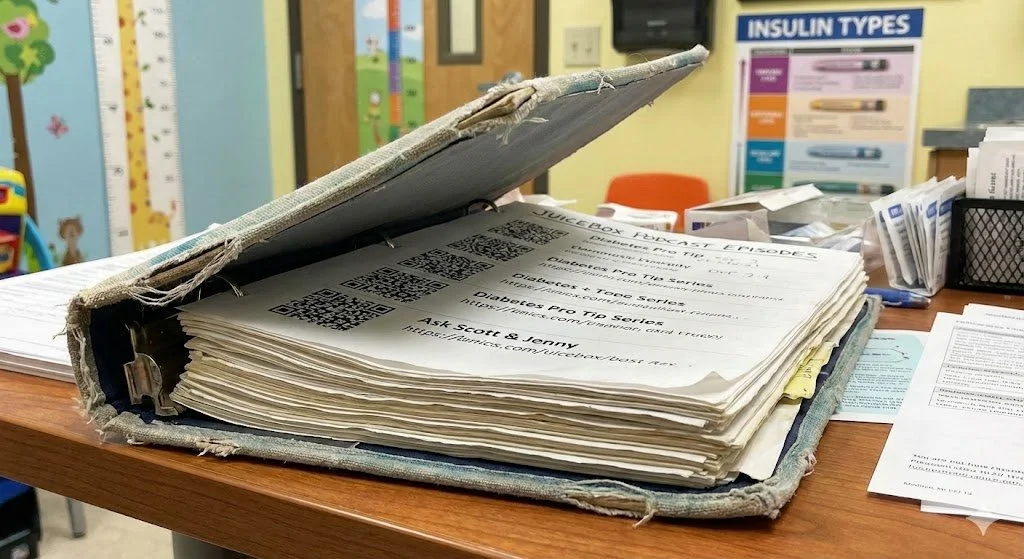
#375 DEXCOM Calibration Practices
To calibrate or not to calibrate, that is the question
Jenny, Scott and the members of the Juicebox Facebook group compare their calibration ideas.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Alexa - Google Play/Android - iHeart Radio - Radio Public or their favorite podcast app.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:03
Hello friends and welcome to Episode 375 of the Juicebox Podcast. On today's show, Jenny Smith and I will discuss different ideas around calibrating continuous glucose monitors. My perspective, of course will come from the dexcom g six because that's what Arden uses. Jenny also wears the G six, but she has worn the Medtronic CGM. And many of you have added your thoughts to this episode through the private Facebook group. For the podcast. I asked this question Hey, calibrating your CGM? Yes or no. And we got a lot of answers. They're all woven into this episode. At the end, I will read directly to you from dex coms website. And of course, while you're listening, I'd love it if you'd remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, please always consult a physician before making changes to your health care plan. We're becoming bold with insulin. I also took a few minutes from the conversation while Jenny was setting up her microphone and everything and she was admitting to not being able to do something around her house and I put it at the end of the episode so you can enjoy it. Jenny is delightful. You want to know something else about Jenny. You can hire her just go to integrated diabetes.com Jenny Smith has been living with Type One Diabetes for 31 years. She holds a bachelor's degree in human nutrition and biology from the University of Wisconsin. She's a registered and licensed dietitian, a certified diabetes educator and certified trainer on most makes and models of insulin pumps, and continuous glucose monitors. She is also a very good friend of the podcast. So check her out. And while you're looking, check out the Contour Next One blood glucose meter go to Contour Next one.com Ford slash juice box to find what I believe to be the greatest blood glucose meter available. Second Chance test strips. super bright light for nighttime viewing. It fits easily in your hand, but doesn't slip away. Well, if that makes sense or not. But it's easy to hold. You don't drop it. I like the shape. I like how portable it is. I can find it in a bag at night without the lights on. I've never told you that before but it's easy to find in a bag. And it's testing ability is just first class. Contour next comm Ford slash juice box where the links in your show notes are the ones available at Juicebox podcast.com. If you have time, I'd also loved if you check out touched by type one.org and T one d exchange.org. forward slash juicebox. Touched by type one is my favorite diabetes organization. And T one D exchange. They're doing research to help people living with Type One Diabetes. And every one of you that completes the research. You just need to be from the United States have type one diabetes or be the guardian or parent of someone with Type One Diabetes. Anyway, when you finish the research, the podcast gets a little help. You know to me a little Cha Ching, and you're helping people live better with Type One Diabetes. It's a great organization 100% HIPAA compliant, absolutely anonymous. You can take your information out at any time, just tell them Look, I don't want to be a part of this anymore. If you want to write so there's no pressure, you'll never have to go to a doctor's office never have to go to a testing site. And once a year, they'll ask you a couple of questions to keep your information updated. And your answers help shape Type One Diabetes Care. It's pretty cool. Being Arden's parent, I was able to fill out the survey took me less than 10 minutes. And I did not find any of the questions to be like I was I was never like, oh god, why they asked me that was all very, pretty simple actually. was easy to do. I think we're going to record an episode today that has the opportunity to be very controversial. Oh, great, but not in a way that I think. I don't think it's gonna get us in too much trouble. So I this is gonna sound crazy, right? But I want to talk about how you manage your G six. As far as calibrating it or not calibrating it goes. And I asked online and got 77 replies. I just said to people,
Jennifer Smith, CDE 4:28
and are all they are they're all different.
Scott Benner 4:30
Oh my god, all of them are so different. So it says I said Dexcom calibration thread, share what works for you. And I did say your tips may be used in an upcoming episode of the podcast. So first, I guess we'll talk about what we do and then we'll dig through all of this now for clarity, right that I mean Dexcom. You know their I guess their public statement is that the Dexcom g six does not need to be calibrated.
Jennifer Smith, CDE 4:59
It doesn't need To be unless it's unless the system asks for a calibration. Okay, in my year and a half of use of G six now I've, I think I've seen it asked for a calibration maybe twice, but its own like, you know, like, this is not right, or I think one of them might have been, you're not right, I'm going to give you a calibration then the system was like, No, no, no, no, no, I'm going to ask for calibration again in like 30 minutes, something I think it what it kind of did. Um, so yeah, technically g six isn't supposed to require a calibration through the whole 10 days of life, right? Unless it requests one.
Scott Benner 5:44
Okay. All right. So there's a whole bunch of information on the website about it, I'll probably read it at the end, just so that it's in here. By the way, keep in mind, I did not tell Dexcom I was making this I don't do that. So I didn't, I wasn't like we're gonna do a calibration episode. It's just something people talk about all the time. And every time someone talks about it, it's like religion or politics. don't mean like, someone will come in and say, Well, here's what I do. And 30 people be like, that's wrong. Don't do that. I was like, wow, everyone has such feelings about this, you know? Yes. So obviously, I think whatever works for you is what works for you. But, Jenny, do you like do you have like a, like a way like, when you start a new sensors, or a thing you do? You just,
Jennifer Smith, CDE 6:30
I started a new sensor. I pop it in, I expect. It's funny. I I see a lot of people you know, work with a lot of people are like, it always kind of like you just said it is always low for a one hour for five hours, six hours after I started up, I know that it's just going to read me low. And whatever. I'm kind of, I think I'm sort of odd in that. Sometimes when it gets going. It is spot on. And I always do a finger stick because I always want to verify where it is. That's just my habit. Yeah. Sometimes it stays completely reliable. from the get go. It's great, right? Sometimes it's a little bit off. But then as it kind of keeps going. It gets right on with a finger stick. Yeah. And sometimes it has that weird. Low. a fun thing about that low is, it always seems to be if I have to change the sensor at night. It's gonna be low. And then I'm gonna be fighting the annoying alerts. All night.
