#987 Glucagon Story: Aimee
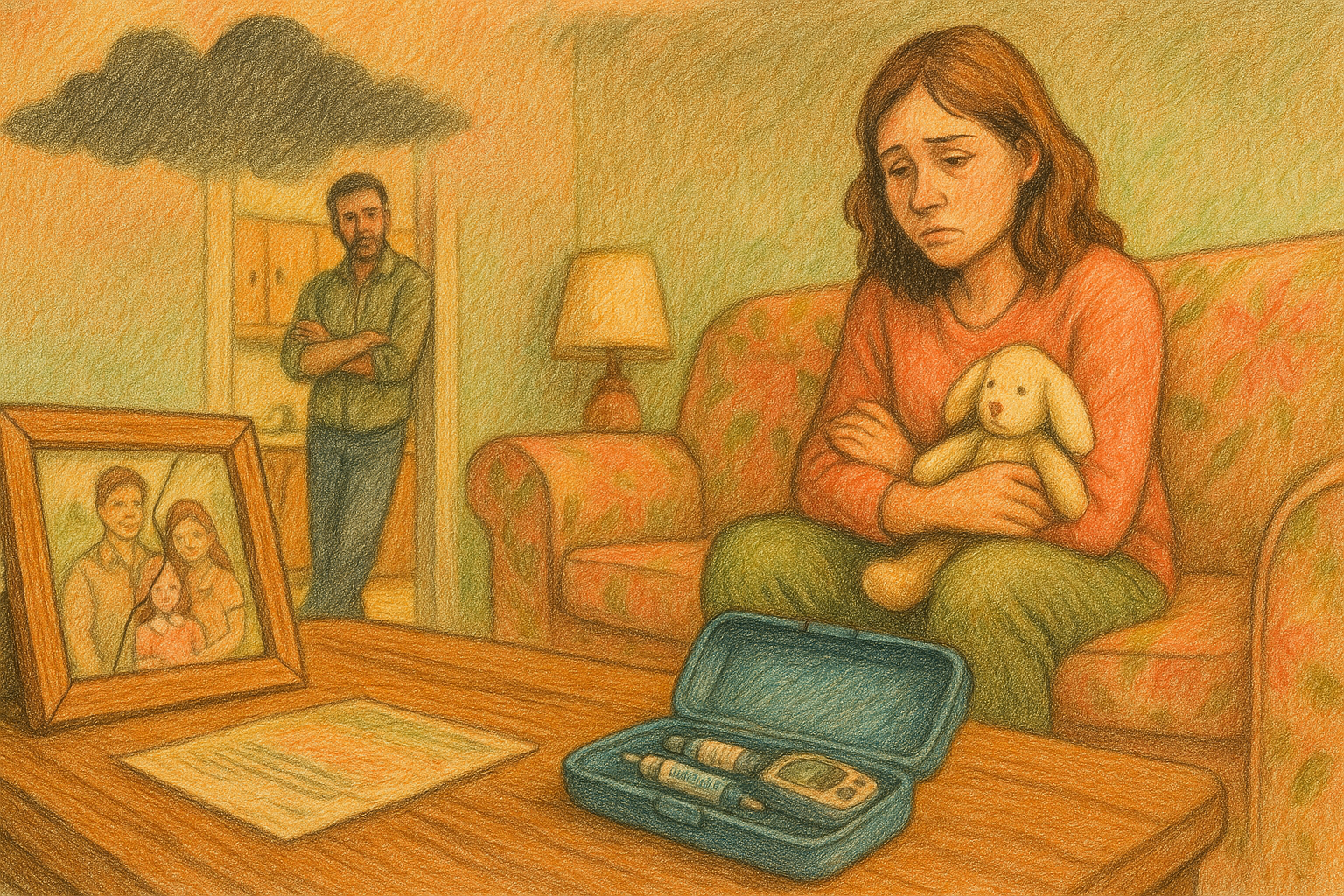
Aimee's girls have type 1 diabetes and she has used glucagon. This is her story.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, welcome back to another episode of The Juicebox Podcast
My guest today is Amy. She is the mother of two young children with type one diabetes. And she's here today to share her glucagon stories. While you're listening, please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your health care plan are becoming bold with insulin. This show is sponsored today by the glucagon that my daughter carries G voc hypo Penn. Find out more at G voc glucagon.com. Forward slash juicebox. When you have diabetes and use insulin, low blood sugar can happen when you don't expect it. GE voc hypo pen is a ready to use glucagon option that can treat very low blood sugar in adults and kids with diabetes ages two and above. Find out more go to G voc glucagon.com forward slash juicebox visit GE voc glucagon.com/risk.
