#1292 Keep Taking Showers
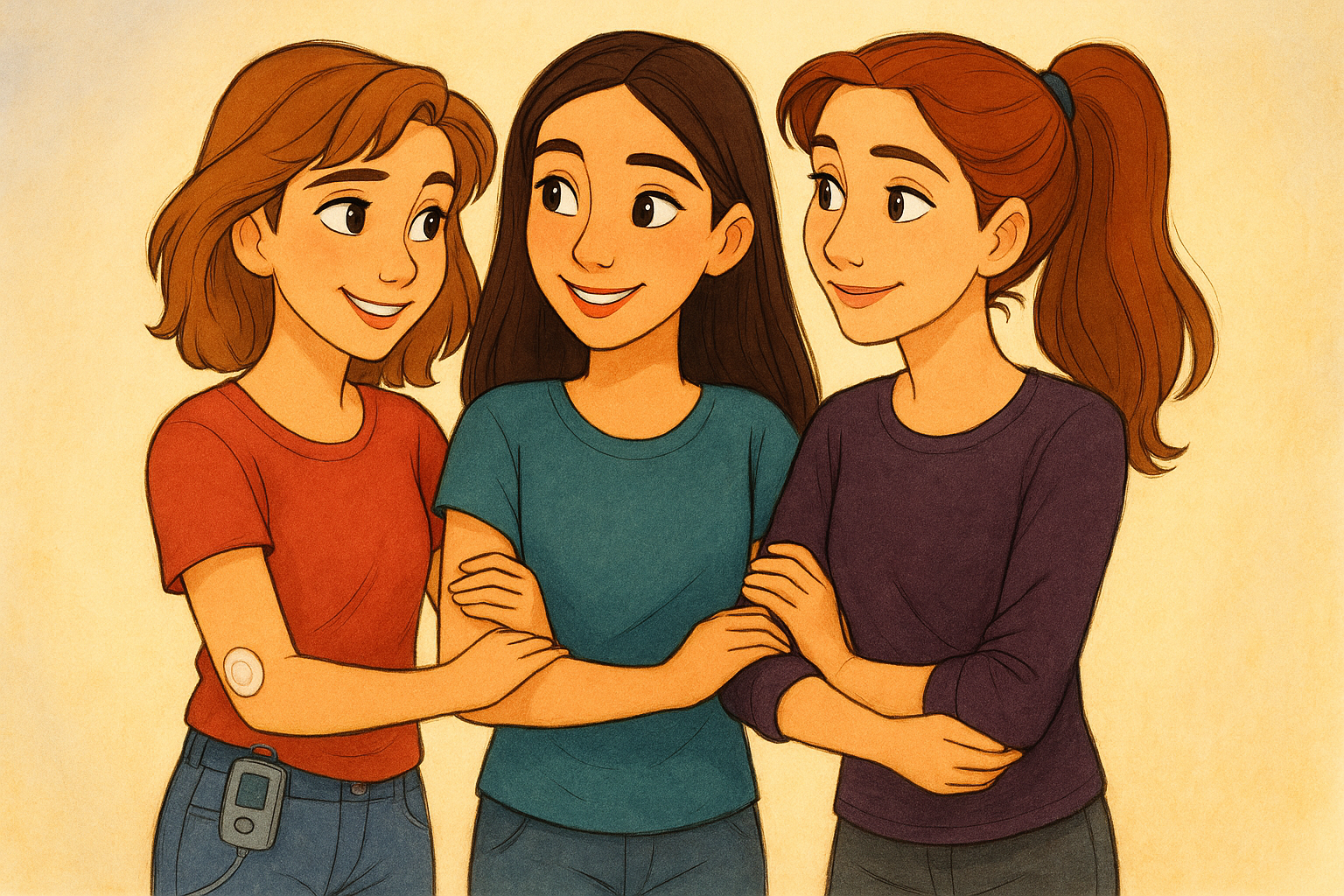
Jason, his sons, his sister and his father have type 1 diabetes. We talked about hospice care.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - iHeart Radio - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends. The hell was that? Hello friends, and welcome to another episode of The juicebox podcast. I gotta find out what that was. Hold on. I just listened back and realized that you couldn't hear that. So now you're wondering what's wrong with me. But trust me, there was a noise.