Scott Benner 7:43
All right. Okay. So always the time that I can relate to what you're saying, I might take a detour for a second here. But before I do your, uh, your your spotty on your end. You plugged in the Ethernet, right?
Jennifer Smith, CDE 7:57
I did plug it in. Yeah.
Scott Benner 7:58
All right. Make that mic a little closer to you, please. So I better I yes, I do think that. What's that old cartoon with around head? And do you know what I mean? It's like, if something's gonna go wrong, it will and it's attributed. How is it possible? I can't remember Murphy's Law. Okay, was it a cartoon?
Jennifer Smith, CDE 8:21
cartoon? I think it's actually, I don't know that it's necessarily is maybe it is a cartoon. I don't know.
Scott Benner 8:27
What am I kidding? No, no, it's like rule of thumb. My thinking of I think I may have had a mini stroke just now because I don't think there's any cartoon associated with Murphy's Law. Okay, let's get away from that.
Jennifer Smith, CDE 8:38
I think that this might also be the issue between my voice. I, well, it came with the mic, okay. And I always try to be very protective of the mics and
Scott Benner 8:50
throw that away.
Jennifer Smith, CDE 8:51
I always put the little styrofoam thing back talking
Scott Benner 8:54
styrofoam between the microphone and our mouth. Well, you throw that out, please. No wonder you can't change that light bulb. Everything you said about the light bulbs thing in the episode now just so you know.
So yeah, so I said at the beginning, but just to reiterate, Arden cgms usually go on. And then they read perfectly. And then sometime in the first hour, it just decides that she's low, like, you know, way lower than she is. And if you let it ride out, it comes back up. Now,
Jennifer Smith, CDE 9:30
in a particular time, do you have like a defined time that usually
Scott Benner 9:34
Yeah, I think in like, if I don't see it in like three or four hours, then here I go. I calibrate it. If it's not that, okay, now I don't calibrate low to 90. Right. So we'll talk about that. Like you can confuse the CGM. If the reality is, if the reality is too far from where the CGM thinks it is. Right? You can't calibrate it because it just goes does not compute and you know, it If you fry, it's mine. And it takes forever for it to come back from that. But no if she's, if she's 100. And for clarity, too, I think this makes sense to say, obviously, we're using the Contour. Next One blood glucose meter. If you have a, like an old janky blood glucose meter, you know, the G six is probably way more reliable than your old meter is right? But I'm very comfortable that this meter is, is pretty spot on. And so if the meter tells me she's 100, but it says she's 60 Well, then that's too far apart, obviously. And so I'll calibrate it, but I'll tell it like she's 75 and kind of coax it up, and then test her again a little while later and coax it the rest of the way. So that's one of the ways I sort of, if it's too far apart, I calibrate but I don't you
Jennifer Smith, CDE 10:59
have no timeframe to calibration, coaxing kind of way, like you said, and if it gets up to par quicker, you probably don't calibrate again at all.
Scott Benner 11:09
Or at all he does.
Jennifer Smith, CDE 11:10
Then you'll calibrate again. But that's not like a defined time period after that initial coaxing.
Scott Benner 11:17
Yeah, yeah, I don't have like, I don't have like a magic number to it. Like, like everyone else does. Like, here's a person who said, over 50 points off, I wait an hour for blood sugar's to stabilize. And if it's still off, I pull it and get a replacement. Well, that seems aggressive. Mm hmm. And I wouldn't do that. Because last night, like I said, Arden's sensor went on. around seven, came online, around nine was great. said she was low, around 10. She was in the shower, but I don't think that has anything to do with it. She gets out. It's wrong for a while. And then it just is right again. And then it just shuts off for like, two hours. So last night was That was last night was an uncommon occurrence for us. We don't usually lose a signal during it. But as it came back on, I calibrated it probably two times overnight. And then it's now it's, it's beautiful. Like, if I use this person's theory, I would have pulled it off. And I knew not to pull it off last night. I was like, No, this one's going to come around. Right? You know, and it did. Tina says that I calibrate if it's way off after warm up. But only if it's a stable arrow. I didn't do it once and waited for it to catch up. And that sensor ended up being not good. So there's so much anecdotal conversation in this thread. Everybody knows, I bet you if Dexcom was here, they would just tell you like, Don't calibrate it. It'll it'll figure it out. Right. But what do you do when it doesn't figure it out?
Jennifer Smith, CDE 13:03
Yeah, that's when people get frustrated like this. They're like, well, it's clearly not doing what I want it to do. I haven't calibrated so either. I'm just frustrated enough to pull it off and start a new one up. Or they calibrate and then they calibrate and then they calibrate and then calibrate and you know, I think Dexcom in the first 24 hours tells you not to calibrate, leave it alone, and the system should write itself after that. If the system is off compared to fingerstick. Then if your glucose is less than 70, you can calibrate if there's more than a 30% difference between finger stick and CGM. If your glucose is more than 70, and finger stick to CGM is off by more than 30 points, then you can calibrate. Okay. So those are the rules of thumb that at least used to be a piece for Dexcom in terms of when they would say, okay, it's it's okay, now to go ahead and calibrate. Yes, the system technically doesn't require them. But if it's this much off, you could calibrate because clearly, it's not keeping you where your finger sticks are. And again, I you know, the fact of using an accurate blood glucose monitor. That's huge. Yeah,
Scott Benner 14:24
that's huge. You definitely can't use an old technology. No, there's a Listen, I'll make this argument all day long. If you've got a 10 year old meter, and you've got a dexcom g six, you trust the dexcom g six, not the meter. And you don't tell the dexcom who might really know that your blood sugar is 90 that Oh, no, no, it's not it's 120 this old busted up meter I have here says so. You know, because then then you're then you're literally telling the CGM. Well, you're really 120 and it's going No, we're not. We're 90. That causes confusion. You know, the next person here says Stacy goes, don't calibrate, install the sensor, when the BG is most stable like right before bed, stay hydrated, learn what the trends are for you or your child, because everyone is different. Thanks again for the pocket. Okay, I thought about that. But so her explanation is, she doesn't like to put on a new sensor in a time of blood sugar turmoil, correct up or down or anything like that. Is that also something that helps? Do you think
Jennifer Smith, CDE 15:28
I would expect that it would help? Yes. I mean, I don't. My personal do I pay attention to that? No. I mean, when my sensor dies, I replace it and I started up. But it for those who do have more issue with sensor accuracy from the get go, it could be a very good rule of thumb, because it used to be I mean, eons ago, when sensors first came out, that was the rule with the calibrations, make sure that you have a stable horizontal line or a horizontal arrow, or there's there's not a very large rate of change happening, so that the system can kind of get on par with what it's sensing in a more stable setting.