GE voc is a prescription injection for the treatment of very low blood sugar in adults and kids with diabetes ages two and above. Do not use if you have a specific type of adrenal or pancreatic tumor, starvation, chronic low blood sugar or allergy to evoke High Blood Pressure hyperglycemia and serious skin rashes can occur. Call your doctor or get medical help right away. If you have a serious allergic reaction including rash, difficulty breathing or low blood pressure, visit G voc glucagon.com/risk for more information.
Aimee 2:04
My name is Amy and I am the mother of Zoey and Riley, who are three and five years old. They are both type one diabetics. And yeah, glad to be here today.
Scott Benner 2:15
Thank you. I'm I'm very pleased that you were able to do this. So thank you. Okay, so Amy. Have you used glucagon with both of your children just one of them.
Aimee 2:28
So only Riley has had to use G voc before we did have a little bit of a scare with Zoey after we had done it for Riley. But we were a little bit more experienced at that point. So we could kind of tell that she didn't. She was a little bit out of the woods by the point that we were thinking about using it. So only Riley has used it so far. Riley's how old she is five right now. She was three years old when we used it.
Speaker 3 2:53
And so he's held today. And so he's three right now.
Aimee 2:56
And she was diagnosed at 17 months old.
Scott Benner 3:00
Okay, all right. So my first question is when your first child was diagnosed, how was glucagon explained to you if at all,
Aimee 3:13
Riley was diagnosed and then so he was diagnosed 14 days later, it was like a whole thing. For Riley, we were immediately given g voc and it was basically explained to us as use this, she is, excuse me use this if she goes unconscious from a low blood glucose. It's not something that's very common to happen, but you need to know how to use it. When Zoey was diagnosed, two weeks later, we were actually given the Lilly, the old red box kit, which is the syringe and vial that you have to mix. And immediately we were like, why did we not get the same thing for both and then it was explained to us that you had to be a certain age. And we were able to switch her over to G voc after she got a little older. Yeah, so she was 17 months old and she was diagnosed and we were able to switch her to G voc when she turned two. She gets a little bit it was a little bit before because it was actually by her weight. But the FDA approval is ages two and up for for the whole hypopyon
Scott Benner 4:07
Gotcha. So she got Riley got Jeeva pypo Ben and then you got the red box for Zoe but then when she was wait appropriate age appropriate slash age appropriate she moved to Chico hypo pen to Okay, exactly. Yeah. So then what? And but but still, the idea is, you're told if she passes out, hit her with this.
Aimee 4:33
Yeah. Which I knew a little bit better than that only because I have experienced with my sister. She was diagnosed when I was like six years old. She was 11. So I kind of knew that, that you can use it before you actually like you actually pass out that you should actually use it when you're exhibiting like extreme severe low symptoms. So like that drunkenness sort of like behavior and a loss of consciousness not being able to eat to keep yourself From getting that low, so we had a little bit of a primer going into it. But at the hospital, that is what they told us.
Scott Benner 5:07
Did the hospital know that you had prior knowledge of diabetes from your sibling?
Aimee 5:13
I think some of the staff did. I can't remember if the person, the nurse, who explained it to us are the diabetes educator who explained it to us because we had two different educators throughout our state. So I don't know if the second person actually was familiar. But I know that there were some things that we were kind of told, okay, well, your kid, your other kid was just in here two weeks ago. So we know that you've already gotten all this information, and they just kind of gave us like, the highlights, you know, by the time that the weight was in there.
Scott Benner 5:40
Okay. Did you feel comfortable leaving the hospital that you understood it?
Aimee 5:46
Yeah, I was definitely like, I hope I never have to use this. And we weren't given any training with like, any kind of demo pen or anything when we were in the hospital for voc specifically, which was kind of weird to me, because it's kind of like they make you practice all the injections and the finger poking and all that stuff before you, you're able to leave, why wouldn't they train you also on how to use this life saving thing that is supposed to keep you from essentially, you know, going into a coma or dying? God forbid? Yeah. So that was kind of weird to me. But again, like, since I kind of knew how things worked, and I'm just a very, like, I'm a very, like, I'm gonna go on the internet, and I'm gonna YouTube it. And I'm going to seek other people's experiences. Because I feel like, just in general, with diabetes and other conditions that medical professionals kind of give you. They give you what's in the book, what they're told to give you, but they don't really always have like, functional experience using it. So yeah, I definitely went online and just kind of looked up other people using it and things like that to kind of familiarize myself.