Unknown Speaker 0:22
You today
Scott Benner 0:24
I'm going to be speaking with Jason. Now. Jason has type one diabetes. He got it when he was 18. He's now 45 his son Wesley is 12, has type one diabetes since he was two. His son Cooper is 10, diagnosed 11 months old. And his daughter, who is six, well, she currently doesn't have type one diabetes, but there's other people, and we're gonna find out all about it. Please don't forget that nothing you hear on the juicebox podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin when you place your first order for AG, one, with my link, you'll get five free travel packs and a free year supply of vitamin D drink. AG, one.com/juice box. Don't forget to save 40% off of your entire order at cozy earth.com All you have to do is use the offer code juice box at checkout. That's juicebox at checkout to save 40% at cozy earth.com I know that Facebook has a bad reputation, but please give the private Facebook group for the juicebox podcast, a healthy once over juicebox podcast type one diabetes. The group now has 47,000 members in it again. Did you know if just one person in your family has type one diabetes, you are up to 15 times more likely to get it too. So screen it like you mean it one blood test can spot type one diabetes early. Tap now talk to a doctor or visit screen for type one.com for more info. Having an easy to use an accurate blood glucose meter is just one click away. Contour next.com/juicebox That's right. Today's episode is sponsored by the contour next gen blood glucose meter. This episode of The juicebox podcast is sponsored by the ever since CGM, and sure all CGM systems use Transcutaneous sensors that are inserted into the skin and last seven to 14 days, but the ever since, sensor is inserted completely under the skin, lasting six months, ever since, cgm.com/juicebox,
Speaker 1 2:35
I'm Jason. Live in the middle of Iowa, and I'm type one. I'm diabetic. I have two children that are also type one diabetic, and I believe today that Dave and I are going to be talking about my dad, who was also type one diabetic.
Scott Benner 2:50
You want to tell people why you called me, Dave,
Speaker 1 2:53
why I called you? Dave? Well, apparently there was some review of your podcast that referred to as Dave, which is telling you how much they pay attention to the actual content they're listening to.
Scott Benner 3:02
It was a really great review about how fantastic the podcast was and how great I was, and then called me Dave. And I was like, I love that. I it could have been a typo. It could be that this person believes My name is Dave. I don't care. You know, I am maybe one of the few smaller podcasters who don't come on and go, Hello everybody. I'm your host. You know what I mean? And then my name and like, I don't do that because I think, I mean, if you want to really know why, I think it makes you sound like you're small time, right? Yeah, I don't turn on the television and not know who somebody is I'm looking at. I don't need to be introduced to them. I know sometimes, like in older media, a host will come onto a TV show and be like, you know, Hello, welcome to the show. I'm David Letterman, like that kind of thing, but that's just, to me, an old idea. So like, moving forward, they're a huge podcast. I've never once turned one on and been like, hey everybody. My name's Billy, I'm the host today. And I'm like, Okay, if they don't know, they'll figure it out, and if they don't figure it out, they're not listening to you. So anyway, maybe I was wrong, just in case that guy's listening Hey everyone, this is the juicebox podcast, and I'm your host, Scott Benner, not Dave. Oh, hey, Scott. Hey. What's up? Dave, how many people right now do you think we're like, oh, Scott, or is it just him?
Unknown Speaker 4:26
I thought this was Dave, yeah.
Scott Benner 4:27
Well, now on the Facebook group, if you or a couple of other intrepid people call me Dave, then it causes then people are like, that's not Dave. And I'm like, Uh oh, this is gonna go on forever.
Speaker 1 4:37
It get it gets engagement though. It gets engagement though. So people ask them questions.
Scott Benner 4:41
We're feeding that algorithm. That's right, Jason, we're feeding the algorithm making it do something I actually that's a whole job that, yeah, I wouldn't want to take the time and to be boring and explain to people, but getting a Facebook group to serve the people who were in it well is a lot about making sure contour. Conversations are happening. And, you know, every once in a while somebody will ask a question, and it's kind of like a, maybe a, I don't know, a beginner question, and somebody will rush in and go, that question has been asked 50 times, and just search the group. And I every time I'm like, no, no, no, bad not don't just search the group ask the question, because if you start searching the group and shooting the group like it's an encyclopedia, the group will die like the algorithm needs to see people asking questions and answering questions, and it's more human, and I think leads to people understanding things a little quicker. So let's start with you. How old were you when you were diagnosed?