Scott Benner 16:12
That to me Makes sense. Because if you're rising quickly, and at the moment, you're 71, and you tell the thing, you're 71, it's aware that you're rising your meters not and so by the time you put the number in, you might be 80. And then that's also well, so. So it's interesting here, because the next Lisa comes in and says in these books, these two people are parents, it's interesting the difference between parents and maybe this is where we really give parents and people with type one a little extra because you know they're paying attention a little extra, right? Like I said, like I put my damn thing on whenever I need to. And that's the end of it. But Lisa said new sensor inserted and warm during stable time, she says the same thing. And then she says when it works for her stay hydrated, avoid rapid blood glucose changes during the warm up and the first hours. For example, it looks like they exercise physical exercise be suspicious of unexpected values in the first evening, I hundred percent believe in that I you know, first day of a dexcom. If I don't trust what I'm seeing I check, right. She says she gives a little rule of thumb here. If way off from a finger stick and a flat arrow. I calibrate a value in between but never more than too many malls. are 36 Oh, she's from? Oh, yeah, at least I think is Australian at a time. Normally given one the sensor gets a brain normally given one a sensor gets around. I don't know what she means by that. But so that's it for her right. It's way off from a finger stick. And you have a flat our calibrate a value in between but never more than than 36 points off for American. So I think what she's saying is, if the if the things that if the sensor says she's 100. And the meter says she's 136 she picks a midpoint and tells it Oh, I'm really 118 that's what I sounds like. Yeah, that sounds like what you're doing too. Well, yeah. coaxing it towards the truth. Right. Yeah. It's like the first hour of interrogation after you've been arrested. We don't go right. We don't go right for the for the idea that we start off with. So are you there?
Jennifer Smith, CDE 18:23
Right. I do have to say, you know, I guess I didn't, I guess I didn't really think about it in in terms. Maybe subconsciously. I was thinking about it. But in terms of like the comment about starting a new sensor before exercise. I don't do that. Okay. I will, I guess, again, subconscious level, I will start it when I'm not going to be moving so that things are moving quicker. I just do finger sticks. If I have a sensor that dies before I plan to go out and just do some finger sticks and go about my exercise plan.
Scott Benner 18:59
Yeah, well, we, you know, we've run into situations before where we're, you know, throwing on new equipment. Honestly, whether it's a pump or a CGM, and we're running out of the house or Arden's leaving, but we're gonna split up. And I think I must always say, hey, look, that's a new pump. So, you know, let's be extra careful. That's a new CGM. Pay attention to how you feel you should probably test in an hour. Right? You know, I think we all have feelings around technology, like, you know, a continuous glucose monitor, or even an insulin pump site isn't a television. It's not just like it works. This thing should do exactly what it's supposed to do every time this. There's also a dance it's doing with your physiology. And that's different for many, many of us, and not always repeatable in the same ways. So,
Jennifer Smith, CDE 19:52
right like I think there's some people to someone who is a very true listen To your podcasts, who I've been working with for a bit, and he actually wears two sensors, he wears g six, and he wears the libri. At the same time interesting. And, you know, a piece of it is the benefit with the pumping system that he uses when it's when he has a new sensor, he wants to be able to continue to feed glucose values to the system in order to keep it running right and doing what it's supposed to do. So he uses the libri data then to plug in the glucose values in order to not have to do finger sticks in that time period. But to be able to still give it glucose values, which I think is a you know, if you're not, if you don't really care about wearing more robotic parts, that's a great idea, you know, running those time periods to and I've had them g six for me has been kind of funny I have, I would say I have really good accuracy with it. But by about day eight on 90% of my sensors thus far, day eight, I start to get sensor error, wait three hours, and then it'll come back. I'll get a little data. And then they'll give me another sensor error, wait three hours. And at this point, if I get it twice, on day eight, I'm like, could put the air the sensors done, I take off, I call it in Dexcom is great. They've sent me new ones, but they always ask the same darn questions. I'm like, I don't know why it's dying on day eight for me, but it is so. But I mean, in terms of even just the time periods when you get those errors, having a backup, like wearing a Liebe Ray, which again, also doesn't require any calibration, right? Kind of can give you a back up in terms of your initial system a little overlap
Scott Benner 21:43
it You're right. It's a little overlap. No, no. And we do testing in that time. Like I I don't I agree with you, when when I see people who are like, Oh my god, the worst time of my life is the two hour warm up when I don't have Dexcom. Right. And I think those people must be newer to diabetes or to deck or in general, because I've never once thought oh my god, we've lost the CGM for two hours like this thing. Like last night it you know, it, it um, it lasted the full 10 days, like right up till the to the hard stop. And it wasn't a problem once during the thing. And then the next two hours, I just hold our nose like they get an hour just test. And if you need insulin, give it to yourself. Like you know, the way we did it for years and years and years before this technology exists.
Jennifer Smith, CDE 22:30
I feel like that's probably the case. And it's, I sort of have, I compare it to kind of being like, you're on the mothership, and all of a sudden you get like, spit out the back door, and now you're like Lost in Space is fast. Where am I traveling to? What's going
Scott Benner 22:48
on? I mean, quite honestly. fingerstick I mean, it's I know that and for many parents, I think it's hard when you've gotten so used to a system that you feel like you're saving your little ones fingers. Yeah, you know what? They're gonna be okay. It'll be hard. If you stick their finger, you know, they'll be okay. If you get information that's going to help in the short term, right? I'm helping a person right now. And I said, Hey, why don't you check with the meter, and they have the contour. So I was like, I'm pretty comfortable with this. And they responded back and we're like, we don't we never test. And I said, you probably should a little bit. And you know, and so And now's one of those touches. Why do you want me to test right now? I said, because we're about to do something. And I want to be 100% sure we're doing the right thing. And I don't know you. And you know, I don't know when you put the CGM on, I don't know how you've managed it. Like I just want. I want a little peace of mind here. Right? Don't take your peace of mind from an old meter. But you know, at the same time, Okay, ready? What do we have here? Dana's got some solid advice. I think I've probably calibrated every sensor a few times, but it has to be a flat arrow. I use decks comms for trends, and a finger pick a finger poke throughout the day. So if it's consistently off by 10, or 20 points, over two and three or two or three checks, then I'll calibrate. So if she's off by more like between 10 and 20 points, two or three times, then she brings the the CGM back. I have to admit, I would do that too. I don't know that that she's saying she does it consistently through every sensor. We don't do that. But if I saw that, I agree I would do it. You know. And Arden's a one see very closely matches her Dexcom data. Right so I'm comfortable that I'm doing the right thing.
Jennifer Smith, CDE 24:46
Yeah, mine does too. And that's a lot of people do some comparison. I mean, I'll usually get emails from people and they're like, well my my G ami from Dexcom was telling me this but my a one c came back at this. What's the What is the deal? You know, and I know that we've talked about that before on a couple of other episodes. But, I mean, you have to understand the difference, you know, blood glucose versus interstitial glucose, a little bit of variance there could be, I, myself also have very good comparison between the Dexcom average and my actual agency. They're, they're close. I think that the last one was within like, one point or point one. Um, well, that is,
Scott Benner 25:29
that is definitely how I, in the end, assess whether or not I'm managing that sensor well, right. And it's funny too, because, you know, back in the day, when people were rampid, for information back when information used to go really slow, like a new CGM, you know, the G five would come out and people right away, I get the notes, scotch doesn't work, review it, blah, blah, blah. I'm like, I'm not gonna know for three months. Like, why do you? What are you talking? You asked
Jennifer Smith, CDE 25:55
me two days after, right?