Scott Benner 6:47
Well, great. I'm glad you did that. And when did it come in handy? What what led up to you needing to use it with Riley?
Aimee 6:55
So Riley was diagnosed in April 2021. We were about seven months into diagnosis when she she had been on she had just gotten on Omnipod dash over the summer. And she was still honeymooning, like super hard. So she was super sensitive to insulin one day and not so sensitive the other days, actually very resistant. And so we have been having a bout of like, really big resistance with her in that week. And then she ended up having a pump failure that morning. So she shot up to like way over 400 for like one of the first time since she had been diagnosed. So we went ahead and you know, we we used her active sensitivity, her correction factor that had been adjusted that week for the insulin resistance that she was experiencing. And sure enough, because that's how everything works. Her pancreas decided to show up at the same time, and she basically got what we what we later realized was like a double correction because we corrected and then her pancreas was already starting to try to bring that down as well because she was still honing honeymooning. So yeah, she had really aggressive correction. And then she just started dropping like, the fastest that we have ever seen her drop. And she started kind of slurring her words, she was getting kind of wobbly, again, like that sort of description that they give you when someone is like disoriented or drunk and very out of it. At the point where she started not responding to like, questions, not even like nodding or saying yes or no. And she wouldn't drink any more juice. We were like, Okay, we're three juices into this. She's still like, dropping really fast. And we had started giving her juice like in the two hundreds to kind of anticipate that she was going to have this big drop, because you were seeing the fastball. Yeah, so we had her on Dexcom already at that point, too, since she was on the pump. And so she went from like, well over 400 to like 300 and a matter of maybe like 15 or 20 minutes like her. And this was on Nova log, which is not really an ultra quick acting insulin, we were like, Okay, well, this is a big correction, but we'll have time to catch her if, you know, but again, what we didn't know was she was already getting insulin probably from being in honeymoon from her pump, or her pancreas showing her
Scott Benner 9:09
or her body was like don't worry, I can get it this time. Yeah. I so wish I could call your little, your little section of this three drink minimum. But
Aimee 9:21
that's how we felt we were like, Okay, this is this is a lot of juice boxes. I mean, just a little bit. Again, she was three years old. So just like the tiniest bit of juice would normally bring her up within like, I'm not even kidding, like five or 10 minutes, she would be up like 100 points. So when we realize okay, we're like two and a half three juice boxes and she's still dropping her finger stick is still showing us that she's like, like, just dropping like 3040 points. Like, at a time it was crazy.
Scott Benner 9:50
Where we're in that process. Are you starting to think? Where's the glucagon?
Aimee 9:56
So it was it was somewhere between again like The third juice box and then realizing like okay, she's actually not acting herself now. She's normally like, really bubbly crazy running around. And she was just kind of slumped over on the couch, just like really quiet, staring at a wall. Like not even paying attention to the TV or anything like that. And it all happened like super fast, which is kind of like the most crazy thing about it. She just went from like, normal self to, again, just like a shell of herself sitting on the couch. And just, we were trying to like ask her Hey, like, you know, are you feeling okay? We just gave you a lot of juice is because your tummy hurt. Because we knew that that was also something that could happen. Obviously, we're pumping her full of juice. And she was just kind of like not responding. Yeah. So I said, Okay, well, let's go grab that evoke. And by the time that we grabbed it, that was like already holding her. And I quickly looked over the instructions, because I had kind of seen it before. And again, like I looked everything up online. But always in that moment, you're kind of like, okay, your hands are a little shaky, because you've never had to actually do this before. So I just looked over the instructions, and it's literally right on the package. It's the greatest thing. It's, it's like four or five little boxes right on the package that tell you step one, step two, step three. And it was super easy. I read them out to dad that grab that evoke, and pop the cap off, pushed it against her skin, held it for the five seconds, you can literally see the medication going in. So you don't have to like, like, I have an epi pen and with my epi pen, I kind of like hold it there extra long because I'm never sure if it all went in. But with the little windows evoke it's they make it super easy. The the window will show the medication going through and then it'll turn red when it's all done. Yep. Oh, it's I don't know if it's like kosher to say this or not. But it's literally like idiot proof. Like you just you just jabbed it against your skin. And it does it does what it does.
