that's all, you know, that's plowing incredible amount of new ground. Yeah. And now, now we know what it takes. And so that's, that's a really exciting place to be in. You know, we've got certainly the battle scars to prove it in terms of the development process, the clinical process, but, you know, this has been building new muscles for our company. And frankly, you know, just bringing brand new technology that many people said, you know, even just a few years ago, couldn't be done to the community.
Scott Benner 41:43
Let me tell people listening, why that's more exciting than they think. So when you get a breakthrough designation, what that means is, the FDA does not see enough similarities between your product and any existing product. Because if they did, you could have piggybacked off of another company's filing look at me showing off what I know about the FDA. Hold on a second.
Shacey Petrovic 42:02
I think this is your wife, right? She's the regulatory affairs professional
Scott Benner 42:05
whispers in my ear. So I don't know anything. I just know how to make this podcast, honestly, and take out the garbage beyond that I'm kind of useless. So so. So here's why that seems exciting to me. It's because what you're telling me is you are bringing something to the world that does not exist yet. That's right. Yeah. If it did exist, and you were just putting it on the pod, we would have been using this thing. A year and a half ago, probably.
Shacey Petrovic 42:30
Right. Yeah, that's, that's right. This is brand new technology. And I think, you know, trying, obviously interacted with the FDA on a highly frequent basis. So she probably has additional insight to offer. But you know, what, what's exciting for me is that we are moving the field forward, you know, we we've known for years that people want to be able to control their Omni pod with their smartphone. And now we're finally here, having worked through all of the technical and regulatory hurdles to be able to bring that to people along with, you know, the algorithm and automated insulin delivery with Omni pod five. But this is no small feat. Nobody's done it before. We're the first and we're thrilled to be able to bring this to the community.
Scott Benner 43:12
I have more questions, but I'm going to ask trying a question in front of Chasey. Who's Chase, he's going to have to leave first. So I want Chang to be comfortable or trying to be comfortable whether or not she can answer this or not. Are we anywhere near the ceiling of what this algorithm is going to do?
Dr. Trang Ly 43:28
And there's no ceiling. Okay. I think, you know, I, I think you'll be pleased when you try it? Yeah,
Scott Benner 43:40
but am I going to wake up here, I'll tell you the fastest story. My daughter is 17. She'll be 18. This summer. We put her on an insulin pump when she was four, because we didn't want to send her to school using shots because I was like, What am I gonna let somebody I don't know, stick my kid with a pin every day. I was like, that doesn't sound right. So we went to our local children's hospital, they had an insulin pump there. And trying you'll love this story. There was a table in the middle of a conference room and it had all of the insulin pumps that were available. They were set out, like like I was buying jewelry, okay, there was everything but lights shining on them. Now, keeping in mind, this was 2007 or eight. And I'm walking around the room, I don't see anything that I particularly am excited about. In the far back corner of this conference from this like little cutout wedge, there's a little fold up table, and there's something on it. And I walk over to see what it is. And it looks like someone had an omni pod in their hand, got about 10 feet from the table decided they didn't want to walk any further pitched it into the wall and it landed on the table. Okay. So I pick it up and I take it over to the nurse practitioner and I go, Hey, what is this? And they're like, Oh, you don't want that. It doesn't have tubes. It won't work on your daughter. She's too thin. They said everything in the world to me about why I wouldn't want this thing. I took it over to my wife and I said this is a this is a contained device. And my wife's like, who cares? I'm like big cuz every time they change it, I started saying like, what are they going to do make 75 versions of this thing I was like, every time they upgraded, like, we're gonna move up with it. I was like, this looks mobile to me. I didn't know anything about you guys. I didn't know if even what I was saying was right or wrong. And that turned out to be true. Basically, I just like being right when I say something to my wife, but it's a long time payoff for me. But But overall, I think that's like, that's where my question comes from, like, in my mind, I'm like, three years from now? Like, am I going to be able to turn the targeted 85? Like, is it gonna get smaller when the technology keeps growing, like what can happen here, and I just, I want you all to stay. I want you all to say super excited about it. Like, I feel like I'm your cheerleader unnecessarily. But for everybody else, like don't stop, like seriously little vacation, I except maybe a week on a beach. Okay. And then we're right back in Boston to freeze our butts off and work on Omnipod. Six,
Shacey Petrovic 45:55
no one's taking a vacation, Scott, and we could not be more excited. And I think, you know, Trang Trang. And her team and many others in the company are already you know, they've already distilled the data from our pivotal distill the data from our type two feasibility studies, and they're already hard at work at our next generation algorithms. This is you know, our mission is to improve the lives of people with diabetes. So we don't stop that. And you know, bringing innovation to market is how we do that. And so we could not be more excited. This is a huge milestone for us. But you know, we expect many more milestones as we look forward.
Scott Benner 46:31
Okay. I'm going to ask a question, it's going to lead into another question JC for you. What's going to happen to the arrows pod? Are you going to keep making it? Or I mean, now we have dash we have on the pod five and we for people don't know we have the arrows, which isn't the original pod. It's the OG pod smaller.
Shacey Petrovic 46:49
Yeah, I like to call it the classic Omni pod.
Scott Benner 46:51
I think that's what we should go. So are you going to so here's my I interviewed chuck a few months ago, I don't know if you heard it. I did. I love Chuck. The minute I met chuck in person, I sent a text to somebody, I was like, I need to interview this guy is fantastic. But I tried to get out of Chuck, how much on the pod five product was piled up in Boston, and he wouldn't tell me. But I imagine you've only got so much space and so many resources, and you can't make an unlimited number of devices. Right. So you have a plan for that.
Shacey Petrovic 47:23
We don't have a plan to discontinue our other Omni pod systems on the market today. You know, we recognize that people want choice. I think that there, you know, I think there's going to be incredible demand for Omni pod five, and most people are going to want to move to that product. But we don't have plans to discontinue our classic Omni pod or Omni pod dash.
Scott Benner 47:44
That's very cool. So now that question leads me into this, which is I want to know your thoughts as much as you can share them with me about the do it yourself loop system and that people use Omni pod arrows to run an algorithm that has never seen the FDA and was written by people online? Have Oh, yeah, I've always wanted to ask you what you thought about that. So?