Scott Benner 25:57
Here's how we'll know three months from now I'll look at Arden's data. If somebody sent me an email and said, Please say data for me. So I'll look at Arden's data. And then I'll look at her a one C. And if they match, I'll say Huh, that CGM must have been pretty good. Because there's no other way to tell. And so I do think that this is kind of crazy, because it's user error. A lot of the times right and and not error, like oh, you screwed up. But I think Oh, you don't know how, which is why I want to put this this episode together. Because it just it is like sometimes this thing needs a little massaging. Chelsea said, we calibrate only if the arrow stable. Usually first thing in the morning, and before I go to bed, keep hydrated. Never calibrate when there is no arrow? Because she believes RAC that means the sensors confused in general, right?
Jennifer Smith, CDE 26:53
Correct. That means the sensor is it's still giving you data. But it's it's making sure like all of its little algorithm, whatever it's doing internally there, it's not giving you an error, an arrow of direction, because it's seeing a glucose value. But there's there's it makes sense for them. Yeah, it's kind of confused, I guess. Yeah.
Scott Benner 27:15
She goes on to say trying to calibrate when food or rapid insulins on board. And some people say this is hearse gleaming, I think what other people said to her that works to her, insert it, let it marinate overnight and then calibrate it in the morning. And in fairness, Jeanette came in and said this and put arrows to it. Like she was like, I completely agree with this one. Next person says we rarely calibrate. We know that the next con will oftentimes be off a bit in the first 12 hours. If you do calibrate, do so when numbers are stable and not dropping increasing quickly. Right? Yeah, see people are starting to hear anything idea
Jennifer Smith, CDE 27:56
is not, it's not I guess, proprietary to Dexcom. A lot of people with Medtronic do exactly that as well, because of I think their sensor has long term been a little bit more wonky, kind of in the get go kind of stage. So there are a lot of people who even with the older Medtronic sensors would let it do that, like marination, they'd sort of inserted at night, they'd start it up first thing in the morning, still get another two hours of wait time period, but it was enough that they got rid of that sink in period.
Scott Benner 28:31
Have you ever seen people put a sensor on but and then cover it? Yeah. And not not at all, like put a transmitter in it or anything like that. I've seen people do that.
Jennifer Smith, CDE 28:42
In fact, I've had a couple of parents who do that with their kids kind of this marinate idea. They'll use that whatever it's called caveman. It's like the the sticky wrap. It doesn't really stick stick.
Scott Benner 28:53
Like if you give blood now they wrap it around your cotton, right? Yeah,
Jennifer Smith, CDE 28:56
exactly. So that what they'll do is they'll put the Dexcom on not put anything in it like meaning like a transmitter. And then they just wrap that around let it sit and then they started up when the actual old the old sensor dies.
Scott Benner 29:10
Because index comms been on and in the past obviously a lot and they've they've know I've been told more than once. Right? There's this there's this wire that goes in and it needs time to I mean, let's say acclimate to the interstitial fluid. Yeah, what yeah, I think is what I so it's soaking in, right. I think the idea. It's like, I guess it's like, you know, it's like taking a log and dipping it in water and pulling it back out right away. The logs not wet in the middle from that, but if you throw it in there for a few hours, it'll soak through. Gabriella, I only calibrate within plus or minus 30% of Dexcom readings directionally towards my readings directionally towards my meter I don't get into calibration loops as a result. Have you ever seen a calibration loop personally, where it asks you to calibrate you calibrate and then tells you to calibrate again.
Jennifer Smith, CDE 30:02
I've not not with G six, I have had that with G five. Okay. But again not often either with that,
Scott Benner 30:08
I think I've seen it. I honestly have to say maybe twice. And we've gotten out of both of them by being persistent and, and doing it. Here's a question for you. Let's say you calibrate. And let's I'm gonna try to make up a number here. So let's just say your blood sugar is really 90. The Dexcom says you're 120 and you put in 90, and it says 110. You know, if you put in 90 again, it will agree with you, right?
Jennifer Smith, CDE 30:45
It did not done that.
Scott Benner 30:47
A double calibration on close numbers, forces it to agree. Now, the question in my head always is,
Jennifer Smith, CDE 30:57
does it stick then? Is that right?
Scott Benner 30:59
To do? Or is it just making me feel better? And and all I can say is that when I do that, things go okay afterwards. But I don't know if that's right or wrong. This is probably right, where I'm thinking right now people are listening. And they're just like they're pulling their hair out and punching the dashboard of their car. And they're like such bad information. Let's keep this in mind. I'm just telling you what I've done in the past. I'm not telling you to rule. I'm certainly not saying Dexcom says to do it. We're having a little conversation here about what other people do because it's such a varied thing. Don't do it if you don't like it, like you know, or try it once and see what happens. I don't know. But I don't even know if the outcomes right or not. I do know that it makes me comfortable. You've done it a couple of times. So it's Yeah,
Jennifer Smith, CDE 31:43
seems like it works when you've done it. Well I've done
Scott Benner 31:47
it enough to say it out loud and let my voice would be recorded while I'm doing it. Yeah, I willy nilly on here yelling about diabetes stuff. Right?
Jennifer Smith, CDE 31:54
Right. Yeah, I I've never tried that. I guess the next time that I feel like it warrants a give it a whirl.
Scott Benner 32:01
See what happens.
Jennifer Smith, CDE 32:03
Mike, give that a whirl and see how that works out especially at two o'clock in the morning. I'm like, I'm not low.
Scott Benner 32:11
Elena says I don't calibrate I find that calibrating leads to far more inaccuracy than just letting it go. With that said, I do think the first 24 hours or so of a new sensor can be rough. And it eventually works itself out. Tara, we check on the first day. If it is 20 points off. we calibrate. And if it helps, and if it helps it not to be so wonky that day. Any other time we spot check it it's right on. that'll stop it. She's saying okay. Molly, I have never had to calibrate and when I test as long as my arrow is stable on my Dexcom they match within three to eight points.