Scott Benner 11:54
I'll check with the attorneys. I'm not sure if you're allowed to call it or not. But if you are, we're definitely leaving this pardon. I know it's talking about I've had the trainer pen. I've used it a million times just to look at it. It is it is explanatory. It feels explanatory. While you're doing it like you it feels like without the instructions, you could still figure it out. Yeah. And honestly,
Aimee 12:17
because she was so little, and I know this doesn't apply to everybody. But she was she was three years old, three years old are still scared of, or nervous around needles and things like that. And I was just imagining like, Okay, if I had to use like the old kit, this would be like a needle she's never seen before, a process she's never like gone through. It was something that I think would have made the whole situation just a lot more stressful and even more scary than it already is. When you're at that point.
Scott Benner 12:43
It's also not near your face. And it's, you know, it's something that can happen. She wouldn't even maybe could even not notice that you were doing it while it was happening.
Aimee 12:52
Yeah, like afterwards, she was like, Oh, I asked her because I was curious how it felt. And I asked her and she said it, it felt like a Dex calm. But when the Dexcom hits like a soft spot that you're like a nerve or something. So it's like a little bit more of a sting than a Dexcom insertion. So I don't know if that helped that she had that to compare it to or not. But my sister has also used it. And she's also said that it's very similar, it does sting a little bit more. But it happens so quick. And you're not in control of having to like push down on a plunger or anything. So if you're doing this to yourself, and you're like afraid of needles yourself or anything, it's literally something that you can just kind of take a deep breath, close your eyes, and just do it without having to put too much thought into it. Yeah.
Scott Benner 13:36
How long did it take for her to kind of come up again and and act herself.
Aimee 13:42
It was like instant. We checked her at like five minutes because we were concerned that we might have to use a second one because we know that sometimes the first one doesn't always dump enough glucose into your system. So we just started checking her at like five minutes. It's supposed to take about 15 minutes to work, but by five minutes, she was already up at like 80 to like 100 from 42. She was 42 when we actually administered it. Yeah,
Scott Benner 14:08
but more importantly than the number you were you were addressing symptoms like you said shell of himself not responding to commands like that kind of stuff.
Aimee 14:17
Yeah, like she was already like, Oh, what's that called? Like? Like talking to us and inquiring about the experience she had just gone through within like 10 or 15 minutes?
Scott Benner 14:28
Yeah, just her brain just shutting off because the glucose leaving our system. It's crazy. It's crazy, isn't it? Isn't it crazy that glucose is like the gas that makes your engine run? And yeah, you need enough but not too much. Not too little like geez All right. G voc hypo pan has no visible needle, and is a premixed auto injector of glucagon for treatment of very low blood sugar in adults and kids with diabetes ages two and above. Find out more go to Jeeva glucagon.com forward slash juicebox G voc shouldn't be used in patients with insulinoma or phaeochromocytoma. Visit G voc glucagon.com/risk.
Aimee 15:10
Yeah, it's it's pretty insane. And it's exactly what you described it, she literally looked like she was running out of gas like she, she was just like coasting along the highway, like this super high VG. And then all of a sudden somebody hit the brakes. And she's just like sputtering down the road, like stalling out. And then we use G voc. And there comes like, she's coming back up to like, a normal speed. And the thing that impressed me the most about it was like, she didn't have like, the complete opposite, like this dramatic, like really uncomfortable rebound. She wasn't like, from 42 to like, 400. Again, she came up and she came up quickly, but she came up, like, smoothly, I don't know if that makes sense.
Scott Benner 15:52
That's fortunate. I mean, the body is an amazing thing, right? Like you're shutting off, the glucose is leaving your system, and it starts to shut, what it what it thinks of is like, systems down, you don't need to stay alive. It keeps paying keeps taking things away from you. Trying to keep that little bit of glucose that's left keeping your heart going and your brain going. It's fascinating. You know what I mean? Like, you're amazing how it works, how how desirous your body is to keep going is really something else. Okay, so did you call 911.