Shacey Petrovic 48:04
Well, you know, what I can say is that we wouldn't be here today with you know, now, multiple system, multiple automated insulin delivery systems on the market without the DIY community. You know, I think the DIY community helped push innovation forward, it probably helped inform some of the regulatory pathways that are leading to interoperability of systems. And so for that we are entirely grateful. And We involved members of the DIY community into the development of Omnipod. Five, because there was a lot to learn from the experience out there that existed. I think the challenge is that, you know, these systems are not they haven't been through the clinical and regulatory, rigorous pathways that Omnipod. Five has. And so we're so excited to be able to kind of provide, you know, provide a system that has the incredible clinical performance and the full muscle of insolate support, clinical technical product support behind it, and, but we're grateful for, you know, the paving of the way that the DIY community did, and it's a remarkable group of, you know, engaged, motivated, talented people, and we've benefited from their expertise,
Scott Benner 49:22
is that partly why you got involved with tide pool because they are taking that algorithm and trying to bring it to market through the FDA. So one day when tide pool gets the okay for their algorithm? Is it as simple as I'll be able to decide if I want to use the one on the board or the one in a tide pool out?
Shacey Petrovic 49:38
I'm not sure it's that simple. You know, we've had a development program for tide with tide pool for quite some time now supporting their regulatory and clinical development efforts. I think it's great that they're working to get this system, you know, through the regulatory process, which is, you know, quite rigorous. But we don't have a commercial agreement with them yet. And I think that's the interesting question. is a big benefit, you know, is the product support, technical support, warranty, all of that stuff that comes with it. So we've got to figure those things out. But, but certainly, you know, delighted to be helping support their clinical and regulatory work.
Scott Benner 50:16
You know, I'm sort of laughing to myself, because I'm thinking back to your previous answer, and I'm imagining, imagining about 10,000 people who use the DIY loop who have been prepping and saving the arrows, pods and clauses and fine. They're like, Wait, I didn't have to stock up on these things. I don't know. I got a couple of drivers. I don't know what to do with all this. It's very, it's a very enlightening conversation. Thank you. It really is. I mean, to your point about that, the DIY group I've seen over my years it push, I think that they're the reason why Dexcom got through so quickly, when they got in the beginning, like, you know, just to what you said, like people are doing this thing already, like, let them do it. i How many years ago? Did I say to you? Are we ever gonna be able to use this on a phone? And you were like, definitely, what is it like six years later? You know, it is. I mean, people are never going to understand the process, and how slow it moves. Right. And I mean, you talked already about you're redesigning a thing, you're packing technology into this little pod, it's not just one, but you don't give me one pod, you give me 10 of them in a bar, how many come in a box, now you changed it can or five? In a box, I need so many I need for a week for a month for a year, that technology lives inside of each one of them. And it just, it bounces online? Because I think most people do see it like, wow, why didn't they like, you know, for instance, like, Well, why is it available for Android? Now that iPhone? Don't they just have to copy and paste that into an iPhone app? Like yeah, I mean, like, it's hard to know, the whole thing. It just takes
Shacey Petrovic 51:57
no, you're right. And, you know, you think about it, we manufacture 10s of millions of pods every year. So you know, part of the FDA clearance processes, ensuring the quality systems, everything's in place to do that reliably high quality, you know, and consistently and with resilience. And so those are that's the you know, that's the not the burden. But that's the that that is why it's a lengthy, rigorous process with the FDA and why consumers that and can be very confident in the technology, like Omnipod phi that we're bringing to them.
Scott Benner 52:32
I, when I saw your your production floor in Massachusetts, I was so blown away with just how amazing it is, you know, the automation and all the technology that goes into building the technology is fascinating. It's why I asked Chuck to come on, because I thought if that guy thought of like this, like, I need an
Shacey Petrovic 52:51
incredible, incredible investment and incredible operation. I'm so glad you were able to see it. I wish I could show it to everybody. I think there's videos on our website, actually, if people are interested in the technology, but you know, just incredible automation, which brings a high level of quality, consistency reliability, to the manufacturing process. And you know, now we've grown so rapidly, you know, more than a quarter of a million people rely on us for their pods, you know, we've got to be able to and we're gonna see a lot more than that with Omnipod. Five, we got to make sure that we have a very high quality, scalable, reliable manufacturing process.
Scott Benner 53:27
Let me let me say something nice to you. For a second Tracy. I have my daughter's had diabetes since she was two. And she was diagnosed in 2004. I started writing a blog in 2007. And not long after that, I started writing little pieces for on the pods website. So that's my the time I go back with all this I've been involved somehow with on the pod before you were here before probably anybody that I deal with was here. There is this, I love the product. And I all I wanted was for my daughter to have it. And I lived with a tiny bit of fear every day before you got to Omni pod that a lot of business people owned it. And they were trying to build it up to sell it to somebody else. That was always a background fear in my heart. And then you got there and I thought oh, this lady wants to sell insulin pumps. And it just like, I mean, I was just so excited. You know, so I can't thank you enough for showing up and and doing that. I can't imagine the one ad you must have. It might have taken some real pulling to pull that those horses around into another direction I would imagine so. I mean, this thing is the it's the greatest thing that's ever happened to my daughter. Like it really has. She's worn one every day since she was four years old. It's almost 14 years.
Shacey Petrovic 54:43
Yeah, that is just I mean, you know, that makes my day that, you know, I'll share that with the team. I can say two things. You know, actually it's not just that I want to sell insulin pumps. I you know, my father lives with type one diabetes. What I want to do is improve the lives of people living with diabetes and you You know, we get to do that it's such a privilege, frankly, to lead this company and be able to see that our technology makes a real difference for people like you and Arden. And the last thing I'll say is, you know, what made the last, you know, several years possible, in terms of really strengthening the company, being able to deliver on the promise of the innovation roadmap, is just adding people like training to our team, you know, we have an extraordinarily talented, committed group of people that are working every day, you know, to deliver technologies like Omnipod, five to the community,
Scott Benner 55:37
you guys do little things that people don't know about, like, I've spoken to your employees a couple of times, just so this, you don't realize there are people that work there that don't have diabetes. And in their mind, they're making a little plastic thing, right, it's their job, and they just know what they're supposed to do. And you go to the trouble of making sure that they understand who it's impacting, and, and why it means so much. And I love coming and making people cry at your thing.