Jennifer Smith, CDE 32:51
Wow. That's crazy. Oh, God, I think you know, and I think a big piece of this too, which has now been commented a couple of times. Yeah, I people is hydration. That is a and I know we've talked about it before I've mentioned it before that is just enormously important. And I think especially for for kids, little kids who you kind of have to coax them to drink more, right? And remind them I mean, kids without diabetes, I don't even think parents pay attention honestly, to how much their kid is drinking through the course of the day. But kids with diabetes, certainly especially with the fluxes that they have in their blood sugar. Hydration is huge. And then you've got kids who are very into sport I mean they might be doing something for four hours, you know, four times a week. Make sure they're drinking Yeah, absolutely. So but for sensors specific though hydration is
Scott Benner 33:51
so important well you know your point is well taken because today in the in the private Facebook group for the podcast it somebody asked about their creatine been been created or something like that, like yeah,
Jennifer Smith, CDE 34:03
they're creating and been is Yeah, blood urea nitrogen is what it stands. Thank
Scott Benner 34:07
you, Jenny. And everyone who came in who had any kind of a medical background was like, Look, if I was you, I would just make sure I'm hydrated. You know, Natasha says we used to try to calibrate after the first 24 hours if dex was still over 20% off for the last sensor change. We did a pre soak no see that the new sensor, they soak their sensor overnight, and then snapped in the transmitter in the morning. And it worked without calibrating. dex was very close to the Contour. Next One, thank you for the plug. Once the 24 hours passed, no sex was also less jumpy during the 24 hours. And
Jennifer Smith, CDE 34:45
I've seen that too. That's actually an interesting comment. You know, with G six, the the system has smoothed the data, right so you get this smoother trend line with SJ good? Yeah. But a lot of people have questioned in that first, like, let's even say 12 hours. Some people do get that like that little up gel where you can see that the numbers, those little dots every five minutes, they are more Up, down, up down versus this nice smooth into yeah each other. So that's interesting that somebody kind of commented on that.
Scott Benner 35:25
Well, someone comes in and asks, Do you can you explain pre soaking and she Natasha went on and said before the current sensor expires, apply the new sensor but not but do not move the transmitter. So the type so the type one will still be wearing two sensors one active one inactive for a period of time, this gives the new sensor a chance to acclimate for longer than the standard to our warmup period. If you do this, be sure to cover the new sensor to protect the delicate electronics. We use a band aid
Jennifer Smith, CDE 35:52
Oh, band aid. Yeah, this is completely
Scott Benner 35:54
off label. Obviously, most of our based on the podcast is off label, right?
Jennifer Smith, CDE 35:59
I would expect that a band aid that's one of those like larger band aids would probably be the better option just to protect that internal part of the sensor. Because you know, the funny thing about g six, and I didn't realize it initially after I started to wear it, but g six has this like sticky stuff. Like inside. And when you remove your transmitter, you can see it on there. And that's why you have to clean the transmitter off every time you take it off.
Scott Benner 36:27
Doesn't it remind you of like petroleum jelly or something? Does I don't know what it is, though.
Jennifer Smith, CDE 36:31
Yeah, it's like carmax or like, you know? Yeah, like petroleum jelly gynae.
Scott Benner 36:37
I, I definitely know what you're talking about. Yeah, it um, listen, Linda, we never calibrate. And I have to say to their sensors for weeks in a row that we don't calibrate. Like, I don't need most like, this is interesting to do. But I'm not a person who's in a position of saying, oh, wow, we really need to figure out what works because what works for us is, you know,
Jennifer Smith, CDE 37:02
like, do what works for you. And you might have censored a sensor that one. One, I guess, idea of what to do with this particular issue. It could be different three months down the road when you've got another sensor. Oh, sorry. I thought I had it turned off. But yeah, it might be three months down the road, that it's a completely different calibration need, right that you do something completely different this time versus the last time that you needed to calibrate.
Scott Benner 37:34
Yeah, there's three people here, Irene, Jeanette and Jolie. And they all say the same thing. Like once in a while, like I put it on, and it works great. But sometimes I get it where it asks me to calibrate twice after a warm up, even though it's not supposed to like, have you seen that.
Jennifer Smith, CDE 37:48
And if I have and I didn't see that until Gosh, a cup maybe it was the beginning of this summer that I put a sensor on. I gave it the code and accepted the code. And after the two hours, it was like, you need to calibrate with a with two finger sticks. Now it's like put I fed you a coat and then it I believe it's every 24 hours then if it didn't, for some reason register the code even though it told you you did right, you'll get the two hour warm up two finger stick and after that once a day, you'll get a request for another calibration every 24 hours with a new sensor. Okay,
Scott Benner 38:23
how amazing is all this by the way for it? Listen, for those of you who have walked into diabetes during the time of glucose monitoring, you're probably thinking, you know, Oh, that sounds like a problem. And for anyone, Jenny or me with Arden, who were around before this, I think this is all like astonishingly amazing. And just as magical. You know, Danielle, we rarely check with a finger poke. We only check when we are surprised by what Dexcom is telling us. I think that's important to remember. That is exactly how I feel about it. It's that like when I don't know how to I don't know how I know. But when I don't trust it, I don't trust it. And right, you get that over time. I think
Jennifer Smith, CDE 39:04
it's kind of like with the ones that as you said they start up and it just reads like ello w Yeah, your low your blood sugar's like 39 I'm like, Yeah, I don't feel 39. I know. I mean, I have, you know, symptoms, thankfully for low blood sugar, still. And I would know a 39. I mean, I really would. And so I can be like yeah, that's totally wrong. I'm going to do a finger stick and it's going to come back at like 78 or like maybe 90 or something you know. So symptoms are another piece to it as well if you are feeling very differently than what the CGM is telling you. Even if you haven't done a finger stick in three months. Yep. Figure out where your glucometer is.
Scott Benner 39:45
Go find that. Megan says I don't calibrate if it's inaccurate we go off finger sticks. Excuse me, why can't I say finger sticks until Dexcom becomes accurate. My daughter has been wearing Dexcom for two years. I only calibrate if it's off by more than 50 points, which is rare. And I only calibrate when the arrow is level. Lizzie says I've never calibrated the dexcom CGM. Wow. Yeah.
Jennifer Smith, CDE 40:14
That's amazing. Yeah, it must have been must be somebody Then who's never been on G five because that required cat needed
Scott Benner 40:20
calibration. Right? Yeah.
Jennifer Smith, CDE 40:22
Although, interestingly, I have had people who've worn g five who said
Scott Benner 40:29
they want it back calibrated.
Jennifer Smith, CDE 40:30
I just don't calibrate it. I've just let it and honestly the system will, it will keep running. Unlike g4, and the previous if you didn't calibrate it, it would just stop giving you information. g five would keep giving you data. Okay, it would keep asking for calibrations,
Scott Benner 40:47
but it wouldn't.
Jennifer Smith, CDE 40:48
It wouldn't stop giving you data. Well, you're right.
Scott Benner 40:51
You're 100%, right. Oh, I remember that, too. Yeah. Okay, Sara in the morning with no carbs or insulin on board with a level arrow. So we're starting to see some similarities with people's answers that are that are repeating over I
Jennifer Smith, CDE 41:06
mean, I think if you could put it together in a simple, it would probably be one be hydrated. Yep. To make sure that the glucose value is stable, or that you're in a stable time period, meaning you haven't eaten like the whole basket of like chicken fries, and like ice cream, and now you're waiting for your sensor to give you good data. Right? Well,
Scott Benner 41:24
I'll tell you what, there's a couple of there's a couple of statements in here that really does shine a light on what anecdotal information is. Because there's a person and they're even putting a laughy face in it, who says, I usually only need it during the first sensor session with a new transmitter. I feel like the new transmitter needs a few days to learn me. The transmitter has nothing to do with the measurement of your blood sugar. It's just sending the signal right to but even so that's it right like it you see something over and over again. And if you misconstrue it, all of a sudden you feel like it's a rule. You know? It's like when people's like Murphy's Law. Oh, that thing. Always I love it. When people say this about diabetes, this stuff always goes wrong at the worst times. And to that I always respond, what would a good time be for it to go wrong? Right. Every time feels like a bad time.