Aimee 16:26
So we actually did not call 911. By the time that my husband was already like administering it, I was already on the phone with our Endo. All of this took place in 2021. So we're pretty still like heavy in the pandemic. And I'm terrified to go to the hospital with like a diabetic kid at this point if we can avoid it. So I got on the phone with our Endo, and they stayed on the phone with us for like 20 or 30 minutes, as we were checking her glucose coming up. And then they even spoke with her to make sure that she was like back to her the right cognitive level and everything. And they felt really comfortable since since we knew that the cause was like this pump failure. And then, you know, her honeymooning plus our correction, it wasn't like just this out of the nowhere thing. They were very comfortable with like, Okay, we'll check in with you again in two hours. And if she's good, then we'll just stay home, because it's going to be a lot worse if she ends up getting COVID This was before the vaccinations and all that stuff. So diabetes and COVID was would not have been a good mix. That's
Scott Benner 17:24
amazing. I, I'm glad it worked out so well for you. Was it in your mind right then to say, hey, we need another prescription for G voc hypo pen? I
Aimee 17:34
Yeah. Actually, I mentioned it to them. And I was like, I'm gonna email you like not today, but probably sometime this week. And we're gonna get in touch with our rep for the area for G voc. And we did exactly that. And they were able to get us a trainer pen as well. So now everywhere that the kids go when they have like, you know, family that they haven't stayed with before and things like that. They have their trainer pen, and the first thing that they do is whip that thing out. And they're like, this is how you use a G voc and this is when you need to use it.
Scott Benner 18:03
I use that same trainer pen, not yours. Of course I have my own. But I use my own trainer pen to show Arden's roommates in college. So yeah,
Aimee 18:12
no, it's fantastic. I was actually surprised that we don't. I mean, I guess they don't want to get one with every prescription. But it should be something that you can that endocrinologist are able to give to their patients especially like at the diagnosis onset, there's nothing like having it like in your hands and being able to feel it, touch it and practice it. Like even just a couple of times before you leave the hospital at your office. You're in those office or even at home. I've had like I mentioned before, I have an epi pen. And the first thing that they gave me when I got my initial prescription was they gave me a trainer pen. So I was a little bit surprised.
Scott Benner 18:46
Yeah, that's a great idea. I will bring that up to somebody. Because in my mind, it takes away the anxiety because you actually get to do the whole process without it actually giving you you know, anything? Of course yeah. So you can it really does you just do it a couple of times you till you think well, this is simple. You know, like okay, take off the cap, click Wait, click again, the window clears like it turns a color. So I know it's gone in like bang, this is this is it. And then after a while, that feeling you had which is interesting, right? Because you open that package up and you're like, Well, let me just make sure we read the instructions one time. Yeah, it can't get it keeps you because you also don't want it to go wrong. You're like, I've got this thing here. It needs to work. Now. I I'm telling Amy I don't know how many people can appreciate that story. But I've my daughter had a seizure when she was like little like, I don't know, three years old, maybe two or three years old. And it's a a test of your adult notice. It really is. Yeah, like because your brains just like just going like cursing it's just like and you're trying you're trying very Hard not to like panic. And there's this feeling like I have to do this thing right now, or this is going to be really bad. And it's a, you see people in a scenario that you've never probably seen a person in before, like that faraway look, or a seat or seizing, you know, like, these things are shocking when you see them. And you don't have time to be shocked. And you definitely don't have time to, you know, be working like Dr. Frankenstein drawing things up and etc. Like being able to pull that pen off and be like, click, click, click bang, that's really valuable. So I've said it before. You know, I was super excited when Chivo came out. And I went after them. I was like, This is it, my daughter's finally gonna get to carry glucagon that I think people could use. You know, it's been, and it's just interesting to hear how it worked for you. I appreciate you sharing this with me.
Aimee 20:58
Yeah, I do want to mention too, that it also. So obviously, I was my husband and I were the ones administering it to Riley. But it makes it so easy that number one a person who is the diabetic person themselves and feeling this way. It makes it foolproof, like they can do this to themselves without like you said, having to fumble with a vial and a syringe and all that stuff. When you're, like you said, your brain is literally shutting down and you can't think about all of these steps. But also it makes it really accessible to the general public. Because I feel like I had never really thought of it this way before. But most people know what an epi pen is and how to use it. At least the basic steps. And this is a real diabetic Emerton like this is a real emergency for a diabetic person that is literally on par with what a person in anaphylactic shock goes through. And I don't understand why we don't have more education and more accessibility around glucagon and just revoke this auto injector that literally anybody who's never had any experience with diabetes, or needles or anything like that could administer this to somebody if they were educated, know what it was for and when to use it in an emergency situation.
Scott Benner 22:06
I agree with you. That is definitely something that needs to be talked about more. It's why I'm making this episode. I've had too many experiences and too many conversations, where it's painfully obvious that many people are living with type one, or helping someone with type one. And they don't know the first thing about this. And I sometimes think it's because a doctor doesn't explain it. I sometimes think it's because you think oh, this is never really going to happen. But it doesn't take long to learn. And
Aimee 22:37
even amongst like diabetics and stuff, my sister was diabetic for 27 years when we were prescribed Evoque she saw us use it oh Riley and she immediately switched over from the old from the, you know, the box kit with the syringe and the vial because she was like, this is something I can do to myself. Yep. And she ended up using it two months later, she ended up actually having to use it. And she was like, wow, I could not imagine drawing a syringe and vial in this situation, I literally would have just, I was alone. And I would have been unconscious by the time that anybody like realized that I needed this.