Shacey Petrovic 55:59
And you did, you did a great job of that almost every few months, we have somebody who comes and makes the company cry, as somebody who benefits from our technology. And we also encourage our new employees to wear the pod for, you know, we call it a 90 day challenge, but do what we can to really connect everybody in the organization, regardless of where they are, you know, finance, HR, or the manufacturing line to the daily life of somebody who relies on our technology so that we all understand that our job is to reduce burden. And everybody in the company has a responsibility to do that, and has the opportunity to do that. And so we take that really seriously. Thank
Scott Benner 56:39
you can you speak to. So I mean, there's no ads on this episode, but because I want people to be able to get through it and listen straight through. But, you know, for the last year, I've been telling people get a dash, get a dash get a dash. And you know, whenever you buy something, inevitably the new one comes out the next day. So for the for the group of people who are like I'm on my third dashpot. Are you kidding me? Can you explain to them if they want on the pod five, what's going to happen? Because it's not like and I know you said it earlier, but I just want to say it again, like in the past, they would have been stuck. So yeah,
Shacey Petrovic 57:14
that's right. And it's really important, because it's trying said earlier, we've thought about the customer experience, and simplifying the customer experience, not just through the technology, which we think we've done to great effect with Omnipod. Five, but also through the whole process of trying to access the technology, which we know is really burdensome for people. So that was the whole point in taking the technology through the pharmacy channel. And it enables us to do a few things, it enables us first of all, to let people just go to their local pharmacy and get pods. So some places they have to go to get their insulin and their other supplies anyways, it enables us to eliminate the upfront cost associated and large, you know, deductibles associated with the Durable Medical Equipment channel. And it enables us to get rid of that four year lock in period. So if you acquire dash tomorrow, and then your insurance covers Omnipod, five in a week, you can move right on to Omnipod five. So that is the benefit of the model. And you know, the great thing about Omnipod dash also is that Omni pod five was based on that platform, so it will make your pathway to Omni pod five, much easier from a training perspective. As training mentioned earlier, if you are in Omni pod dash user, and a Dexcom G six user, it's an online training module to then move from Omni pod dash to Omni pod five, once your insurance covers it, so no, no burden, some process to be able to access the technology, no upgrade fee, and no timing requirements, we're going to be able to let you do that as quickly as possible. So I always encourage everybody, you know, even if you think your insurance is gonna cover it next week, there's a benefit to getting on to Omnipod five and there's no cost I mean to getting on to Omnipod dash and there's no cost to move
Scott Benner 59:02
to five, five, the work you guys had to do getting on the pod dash covered by all the all the myriad of insurance companies. By the way, that's not a job anybody wants. But but getting all that worked out, is that going to translate right over to five? Or are you going to have? I mean, is there going to be a gap of time where you're out there? You know, talking to every insurance company trying to get coverage?
Shacey Petrovic 59:24
Yeah, our team has been hard at work establishing coverage for Omnipod five, and we're doing great. We now have more coverage established for Omni pod five than we did you know, months after we launched Omni pod dash, but there are payers who will not contemplate establishing a reimbursement policy until the product is FDA cleared. So, you know, today is a great day for us because it also will enable us to accelerate even faster on the covered lives or number of people that we can get covered for Omnipod five and all of that work is is underway. We do have a lot of leverage you It will launch in a really strong position. But now from here the teams are going to accelerate and get even more coverage established from the pot five.
Scott Benner 1:00:08
Oddly, I just got an image of you in a smoke filled room with a cigar calling insurance companies gone. Hey, we got the clearance. Let's do this. I don't smoke. I know. But that's what popped into my head. It was just completely ridiculous because looking at you, I don't think you smoked cigars. Well, she's the I'm gonna I know you have to go. But you're gonna let me hold on to trying for a little bit. She's happy to do that. Right. Gird your loins. I'm gonna beat you up pretty good. I got a lot of questions. Thanks so much, JC
Shacey Petrovic 1:00:35
thanks so much.
Unknown Speaker 1:00:36
It was great to talk to you.
Scott Benner 1:00:38
In just a moment, you're gonna hear my 25 minute conversation with Dr. Trang lie. But first, if you've heard about the diabetes, pro tip episodes from the podcast, or any of the other content, and you don't know how to get started, go to juicebox podcast.com. There, you'll find all of the series that are available inside of the Juicebox Podcast, not just the daily episodes, which by the way, the podcast comes out on Monday, Tuesday, Wednesday and Friday, every week. But there's also a protip series with me and a CDE named Jenny Smith, she and I break down all of the ideas that are spoken about in the podcast. And I think if you try those episodes, if you really dig into the Pro Tip series, you're gonna get an A one scene of variability where you want it. If you're just starting with diabetes, we have a defining diabetes series, which takes all the terms that you're going to use every day with type one, and explains them in very, very usable fashion. In layman's terms, it's not going to be all technical and medically and boring. It's going to be quick, easy episodes to get you in line with what it is you need to do. And what it is you need to know. You know how there's all those variables and diabetes, we have a diabetes variable series. There's also an after dark series where topics that don't get spoken about much get tackled. Past topics include heroin addiction, bulimia, other eating disorders, diabetes, complications, being from a family of divorce, sexual assault, PTSD, so much more. There are the things that happen to everyday people just like you that no one talks about, but we talk about it here on the Juicebox Podcast, there's a complete series about algorithm based pumping, which is only going to get longer now that only part five is here. And if you're interested in how we eat well, there's an entire series dedicated to how people eat. Because here are the Juicebox Podcast, I believe that it doesn't matter what eating style you employ. You deserve to know how to use insulin and use it well so you can be happy and healthy, and unencumbered day to day with type one diabetes. Check them out juicebox podcast.com. You can also find the pro tips at diabetes pro tip.com. And don't forget if this is your first episode, subscribe and follow in their audio app that you love using doesn't matter if it's Apple Music, Spotify, wherever you listen to audio, you can get the Juicebox Podcast. I appreciate you listening to all that. Now let's get you back to the show. All right, trying. Let's dig this thing apart. Okay, how's this thing work? What are we