Jennifer Smith, CDE 42:19
Right? Exactly.
Scott Benner 42:20
Yeah. Going along and live in your life. And then all of a sudden, something you're counting on stops working. There's a good time for that.
Jennifer Smith, CDE 42:27
Yeah. Always stinks. Yeah, no matter if it's two o'clock in the morning, or when you're on the beach vacation or your whatever, in the middle of a basketball tournament. It's never a good time. Jeff,
Scott Benner 42:40
Brent and Jay, I don't calibrate.
Jennifer Smith, CDE 42:45
If I'm curious for those who are not calibrating
Scott Benner 42:48
how close they're a once the matches there.
Jennifer Smith, CDE 42:51
I'd be curious about that. But I'd also be curious if they're also people that may not be doing finger sticks. So they may not really know if their sensor is really off. Yeah, it. I mean, because, you know, having had diabetes as long as I have. I didn't have sensors for a good majority of my life with diabetes. I didn't. And I mean, my first sensor was in 2006. That's when I first started using them. And so I was always, I still am. I still do finger sticks during the day, even if it's not to check my CGM. It's because it's time to eat. And I'm so
Scott Benner 43:35
programmed.
Jennifer Smith, CDE 43:36
I'm just programmed to do a finger stick. I do a finger stick when I wake up in the morning. I do a finger stick at lunchtime. I do a finger stick at dinnertime. I always do it before I go to bed. And I'll even do more than that during the day with exercise. Right? And I just it's just a routine. It's like brushing my teeth. It's not something I think about anymore. So I think that I'm also a little bit more in tune then with Oh, my CGM is reading this. My finger stick was this. You know, and for those who pomp especially if you're relying on the CGM, but you've not really been doing finger sticks, and you're kind of wondering why Will my GM from Dexcom is telling me this is my average. But every time I get my a one c done, gosh, it looks like I'm a lot higher. Yeah,
Scott Benner 44:21
well,
Jennifer Smith, CDE 44:22
it. It could just be that CGM just isn't reading you as
Scott Benner 44:26
accurately. Do you remember a long time ago in the original Omni pod? PDM there was the meter and that the meter wasn't it wasn't great. And so that's how I figured it out. Right. So how did I figure out the meter wasn't great, because Arden's a one seat kept coming back higher than it should and it didn't matter. This is before CGM, and it didn't match what the finger sticks. were telling me. And that's when
Jennifer Smith, CDE 44:54
we'll figure out how to play with the Kalam
Scott Benner 44:56
Yeah, then you change the calibration code and the meter works better. And so I used to it was 17 or 18, right? All the all the test strips for the Omni pod PDM or code 1616 and some people change the meter to code 17 and some people change the meter to code 18 depending on which ends up being more accurate for them, we were 18 I know a lot of people were 17
Jennifer Smith, CDE 45:19
Yes, I was 18
Scott Benner 45:20
Yes. And then Arden's a once he started matching my expectations, just like that. So you can be mad about it if you want. But at this point, now that meters a decade old, right, and you know, and so the people were like, I can't believe that the new dash doesn't have a meter in it. You don't want a meter in your technology, because the meter keeps getting older. All of our new technology now is updatable, right? It's like your iPhone, you want to put a new operating system on it, you can a new app. But if you stick a physical piece of equipment into it like a meter, now suddenly you are stuck with that meter forever. And that's that's I don't think that's a good play. And I think that's why if I had to guess why Omni pod took it out? I think that's one of the reasons. It could be. Yeah, I
Jennifer Smith, CDE 46:03
mean, it's also the reason I think that they've decided, you know, now when you get on the pod, the dash system, you get the Contour. Next One,
Scott Benner 46:11
right. And the PDM is now really just sort of like a lockdown Android device. Right? Right, exactly. But it's, but the point is, is that I saw that as far as moving on, I kept thinking like, Oh, my God, this meters old, old, old, and I felt tied to it at that point. You know, I am. I hate to say this, but I am so much more happy with the Contour. Next One, then I was with the PDM meter. Back in the day, I'm thrilled with it. And I think that two people listening probably were like, Oh, my God, Scott's taking a meter ad. We know he uses Dexcom, he probably doesn't even use a meter, we use a meter every time we need a meter. And it's a lot more than you think it is. And it's not because Dexcom is not great. It's for the reasons Jenny just said. So I was
Jennifer Smith, CDE 46:55
actually kind of curious, you know, I my insurance doesn't cover the Contour. Next One, I wish it did. It covers the Accu check guide me, which is another very similar to the contour its accuracy. That kind of parallels, right. But the interesting thing is I do have a Contour Next One. And I had like the sample bottle of test strips that kind of comes with it. So I played once I got my Accu check. I was like, I'm just curious. And they were pretty spot on with each other, quite honestly, which was nice to see. But also then went back to my old school PDM and my freestyle light test strips and and I figured out that actually that code 18 is the one if it was the code 18 it was within like two to five points of the contour next in the accucheck. Yep. So that's old school as it is.
Scott Benner 47:45
Code. I know. I know. That doesn't make sense to a lot of people. But code 18 for code 16 strips in the old PDM perfect for Arden was the way to go. You know what's interesting here, here I have three people in a row who I know are not old school diabetes people but been added a long time right people whose comments that I'll pay attention to when I see them roll by Jen, a big note of calibration, Shawn, personally, I would never use the G six without calibrating. And then the third person reads as we calibrate if readings are off by more than 20%. But it doesn't happen that often. These are three people whose opinion I think are probably pretty good. And they said three different things.
Jennifer Smith, CDE 48:26
And they all do it differently. And I think it's also kind of as I commented earlier about mice a good number of my sensors like just being done on day eight. I think it goes back to the the truth in that the sensor filament interacts with everybody's body system, body tissue, interstitial fluid, whatever you're going to call it a bit differently. I think that's the reason some sensor systems work beautifully for some people, and not so beautiful for others. I've got friends who love their Medtronic sensors get really awesome accuracy finger stick CGM. It's always on they don't have any problems with their systems. I could not get that thing to work for me. For the life of me and I wore both my sensors I wore Medtronic and Dexcom and it just
Scott Benner 49:18
never want to work. Good. But you know, here's another name that I Kristen who I know. And she says I've never calibrated I do not believe my blood. Here's why. I do not believe my blood glucose meter to be more accurate than my dexcom. So she just doesn't have probably Chica confidence in her meter. And some people don't think about that. They're just like, yeah, I checked it. So the meter the meter is like God, you know, the meter said so the meters right? Well, you know, some of those meters. If you've seen the testing, I brought it up recently on an episode. There's I think the last one was like 2018, right and it kind of ranked them only like six meters even ranked in like I would use this. If I was You all the other ones were like, Don't buy this meter.
Jennifer Smith, CDE 50:03
Right? The variance was way off. Yeah,
Scott Benner 50:05
right. Well, okay, we're out of time, aren't we? Because we're also at the end of the list. I only had an hour today. So I actually got down to the list. There's people's I'm sorry, I skipped some that obviously were repetitive. But yeah, like Jenny said in the middle, I think that what works for you is important that checking with a quality meter is important. And it seems that you know, the consensus seems to be if you're going to calibrate, make sure you're hydrated at a stable blood sugar before exercise, no active insulin, that kind of stuff. So the thing has a chance to, clearly,
Jennifer Smith, CDE 50:44
correctly from the beginning.