Scott Benner 23:07
Well, I just recorded another I'm doing these all in one day, the short recordings. The one I did earlier this morning, young girl like 2122 years old. By the time she's like in her 40s She's drinking like sodas trying to like get her blood sugar to come up. She's finger sticking. When she finger sticks. And she's 28 She thinks she's at work. And she thinks I should go home. Like, that's where her brain was. She's like, you know, poem safe, I'll go home. And she ends up passing out and you know, in people who were at her job, give her glucagon. And then the emergency response comes and gives it to her again, twice, I think. But my point is, is that when she really needed it herself, her brain was lying to her. Like it was It wasn't yelling, no get your glucagon out. Also, the instruction she got from doctors was so basic and maybe subpar that it wasn't in her mind, like her mind went to the thing that it thought would help her. I want it to be in people's minds that the thing that your brain thinks, oh, do this now is get that Pannon do this thing. You know. So anyway, I appreciate you sharing this very much. I think it's gonna help a lot of people.
Aimee 24:23
Thank you so much for letting us share of course.
Scott Benner 24:29
It doesn't matter if you're a newly diagnosed person in their 20s a parent of someone living with type one diabetes, or someone who's been living with type one forever. If you're using insulin, G voc glucagon wants to remind you to check the expiration dates on your glucagon and if they're expired, contact your physician immediately for replacements. Don't be without glucagon in the moment that you need it. Have it where you are on your person in your home, at school, at your job, or when you Traveling. Emergencies don't announce themselves. That's why you need to be prepared. Parents of children, this is a perfect time. You're going to end up back at the endos office before the new school year to get your orders in line for the school nurse. Don't forget to ask them about G voc glucagon. If you'd like to learn more about G voc hypo Penn episode 789 is with Jenny Smith and I we discussed the important things you need to know about CI voc. This episode is absolutely terrific to teach you or other people in your life how to use G voc hypo Penn School Nurses, your best friend anybody you're around who might be in a position to help you or your child if the need should arise. GVL Capo penne is the first glucagon auto injector that treats very low blood sugars in people with diabetes ages two and above. Low blood sugar also called hypoglycemia occurs when your blood sugar gets below 70 milligrams per deciliter. When this happens, you can consume sugary foods or drinks to bring your blood sugar back up. There are many reasons why you may have low blood sugar including taking too much insulin, the amount and timing of physical activity and unexpected changes to your schedule. Very low blood sugar or severe hypoglycemia occurs when your blood sugar gets so low that you need help to bring it back up. It is an emergency situation that needs to be treated immediately. If your hyperglycemia is left untreated, it can quickly and unexpectedly progress to severe hypoglycemia. Severe hypoglycemia is potentially life threatening and can lead to loss of consciousness, seizure, coma, or even death. If you experienced any of the following administering glucagon is the next step. You've tried eating or drinking but it's not working. You're unable to eat or drink. You feel like you might pass out or if you have passed out or are having a seizure. I'm just gonna leave you with this. My daughter carries G voc hypo pen with her constantly. It is always on her person. There is another pen in her bedside table. When she goes to college, there is one on her person and one on her bedside table. Everyone in her life knows how to use G voc hypo pen, her roommates, her friends and family members both extended and within our home Jeeva. Glucagon is a sponsor of this podcast because it is the glucagon that my daughter carries, not the other way around. You understand. We carry G Vogue and then I found the company and said if you guys want to be advertisers, I'd love to spread the word. I personally find that G voc hypo pen is the easiest to carry glucagon option that I've ever seen in the entire time my daughter has had type one diabetes. This may seem odd, but I was genuinely excited when we got G voc hypo pen the first time putting G voc hyperopia my daughter's bag gave me a sense of relief that I had not had since she was diagnosed. Ask your physician today about G voc glucagon or go to G voc glucagon.com forward slash juicebox.
If you have a glucagon story that you'd like to share with me on the Juicebox Podcast contact me through juicebox podcast.com Or on the Facebook page Juicebox Podcast type one diabetes. Find out more about Chivo Capo pen at G Vogue glucagon.com Ford slash juicebox you spell that GVOKEGLUCAGon.com/juicebox.
Please support the sponsors