going to do? Let's go. Yeah, I'm ready. So let me let me I'll give you a little preamble first. And again, everyone should understand i, we didn't pre plan this, I may ask you something that you're not comfortable asking if that's the case, just say I can't answer that. And we'll keep going. So here's my perspective. I employ a very active insulin management system, like even when my daughter's just using Omnipod five, and I'm using a CGM, and we're making every decision manually. By that, I mean, we are very diligent about a good Basal rate, we Pre-Bolus meals, we understand the differences between the impacts of different glycemic load specific indexes of food, I don't abide high blood sugars. If I miss on a Bolus, I come back at it again, I live by the ethos that I'd rather stop a falling blood sugar than live with a high one. And and that is how we stay very flexible from there. A number of years ago now a listener contacted me and said, I want you to try this Do It Yourself algorithm. Because I you know later I learned that she didn't know how to use it. She thought if I learned I could tell people. So at the time, I did not want to do it. Every reason why a sane person would not want to download an algorithm off the internet and let it give their kid insulin. I had a problem with that. I watched everybody doing it. It was working for people. And overall what I thought was this is the future like algorithm based pumping is going to be the future. If I'm going to do a good job at this for my daughter and for this podcast. Honestly, I need to understand this so I begrudgingly did it. There's a great series of conversations about it in the podcast from me, you know on day one and being like, oh my god, I hate this thing. Why does it shut off the basil when I Bolus like you know, like all this stuff. But now I found a real happy place with with algorithms. And I gotta be honest with you, I'm not going back again, that doesn't make any sense to me, I also got to learn an immense amount more about how insulin works, just by having Nightscout on my phone, and watching the algorithm give and take away insulin, it's a fascinating way to learn how to manage insulin just to watch a computer do it instead,
I meant every word I said earlier, the minute I can have on the pod five for my daughter, I am taking the loop off of my daughter, and we are switching over and it is my wholehearted goal to keep her on it forever. But I feel like there's things I'm gonna have to learn about it. Like there were things I had to learn about the loop to make it as truly like successful endeavor. And so I just want to know what you learned with people wearing it, you know, and then if we can't dig into some of this a little bit.
Dr. Trang Ly 1:06:04
Yeah, I think the profile that you're describing someone who has well tuned Basal rates, who Pre-Bolus is their meals, who really understands the impact of low glycemic foods and high glycemic foods, I think all of that really bodes well for excellent glucose control on the Omnipod five system, you know, we if, if you're able to do all those things, and good glucose control is achievable with AD systems. The reality, Scott is that it's really hard to be very regimented about your diabetes every single day for the rest of your life. You know, I tell people, you know, it's like a exercise program, you know, a lot of us can do it for a day, three days a week, but it's really hard to do that for every single day for the rest of your life. And so, you know, we have built this algorithm for when people you know, underestimate their carbs, or or forget to Bolus, you know, for teenagers who do not Bolus. And that that comes from my clinical practice of taking care of a lot of teenagers, over the years. And so we really want it to work for the broad population of users out there who live with diabetes every day. And, and that means, you know, being able to be responsive enough to what we call an unannounced meal, otherwise known as a meal, where you haven't given a Bolus, you know, so that just happens really regularly in everyday life. And that's what we're trying to do. And, and as, you know, the whole art of this is giving just enough to get this person down, and not overshooting and causing, you know, prolonged, severe hypoglycemia. Because, you know, if that happens, then really, you know, you have not succeeded in this area, and you will cause you know, intense mistrust with with your patient. And so, getting that just right, and that formula just right, for our adults, as well as our little kids, was really important to me. And so I think will work really well for Adam.
Scott Benner 1:08:33
Okay, will will I see, when she's low and stable, like away from meal insulin and away from food? Am I going to see a 110 blood sugar? Are there worlds where she'll ride lower than that? Or?
Dr. Trang Ly 1:08:47
Yeah, in some cases, she could ride low, lower, for sure. But those are the sorts of numbers, you know, 110, between 101 10, you know, waking up in the morning was very, very common in the clinical data that we collected. Yeah, that is, I mean, as you know, that is really the impact of this technology is, is really that overnight glucose control and being able to wake up in range and, and not, you know, being agitated by hyperglycemia. And really, you know, really letting it ruin the rest of your day. That is the beauty of AIG technology is really enabling that. That dynamic glucose control in between those big meals,
Scott Benner 1:09:35
okay. Hey, just because it got past me earlier. Ai D, automated insulin delivery.
Dr. Trang Ly 1:09:40
Yes, that's right. Yeah. Very good with my abbreviating. So thank you.
Scott Benner 1:09:46
Make sure I was doing that. Right. So here's, here's a question for you. My daughter goes to Five Guys. She gets a burger and she gets a shake and she gets french fries. And are she
Dr. Trang Ly 1:09:55
gonna get peanuts? Two from five guys? We don't do that. Isn't that interesting to you? Peanut giant, I have the best peanuts. Alright, I'll
Scott Benner 1:10:02
try next time. Just now you're making I feel pressure, I'll eat the peanuts. So we go in. And here's what I know. I know it's a lot of carbs, right. And I make a huge Pre-Bolus. And for a lot of carbs, but what I also know is there is no amount that I can Pre-Bolus or Bolus, that's going to get ahead of the fat rise that comes about 45 minutes or an hour later. Now, right now, on the system we use, or even previously, before algorithms, I would have made a new Bolus about 45 minutes and I would Pre-Bolus the fat rise. You know what I mean? So yeah, I can still do that, right? Because the fats gonna hit like carbs. So they won't mess the algorithm up? Well, it?
Dr. Trang Ly 1:10:44
No. So you can Pre-Bolus For sure. Definitely. And, and you can wait till your daughter starts to kick up again, before you give more, that's totally fine. Or you could could Pre-Bolus and just let the algorithm run with it, as well. I think high fat meals are very hard to manage, it's likely, if your daughter runs at 5.2, she doesn't have that many of them.
Scott Benner 1:11:14
It's more likely that I'm really good at Bolus thing for them.
Dr. Trang Ly 1:11:20
And she's 17 Scott's gonna go to college soon. And you can't go with her.
Scott Benner 1:11:25
I got a text. Don't worry, we'll be good. But I've just, you know, My bigger question is about the algorithm like, can I put that in? If that works? Like, here's my other question does do fake this fake carving mess up the algorithm. So for people who don't know, some people adjust algorithms by lying about carbs that don't exist.