Scott Benner 50:46
Yeah, that's it. I wonder if we'll get yelled at about this? I don't think so. I think we were very clear.
Jennifer Smith, CDE 50:51
Yeah, I don't think I mean, it's not like we're saying, This is what you should definitely be doing. 100% to make. I mean, that's not this is not medical advice. This is just discussion. Jennifer,
Scott Benner 51:01
this is a woke culture. Okay, if you say something out loud that somebody doesn't agree with. You're trying to ruin the world. Don't you understand?
Jennifer Smith, CDE 51:08
I do understand.
Scott Benner 51:10
All right. Listen, I want to wish you a lot of luck changing your light bulb. And I really wish I knew your husband, because I would go behind your back and tell him that you don't change the look.
Jennifer Smith, CDE 51:20
Like I will, he will laugh at me. He'll be like who don't you see this little like thing on the side? This is very, like, pull it off. And so I'm like, scouring.
Scott Benner 51:28
Well, listen, I'm gonna help you for a little bit before you go. He's get up on a ladder and look around the ridge at the ceiling to see if there's little set screws that are holding the whole thing or not. No, that's good.
Jennifer Smith, CDE 51:39
There are no screws, there's nothing.
Scott Benner 51:41
So then it's got to be. Did you twist it for? I don't want you to twist it out of the ceiling.
Jennifer Smith, CDE 51:47
Yeah, I twisted the glass part of it, which is would be the next option. Because I've seen the glass bulbs that just twist off, right? This one is either really screwed in unbelievably tight, which I guess might be the case. Or maybe I'm just too worried to try to unscrew it or like, heavier because I don't want it to crack in my hand.
Scott Benner 52:06
Here are my two thoughts. When you're trying to turn it is the base the metal base turning with it? No. Okay. So maybe you have I don't think you have to turn the base. But what I am thinking is, is it possible that it's a reverse thread?
Jennifer Smith, CDE 52:22
Oh, counterclockwise.
Scott Benner 52:23
If you have to turn it the other way opposite. I wish you had enough time I would like to make you go up right now and turn it and see if it comes off. But instead I will just wait for your text message later. And
Jennifer Smith, CDE 52:32
I will let you know whether I required help to change the light bulb or not. I hundred
Scott Benner 52:37
percent agree you shouldn't tell anybody about this. That's all. Thanks. Yeah. All right. Well, thanks for doing this. I really appreciate it. Yeah,
Unknown Speaker 52:44
absolutely. Have a good weekend. Bye. Okay, bye.
Scott Benner 52:48
Hey, everybody, Jenny's gone. I'm still here. We're going to do everybody's favorite podcast thing I'm going to read to you for a second this is from dexcom.com. In their frequently asked questions. The question is, is my dexcom sensor accurate heading Dexcom g six continuous glucose monitoring system reading and meter value. Whether you're new to Dexcom, or experience, Review Product instructions before using the Dexcom g six. Keep using your blood glucose meter to make treatment decisions until you know how Dexcom works for you. Your meter gives you one number if you test twice, using the same or even different meter, it gives you another number and your Dexcom g six gives you a third. What do you do with all those numbers? Next heading is the test. The test your doctor does is considered a more accurate glucose number than any products you use at home. Both meters and Dexcom g six are compared to that doctors test to measure accuracy in clinical studies. They aren't compared to each other. Because of this, the dexcom g sex reading and meter value are unlikely to be exactly the same number, but they should be close. Compare the meter and your Dexcom g six to see how closely the numbers match each other. If your G six reading and meter value are within what we call the 20 rule, also known as the 20% 20 rule. They match closely. Here's the rule. To use the 20 rule follow the steps using the table below my gosh there's a table lookup your meter value in the green middle column. The left g six column shows the low range for G six reading that okay, you're gonna have to go look at this yourself. I'll put a link in the show notes for this 2020 rule goes on to talk about good fingerstick practices. When you're using your meter. Make sure your test strips are stored as directed and not expired. Your hands are clean for finger sticks. Wash your hands thoroughly with soap and water, not hand gel and dry them then test. There are times when the numbers temporarily don't match, but are likely to become closer over time. For example, the sensors first day with newly inserted sensors the difference between your meter value and Your g six reading may be greater. Generally the match gets closer over the first 24 hours. Glucose changes quickly. When your glucose is changing quickly, it is more difficult to compare numbers. The meter and Dexcom g six measure glucose from different sources. They are blood and interstitial fluid and blood glucose changes a little before interstitial fluid. The match gets closer and easier to compare. When your glucose stabilizes pressure on the sensor. When something is pressing on your sensor, it can affect your G six readings, the match should get closer after the pressure is relieved. That of course is what people call a compression low. So everything they're saying here matches pretty much everything that we found. Talking to Jenny, you know my experiences and what everybody in the Facebook page was saying. To determine what to do watch your G six readings over several hours. If the readings are always higher or always lower than your meter values, and always outside of the 20 rule, consider calibrating. Also consider calibrating if your Dexcom g six meter numbers don't match and your expectations or symptoms fit the meter value, not the G six reading calibration. calibrating your G six with your meter is never required. It can make the dexcom g six more accurate or less accurate compared to lab results, but it should bring the G six reading closer to the meter. When calibrating make sure you enter the calibration within five minutes of taking the finger stick. You don't calibrate during a sensor error. If you like you can calculate the 20 rule on your own. The dexcom g six reading must be within 20% of the meter value when the meter value is 80 mg dl or higher 20 mg dl of the meter value when the meter value is under 80. Please note that the information listed here is applicable to the dexcom CGM user within the US only. I cannot just read you this link. Because it is it looks very maybe I can hold on one second. So it's dexcom.com forward slash FAQ s forward slash is dash my dash Dexcom dash sensor dash accurate. Like I said I'll put a link in the show notes.
Huge thanks to the Contour Next One blood glucose meter for sponsoring this episode. Go to Contour Next one.com Ford slash juice box to learn more. And thanks to touch by type one.org for being such a wonderful long term friend of the show. Check them out touched by type one.org. Of course if you'd like to get a dexcom CGM dexcom.com forward slash juice box you can get a free no obligation demo of the Omni pod tubeless insulin pump that my Omni pod.com forward slash juice box take the survey at T one d exchange.org forward slash juice box guys ready to hear Jenny admitted not being able to do something that I think she's kind of embarrassed about and some other chitter chatter if you're looking for bonus material, I got you covered.
Jennifer Smith, CDE 58:18
I'm fed children I've gotten them changed I've wiped but
Scott Benner 58:23
I had
Jennifer Smith, CDE 58:25
washed my hands and then I picked my tomato isn't hi peppers from my garden and chili was how did you get up?
Scott Benner 58:32
Six o'clock. Oh, so last night.
Jennifer Smith, CDE 58:35
That was seven o'clock your time.
Scott Benner 58:38
Last night. Last night as Arden's pump was winding down. I was like it'll make it overnight, then her and her CGM me, right. And we change your CGM around seven o'clock it was done. It lasted the entire you know 10 days. It was working great right when I shut off and we hit like a little bit of a bleeder I was like God that'll probably be okay. So it comes on in two hours. And Ardennes. CGM starts are all exactly the same. It comes on nosorh blood sugar perfectly. And within an hour tells me she's low when she's not. And then we we coax it along and get it going and it's fine. So this happens. Around midnight I go to sleep. And at 2am Kelly wakes me up and she goes, Hey, I need help we changed Arden's pump, because our blood sugar was going up. And her CGM has lost its signal. And I was like, Okay, no problem. I'll take care of it. You go back to sleep. And I did take care of it, Jenny. And then I went back to sleep at 6am I was up for four hours in the middle of the night. And no and it just It would come back and it would go away and it would come back and it would go away. But I'm, I know, it's gonna be all right. And if this would have happened in the middle of the day, I want to be clear that this doesn't happen often. Does it just happen this time at a really bad time? But since it did happen, I know what I want to talk about today.
Jennifer Smith, CDE 1:00:18
Oh, great. And while we're waiting that I'm going to actually I've got like, I have so many chords. What's going on? What is the deal with chords? Right? The room
Scott Benner 1:00:29
is cleaned up, though. It's different.
Jennifer Smith, CDE 1:00:32
Oh, oh, because we are putting in new floors. Oh, this room. Okay, this. This is the bigger of, they put in new floors in our living room. They're like, we are purging our home of carpet.
Scott Benner 1:00:47
Okay,
Unknown Speaker 1:00:48
blah.
Jennifer Smith, CDE 1:00:50
So living room got done. Now we're moving on to the space that has been my office which interestingly has been, it's the bigger of the two bedrooms, right. Okay.
Unknown Speaker 1:01:03
And
Jennifer Smith, CDE 1:01:04
we're going to put new floors in here. And then we're going to put new floors in what is now the room that the boys technically share. Okay, we're gonna then transition rooms. I'm gonna take that room, which is actually the smaller they're gonna we're gonna move their stuff in this room and this is the bigger of soap.
Scott Benner 1:01:24
You're under. Well, listen, we are on stop. It's amazing. I know. There's nothing like being an adult is there? We just ordered a floor for Arden's room. And she very Arden just picked this floor that wasn't very expensive. So we were like, okay, yeah, you can have she's like, Can I do this? And when she picked that one, we're like, yes, you can. And you absolutely can. But we're replacing we. It's funny, you said this we wanted to replace, we've hardwood through most of our house. So kids bedrooms, and this room, amen. Is carpeted. And then our living room is carpeted. But everything else has Tyler or wood. And we wanted to make the living room, tile or wood or something. We weren't really sure what. Because the one one of the bonehead mistakes we made when we put the house together was we bought this carpeting and didn't realize and dog owners will know right away, you don't buy looped carpeting with a dog right. And we didn't know that our carpet cats or I think the over under on poles that I fixed in that carpet have to be in the thousands, you know, or sometimes the dog's leash or something gets called on a runs away and just Yanks out like six inches of carpet and I actually get back down on my hands and knees with a hot glue gun and toothpicks and put each one back in again. Right. Hi, God,
Jennifer Smith, CDE 1:02:51
you have so much more time than me. Oh my god.
Scott Benner 1:02:55
The other option was the other option would have been to burn the house down. It was like right in the middle of the room. You know, like I said, we got to get out of here. It was just really bad. And so we can't afford to put wood down or what we wanted to put down in there right now. So we just went out and bought like a really inexpensive piece of carpet and it's being delivered in a couple of days. I can't believe we're doing flooring at the same time
Jennifer Smith, CDE 1:03:16
at same time. Yeah, I don't think I've ever seen the floor in that room. Usually there's like a nice couch behind you. And that's all I see besides like,
Scott Benner 1:03:25
Yeah, well my son stole the couch, just so you know. So that's gone now. He's like, I'm gonna take this sofa into my room because and he's home forever. So we're like, Alright, he's, you know, my gonna take the couch, you know? He's got that. And I have all of Arden's junk in here because we're waiting for the flooring to be put in her room. So it's a bit of a disaster. Anyway,
Jennifer Smith, CDE 1:03:47
but I was gonna say I'm gonna get yet another core do totally
forgot to plug the cord for the computer like Direct Connect in so give me a sec.
Scott Benner 1:03:55
Yeah, sure.
I make Jenny plug her I don't let her use Wi Fi while we're doing this. She's dragging an ethernet cable across.
Jennifer Smith, CDE 1:04:10
Oh, and I also realized that I I have no clue how to change the lights.
Scott Benner 1:04:17
What do you want to change in there? What do you mean what
Unknown Speaker 1:04:19
I
Jennifer Smith, CDE 1:04:20
want light bulbs in the ceiling died. You don't i
don't i cannot figure out how to
get like you talking about let me say I don't know how to get it off. I have no idea is there
Scott Benner 1:04:35
no screw in the middle of it.
Jennifer Smith, CDE 1:04:37
There's no screws. I've tried to turn in the glass.
It doesn't unscrew. I don't know what to do. So I have a big ol like floor lamp in here now so that I actually have Why have you
Scott Benner 1:04:53
brought anyone else into? Try to figure it out?
Jennifer Smith, CDE 1:04:58
No. I should If I knew I should ask my husband, do you
Scott Benner 1:05:02
not want to tell your husband? You can't figure out how to change the light bulbs, right?
Jennifer Smith, CDE 1:05:08
Like, I'm not this dumb, like, I don't know what the deal is. Oh,
Scott Benner 1:05:12
you're not wrong. It's is it glass? It's a dome, right?
Jennifer Smith, CDE 1:05:16
And it's glass. Right? So it's
like the wrong move. Like, I just I think I also need to get like a taller.
Scott Benner 1:05:23
Are you reaching? Yes. Yeah.
Jennifer Smith, CDE 1:05:25
Because I've got just the basic Let's switch. This stool has worked fine for all of the other like ceiling things. Right.
Scott Benner 1:05:31
So why wouldn't it work for this? How long has the light bulb in that light been working for you? This is the first time you try to change
Jennifer Smith, CDE 1:05:39
it is we moved in.
It'll be October 1 will be two years in this house. And we've not changed the light bulbs in this light. It's obvious.
Scott Benner 1:05:52
That's good. Wrong. I'm doing all right.
Jennifer Smith, CDE 1:05:54
Good lights, I guess you know, but also don't get used that very that often. And because I'm really on this in this room during the daytime. Okay, and so unless it's really dark in here, I typically don't usually use them. But anyway,
Scott Benner 1:06:13
yeah, cool. All right. Listen, let's try to bring your yes your bring your microphone a little closer. Do
Jennifer Smith, CDE 1:06:18
no sir to me. Is that better? Try get
better. Yes. That's okay. There's this guy.
Scott Benner 1:06:25
It's been. So hopefully we've answered some of your questions today about how to calibrate or not calibrate your Dexcom g six and the other burning question. How many people does it take to change a light bulb in Jenny's house? As of now we know the answer to be more than one. If Jenny's involved and it's in her office. Thanks so much for listening to the Juicebox Podcast. Please take the time to share the show with a friend and leave a wonderful five star review on Apple podcasts. If you're so inclined.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!