Dr. Trang Ly 1:11:45
So in our Bolus calculator, you can do everything that you do today. So you can set your insulin to carb ratio as aggressively as you want, or, you know, different times of day, you know, if you're more sensitive, or actually more resistant in the morning, which is much more common, then you need more insulin for those morning carbs, you can set those ratios through the day. And then same thing for insulin sensitivity, you can set that as aggressively as you want for different types of days, and none of that changes. So you don't have to kind of fake the system. I think what I've learned, looking, you know, taking care of people with diabetes is, it's really hard to get it right, even without, you know, training, fake things. So what the system knows is insulin on board. So if there is a lot of insulin on board, it notes to kinda like, take it easy. And if there isn't a lot of insulin on board it, it allows itself to be more aggressive in the presence of hyperglycemia.
Scott Benner 1:12:51
Okay. It's, I mean, listen, it sounds terrific. Here's what I mean. My goal is to take it and, and to get the settings in a place where I just fine tune it as best I can. I just, I genuinely meant what I said earlier. I don't I let me be clear, because I don't want to hurt anybody's feelings. I love the do it yourself loop. I think it's astonishing. As a matter of fact, I don't know who Ivan is, but you have to find him and hire the guy. And you know, but but but beyond that, this the ease of use the simplest that you guys have been saying it over and over again. It's what's in my heart. I just don't want I don't think that, that I care. Here's how I think about it, you don't have to answer. If my daughter is five, five right now and she can be six on on your product. My imagination tells me that in the future, you're going to work on getting the target down. So if the next number of years of my daughter's life are spent at a six a one C while she goes to college, and then one day, you and I are talking about this again, you have I look older, you of course look exactly the same. And you're like, Hey, Scott, good news, we got our target to 90 of bah, bah, bah, whatever. I don't think of those three wasted years. And I'll tell you why. Because I've interviewed so many people, adults with type one who had it when they were children who talked about going away to college, and ever it's just a dumpster fire while they're at college. And it gets so bad that they lose their way. And and a lot of them have to have some sort of like a personal awakening to even like try to bring it back again. It's it's an A lot of people don't come back from it. You know, and it's not the stuff we talk about so much. But it is the real like valid truth about diabetes is that you could burn out you could just be not good at it. Your diet might not jive. Well, your doctor might suck like there are so many things that could happen to you, where you're just calling to stay alive instead of a living well, and I as much as I'm happy to tell you that my daughter is a once he is five, five, I would gladly tell you that it's six, and that she doesn't think about diabetes very often that used to be the tagline of the company. Right, long time ago, make diabetes a smaller part of your life or something like that as a long time ago, but I still I shoot for that all the time. And the look on your face tells me I'm gonna find that with this. Yes. So,
Dr. Trang Ly 1:15:13
so sure, it's, it is really about reducing burden for our users. And, you know, all those things you say about. Just, I'm gonna, I mean, I've been crying a lot this week, God,
Scott Benner 1:15:32
just so you know.
Dr. Trang Ly 1:15:36
I'm gonna try really hard not to, but, you know, I have taken care of so many teenagers who have lost their way. And so a, it really is about reducing burden in ways to just allow them to live their life and not think about diabetes. So yes, all the things you're talking about, about lower targets and getting tighter control, we will get there with better insulins and better sensors, we've got to do it safely with the tools that we have today. And I'm really proud of the system we built that has excellent timing range, remarkable hyperglycemia reduction, and thriving children and adults on the system, who can live their lives and, and travel and not have to think about their diabetes. I mean, I have patients who we used to be my patients at Stanford, and I text them now they're on the system. And then Mom doesn't even talk about diabetes. And I'm like, Oh, my God, are you still she's still using the system. She was a year kid still using the system. But, you know, I get this long text about how she's doing really well at school. And she's top of her class. And, you know, that's what makes me so proud to be here today. So, yes, it is all about that. It's never been really about the numbers.
Scott Benner 1:17:03
Yeah. Okay. So a couple of harder questions based on that idea. I, I like to go happy to sad, happy to sad. I like the way it keeps it moving. So I mean, I don't think it's any surprise to anyone who uses an insulin pump that your site doesn't always last, as long as you hope it will. Sometimes it does there, there are times that my daughter rides in on the pod for 80 hours right into the emergency time at the end, and there's nothing wrong. And there are times where five, six hours before it's supposed to expire, I say to her, Hey, if I was you, I'd bail on this pod now. Right? So is the am I gonna see the algorithm like if the if the sight gets gets janky, and you're gonna see the algorithm pumping, pumping, pumping? Trying to get ahead of it? And does it have much luck with that, from what you saw, I
Dr. Trang Ly 1:17:52
think what you're describing, you know, the algorithm responds to that really well, without over responding to that. And, you know, what we've seen is that, yes, that that is a sort of something we see with all the types of pumps, in fact. And, in fact, it's actually more of an issue in tubes, plans, where people tend to, it's a bit like contact lenses, you kind of wear them, and you kind of forget what day you're on, right? So it can, you know, especially if you beyond that three, four day period of of an infusion set, you can generally see that hyperglycemia we don't tend to see, you know, that much of a problem and certainly, you know, the algorithm can really augment for that type of behavior, it really just sees that as sort of, again, just kind of that increased insulin resistance, so that you know, short term increased insulin resistance, so the algorithms able to respond appropriately, and deliver more can actually give up to you know, kind of 300% of kind of Basal settings so it has pretty well good range of being able to adjust to, to your insulin needs.
Scott Benner 1:19:19
So if my daughter's Basal is 1.1 an hour, if it sees her like randomly heading up, right, she's she's been 100 for a couple of hours, she starts heading up, it starts predicting more. It will as aggressive as it is, as it feels like it can do without causing a low later it's just going to keep it's going to quickly put up the basil to so there are you're you're you're basically doing micro Bolus is through basil, is that right?
Dr. Trang Ly 1:19:46
That's right. Okay. Yes. So micro Bolus is every five minutes. So yeah, so that's exactly you're exactly right. I will say, just to clarify. So when you first set up an AMI You plug five systems, so your daughter's on, you know, one unit a day just just for ease of math, the system will use that information initially, but later on, like, you know, by the second third pod, it will, in fact, not rely on the Basal rates to augment insulin delivery, it will rely more on her total daily insulin, because, again, we don't want people to spend their lives, you know, trying to figure out whether they need, you know, 1.1 or 1.05 units an hour. And so it is really the algorithms Basal rate that is being adjusted over time. But yes, it has kind of its own power to increase with in the presence of high glucose levels. And then within it has its own safety measures. So these are not related to the max Basal settings. And in fact, not related to max Bolus settings that you would set in a sort of traditional pump setting. It has its own safety mitigations. And based upon all the studies we've done over the last six years,
Scott Benner 1:21:16
so when a wearer puts the pump on on day one, it's collecting data on the on the first pot, then I take that I take that pot off after three days, actually, does it take the whole three days to figure out what it wants to know? Or how long does it take for to?
Dr. Trang Ly 1:21:32
Well, since you asked is 48 hours, so
Scott Benner 1:21:36
So yeah, so will I see a change on day three or not? Until pod two?
Dr. Trang Ly 1:21:41
Not until pod two. Okay.
Scott Benner 1:21:43
But now I wear pod two for three days, I'm getting the benefit of what it learned off of pod one. When I go to pod three, the 48 hours doesn't start over. Right? It just piggybacks on to what it knows from the
Dr. Trang Ly 1:21:54
Yes, you got it just right. Yeah.
Scott Benner 1:21:56
Okay, look at me paying attention. You don't know me. But anytime I'm focused, it's kind of amazing. This podcast is the only thing I'm an adult about the rest of my life, you just be like, why am I talking to this guy? But right here, you got the right guy? Is there anything that I didn't ask you about it that you were like, oh, we should have asked about this?
Dr. Trang Ly 1:22:22
Honestly, I think you've covered everything, I just want people to know, we're really proud of what we've built here. And it's going to change a lot of people's lives. You know, I get asked by patients all the time, you know, when they can get on edge. We we just have wonderful stories of you know, we have a child who is actually taken care of by his grandmother for various reasons. And Grandma said, you know, the system is so easy that she doesn't, she can actually send him off to daycare. So he's, you know, only a three year old boy. But because of the system and the simplicity, you know, other people can take care of him, he can go to school, daycare and be cared for by others. And, you know, I was just really proud of that. And I just, I mean, I have so many incredible stories. You know, I think you'll really appreciate this because your daughter was young. When she was diagnosed, you said to Right, yeah, yeah, so this child was six years of age, right? And wetting the bed because of hyperglycemia. So we'd have soit sheets and mattress because of his diabetes. And because of our system, this child doesn't have to wear diapers anymore. That's a
Scott Benner 1:23:55
big deal. Like, isn't that amazing? It just really is, I find that the ones I try very hard not to lose focus, because the podcast is, is pretty management centric. In some places, I realized that most of the people I interact with are, are, you know, on a higher level and are striving for that higher level. So I'm very careful to make sure to interview people who are not in that situation to so I don't forget that. No matter how many people this show reaches there are far many of them that have type one who never consider stuff like this and never find health or happiness. And it's debilitating. So I'm not I've listened you guys are advertisers. But if you weren't, you'd still be here today talking about I'm incredibly excited about this. So I really appreciate you doing all this with me. You did bring up one last thing before I let you go. You brought about you talked about kids go into preschool or their school for people who don't have an opportunity to Pre-Bolus Because of you know their caregivers won't tell helped them or they forget or something like that would the way I would handle it. And I'm not certainly saying you should have told me that you agree with this. But the way I would handle it is if I can't Pre-Bolus I over Bolus i Pre-Bolus. If I can't Pre-Bolus I Bolus for the food and I Pre-Bolus the rise, I know is going to happen by not Pre-Bolus thing I imagined with the algorithm, I could still do that. But my question is about little kids who can't Pre-Bolus At school? Is the algorithm going to see that rise? And try to stomp on it? And will that? Like, I guess what I see with my daughter when she doesn't Pre-Bolus on this current system is that it does a pretty good job of keeping her under one ad, if we don't Pre-Bolus Is that what do you see on your side?
Dr. Trang Ly 1:25:43
Yeah, for sure, when we did all of our testing, those were the exact scenarios that we look into, you know, every person is different, and you just can't control a toddler, you know, deciding, deciding what to eat, you know, I have a four year old at home who is impossible, he doesn't have diabetes, and I just shudder to think what it would be like. So it is very, very challenging. But it is, you know, it is the reason why we need better tools, like automated insulin delivery. And I think it'll hopefully make things easier for people and worry a little less, that they're going to be crazy out of range, you know, if they had no insulin versus with an algorithm that can augment and give more, when they're high. But you know, they may have just been running that school for, you know, an extra 20 minutes and suddenly be crashing low and actually not need that. Pre-Bolus right. You just don't know. And it's just so hard. And, you know, we can't always be with our children. And this, this system really gives people peace of mind.
Scott Benner 1:26:52
Well, I'm excited, I am going to here's my here's my promise to everybody listening, I am going to get on the pod five as soon as I can. For Arden I am going to become a super user of it. And then I'm going to come on here and ad nauseam beat into your head how it works. So because I think you're all gonna you're about to make a real leap with your lives. So I can't wait to try and thank you so much. I can't tell you how grateful I am for you and JC doing this. Thank
Dr. Trang Ly 1:27:15
you. Yeah, of course, anytime.
Scott Benner 1:27:18
Thank you have a great day.
A huge thanks to a huge thanks to Shashi And a huge thanks to JC and Trang for taking time out of their very busy day to come on the show and talk to me. I mean, this just became public three and a half hours prior to when we started this recording, and you're hearing it just a few hours later. This is hot off the presses kinds of stuff. I also want to thank all the sponsors of the Juicebox Podcast and remind you if you ever need them, they're there and using my links helps the show. All the sponsors are listed in the show notes of your podcast player and at juicebox podcast.com.
If you're a US resident who has type one diabetes, or a US resident who is the caregiver of someone with type one, go to T one D exchange.org. Forward slash juice box now and take a few minutes to fill out their survey. When you do you'll be helping people living with type one diabetes, and supporting the show. If you have any trouble learning how to subscribe to a podcast, go to the Facebook page for the podcast Juicebox Podcast type one diabetes, it's a private group, you'll answer a couple of questions and make sure you're a real person. And once you're in a bevy of information awaits you, and conversations with people all the way from newly diagnosed to people who have been living with type one forever. There's a equal mix of parents of kids with type one and adults living with type one in there. There's also a bunch of type twos, people who have Lada I'm very proud of that group. It is a wonderful place for people using insulin doesn't matter if you have type one, type two, if you're the caregiver, or have type one yourself, and just like the Juicebox Podcast, the Facebook group is absolutely free. Why don't you go check it out. Okay, if you're still here, you probably really want the link to go check out the on the pod five. I appreciate you listening this long and making it to the end. If you want to learn more about the on the pod five, go to my special link Omni pod.com forward slash juice box five, that's juice box and the number five Omni pod.com forward slash juice box five. You'll know you're there when you see the words on the pod five automated insulin delivery system first tubeless system with smartphone control and then that excited feeling goes up your spine. That's how you'll know you're at the link because you're gonna see a tubeless insulin pump running Automated insulin delivery system. Its algorithm pumping with an omni pod from Omni pod. Go check it out on the pod.com forward slash juice box. Oops, I did miss the Omni pod for will give me I'm so used to saying it the other way. Omni pod.com forward slash juicebox five. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast share this episode Everybody spread the word
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!
#619 Defining Thyroid: Defining Thyroid: Pituitary and Thyroid Glands
Scott and Jenny Smith, CDE share insights on thyroid disorder.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, welcome to episode 619 of the Juicebox Podcast.
Today's episode of the podcast is the second in the defining thyroid series. And today Jenny Smith and I are going to talk about the glands pituitary, and thyroid, the thyroid and pituitary glands. Now I know you're thinking, oh my god, Scott, so exciting. What are you doing to me? I know. But listen, it's important. If you have autoimmune, you very well may run into hyper or hypothyroidism at some point. Hashimotos disease, in fact, could be around the corner, you need to know what to look for. So, while you might not think this is exciting, it is very needed necessary. Listen and educate yourself. You'll be glad you did. While you're listening, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan, or becoming bold with insulin.
This episode of The Juicebox Podcast is sponsored by touched by type one, learn more about my favorite diabetes organization at touched by type one.org. You can also find them on Facebook, and Instagram. And I heard recently a little birdie told me that I will be speaking at their next event. I think it's an August. That's a ways away. But anyway, go orient yourself with their webpage so that when I say to you, I'm speaking at the next touched by type one event, you'll go, Oh, I know right where to go touch by type one.org and you can go get yourself some tickets. If you're a US resident who has type one diabetes, or is the caregiver for someone who has type one, you could take the survey AT T one D exchange.org. Forward slash juicebox in fewer than 10 minutes. When you do this, it will be completely anonymous. They will be HIPAA compliant. You will be helping people with type one diabetes, and you will be supporting the podcast T one D exchange.org. Forward slash juicebox. If you're looking for the defining diabetes series, they're available in your podcast player or at Juicebox Podcast calm. At that website you'll also find the diabetes Pro Tip series. Ask Scott and Jenny. The diabetes variables episodes after dark episodes algorithm pumping based episodes, how we eat series. It's all right there. It's either in your podcast player or at juicebox podcast.com. At the end of this episode, and at the end of every defining thyroid episode, I will list the symptoms of hypothyroidism, hyperthyroidism, and Graves disease. Do you want to do the glands now thyroid and pituitary? Sure, okay. The weirdest part is the starting over because you have to remember it's another episode. I used to remember the defining diabetes idea. Hey, Jenny. Like like we like we just seen each other for the first time. Yeah. Well, hey, Jenny. Today I'd like to define what a thyroid gland and a pituitary gland are. Sure you want to start or should I read a definition and then we'll talk
Jennifer Smith, CDE 3:45
you can read the definition. I think it's the most specific thyroid gland
Scott Benner 3:49
is an endocrine gland located in the neck that produces hormones to regulate metabolism. The thyroid gland is controlled by the pituitary gland which secretes TSH in effort to trigger thyroid hormone production. But sometimes the thyroid simply won't release enough hormones. An underactive thyroid gland, one that doesn't produce enough hormones will result in hypothyroidism. That's not a bad reaction. I felt pretty good.
Jennifer Smith, CDE 4:16
Oh, that was a very good read.
Scott Benner 4:20
I didn't even like I'm very proud. Two years old, I read two sentences. And I'm like, wow, look at me. Yay.
Jennifer Smith, CDE 4:28
You get the gold star reading award today.
Scott Benner 4:31
So so let's go over it. First. Thyroid is where in your body. So it's
Jennifer Smith, CDE 4:35
located in your neck, kind of like this. Beside that bumpiness that you could feel going down in the middle of the front of your neck, right? But you would consider your throat and on either side. That's why it's called like a butterfly type gland because if you imagine the butterfly body being the middle, the wings sort of spread to the sides of your neck, right? So that's why If you've ever had an evaluation by a doctor, they will put two fingers typically on both sides of that middle of your neck and ask you
Scott Benner 5:08
to swallow. Okay, what happens when you swallow? They can find bumps then on it.
Jennifer Smith, CDE 5:13
Correct? Yeah. So if there are bumps present, indicating something is not going the right way with the gland, then they would essentially do more testing to reveal, you know, what might be the potential problem.
Scott Benner 5:25
Right. And will they feel but they won't feel bumps if I'm, if I'm hypothyroid. Without Hashimotos, though, is that correct?
Jennifer Smith, CDE 5:34
I don't correct. I believe that the bumps come specific to the autoimmune Hashimotos. Yes.
Scott Benner 5:40
Okay. All right. Well, it's a win. And sometimes when you see people who have that little like scar on their neck, that could be that they had thyroid cancer, right. Or, or that their or their Hashimotos was so a lot of work for graves, right.
Jennifer Smith, CDE 5:56
Graves disease. Mm hmm. Yep. Yep. Which is kind of the opposite in terms of hypo hyper, I mean, we all talk about hypose and hypers. Right. But this is a very different specific reason for that. But hyper would be, you know, the potential for having like a thyroidectomy or surgical removal of some parts, but most often it's, it's cancer.
Scott Benner 6:20
Yeah, we'll talk about that when we define Graves disease, I think. Yeah. Okay. So that's where the, that's where the actual
Jennifer Smith, CDE 6:29
the thyroid hormones come from and
Scott Benner 6:31
the gland is right there. Right? The gland is right, though we understand that. Okay, now the pituitary gland is a small gland, the size of a peanut that is located behind the eyes of the base of the brain. It secretes thyroid stimulating hormone, TSH, which helps control thyroid function. I didn't realize that so yes,
Jennifer Smith, CDE 6:52
so TSH does not. TSH is regulated by the way that the pituitary gland talks to the thyroid gland. Essentially,
Scott Benner 7:02
they're nowhere near each other. The body is amazing.
Jennifer Smith, CDE 7:06
No, isn't the body I know.
Scott Benner 7:07
Really? If they were talking, you think you'd make them neighbors? But I guess?
Jennifer Smith, CDE 7:13
I guess not. I know.
Scott Benner 7:17
I include a pituitary in here, because I don't think it gets talked about much when you actually have hypothyroidism. Nor do I think anybody's ever gonna bring it up to you while you're treating it or living with it. But
Jennifer Smith, CDE 7:29
because most people just think that there's an issue here, right? And so while the issue does lie in the thyroid, the way that the pituitary gland responds to the signals, it's getting, they work together. So they're, they're both important to understand. Definitely.
Scott Benner 7:47
Okay, is there anything else people need to know? I mean, that's pretty cut and dry and simple, but they should know their thyroid gland is in their neck, and that it can be looked at manually by their doctor visually, or they could have an MRI taken over as well. Those are the ways that would be looked at. Right. Okay. All right, I will put some more important stuff that people need to know after I let you go at the end of this. Alright, hold on a second. Now I need to keep track of what we've done. Because that is. While I'm moving to the next one, I'll tell people that one check them off. There was one time in 2021 where I had Jenny do a diabetes variable. And then like three weeks later, we saw each other and we did the same exact variable again. Neither of us knew that it happened. And that's all right. I was very amused by that. Why don't we now talk oh, what
Jennifer Smith, CDE 8:49
would be interesting would be to listen to both of those episodes and see where they similar
Scott Benner 8:54
it. And I did Jenny and I put them together in their variable. I forget which one it was. Because interestingly enough, we we sort of built on what we said previously without knowing it. Oh, okay. It was very interest, maybe
Jennifer Smith, CDE 9:10
with a subconscious realization that we've already talked about this, but these are the additional pieces to it, right? No one said
Scott Benner 9:18
it out loud. So I put them together. All okay. Okay, so let's put together here. Let's
Jennifer Smith, CDE 9:26
put well I think maybe the next thing would really be since we talked about like Hashimotos hypo, the glands that are specifically involved, maybe the types of tests like the hormone that would be being produced and how they work. Okay,
Scott Benner 9:43
so talk about,
Jennifer Smith, CDE 9:47
you think T sh t four T three. Yeah, that kind of stuff.
Scott Benner 10:00
A huge thanks to touched by type one for sponsoring this episode of The Juicebox Podcast. Don't forget to check them out on Facebook and Instagram touched by type ones mission is to elevate awareness of type one diabetes, raise funds to find a cure and inspire those with diabetes to thrive, touched by type one.org. And if you're a US resident who has type one, or is the caregiver of someone with type one, please go take the survey AT T one D exchange.org. Forward slash juicebox. Looking for community around type one diabetes, look no further than Juicebox Podcast, type one diabetes on Facebook. It's a private group with 20,000 people just like you.
Thanks so much for listening today. Please stop back frequently for more episodes of The Juicebox Podcast and to continue with a defining thyroid series. If you like Jenny, she's for hire. You can find her at integrated diabetes.com. She helps people with their type one diabetes, she really good at it. So if you're enjoying the Juicebox Podcast, and you're listening in an app, but you're not subscribed or following, please hit subscribe and follow on that app. And don't forget to tell a friend. Hey, if you find the podcast on YouTube, we started putting up animated versions of the defining diabetes series. They're really cute, great for kids. Very visual. Go find it. Alright, now let's go through the symptoms. We will start with hypothyroidism. Hypothyroidism signs and symptoms may include fatigue, increased sensitivity to cold, constipation, dry skin, weight gain, puffy face hoarseness, muscle weakness, elevated blood cholesterol level, muscle aches, tenderness and stiffness, pain stiffness or swelling and your joints heavier than normal or irregular menstrual periods. thinning hair slow heart rate depression impaired memory enlarged thyroid gland. In infants you're looking for a yellowing of the skin and whites of the eyes which is commonly called jaundice. In most cases this occurs when a baby's liver can't metabolize a substance called bilirubin, which normally forms when the body recycles old or damaged red blood cells. You also might see a larger protruding tongue, difficulty breathing, hoarse crying, or an umbilical hernia. As progression happens in infants, you may move on to constipation, poor muscle tone, or excessive sleepiness. Hypothyroidism in children and teens may indicate with poor growth resulting in a short stature, delayed development of permanent teeth, delayed puberty, poor mental development. That list is from the Mayo Clinic. Let's move on now to hyperthyroidism. This list is from the Cleveland Clinic. Hyperthyroidism may present with rapid heartbeat or palpitations, feeling shaky and or nervous weight loss, increased appetite, diarrhea and more frequent bowel movements, vision changes, thin warm and moist skin menstrual changes, intolerance to heat and excessive sweating, sleep issues, swelling and enlargement of the neck from an enlarged thyroid gland. Hair loss and change in hair texture. It would get brittle, bulging of the eyes as seen with Graves disease and muscle weakness. Okay, back to the Mayo Clinic for Graves disease, you're looking for anxiety and irritability. A fine tremor of the hands or fingers heat sensitivity and an increase in perspiration where warm or moist skin weight loss despite normal eating habits, enlarged thyroid gland changing menstrual cycle erectile dysfunction or reduced libido. frequent bowel movements, bulging eyes, fatigue, thick red skin usually on the shins or tops of the feed, rapid or irregular heartbeat palpitations, sleep disturbance. If you your child or someone you love has any of these symptoms, please seek medical attention. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!