Speaker 1 5:40
I was 18. I just turned 18. It was in October, and actually voted for President for the very first time from my hospital bed.
Scott Benner 5:50
Who'd you vote for? You don't tell me that it was Bill Clinton at that time. Okay. How old are you now? 45 that's insane, isn't it? Yeah, time is terrible. Oh my god, okay, let's run through it. You have two kids.
Speaker 1 6:08
I have three kids total, three. Two of them have type one. How old are they? Our oldest is 12 years old, and he was diagnosed at two and a half years old. And our middle boy, who just turned 10, he was diagnosed at 11 months old. Wow. And our daughter, she is six years old,
Scott Benner 6:28
and you're worried because she hasn't reached 10 or 12
Speaker 1 6:32
yet? Yeah, yeah, she's, she's made it so far, so it's, uh, thankfully, she hasn't shown any signs yet. But we're, we're prepared, yeah? Well, I
Scott Benner 6:40
mean, you'd have to be this point. I mean, if you don't have enough experience to handle it, then who does right, you know?
Speaker 1 6:47
And then your father, type, yeah, yeah. You know, when he was diagnosed, he was diagnosed around three years old. Oh, wow, yeah. So that was back in the stone ages. So
Scott Benner 7:01
you're the one that really pushed the envelope, as far as you all go, making it to 18. Okay, so he was three, yeah,
Speaker 1 7:11
and, you know, just, just to tack on to that, my sister, who is a couple years younger than me, she's also type one. Oh, okay, yeah, how
Scott Benner 7:21
old when she was diagnosed? You remember she, I think was just 14 or 15. Okay, beat her easy. Okay, no, wow. Do you have other brothers and sisters? No, just one sister. Okay, how about other autoimmune stuff? No,
Speaker 1 7:39
I know you're gonna say, but you know, did you No, I don't think there is. You don't think
Scott Benner 7:44
there just is. It's just type one diabetes. You guys are what they call hyper focused. Yes, okay, wow, when you have type one and your sister has type one and your father has type one, when you are getting ready to have a family, what runs through your head about the possibility of diabetes in children? This episode of The juicebox podcast is sponsored by ever since, and ever since is the implantable CGM that lasts six months, ever since. Cgm.com/juicebox cgm.com/juicebox, have you ever been running out the door and knocked your CGM off, or had somewhere to be and realized that your adhesive was about to fall off? That won't happen with ever since, ever since. Won't get sweaty and slide off. It won't bang into a door jam, and it lasts six months, not just a couple days or a week. The ever since CGM has a silicon based adhesive forged transmitter, which you change every day. So it's not one of those super sticky things that's designed to stay on you forever and ever, even though we know they don't work sometimes, but that's not the point, because it's not that kind of adhesive. You shouldn't see any skin irritations. So if you've had skin irritations with other products, maybe you should try ever since, unique, implantable and accurate. So if you're tired of dealing with things falling off or being too sticky or not sticky enough, or not staying on for the life of the sensor you probably want to check out ever since, ever since, cgm.com/juice box. Links in the show notes. Links at juicebox podcast.com, contour, next.com/juice box. That's the link you'll use to find out more about the contour. Next Gen blood glucose meter. When you get there, there's a little bit at the top. You can click right on blood glucose monitoring. I'll do it with you. Go to meters, click on any of the meters. I'll click on the Next Gen, and you're going to get more information. It's easy to use and highly accurate. Smart light provides a simple understanding of your blood glucose levels. And of course, with Second Chance sampling technology, you can save money with. Fewer wasted test strips. As if all that wasn't enough, the contour next gen also has a compatible app for an easy way to share and see your blood glucose results. Contour next.com/juicebox and if you scroll down at that link, you're going to see things like a Buy Now button. You could register your meter after you purchase it. Or what is this? Download a coupon, oh, receive a free contour next gen blood glucose meter. Do tell contour next.com/juicebox head over there. Now get the same accurate and reliable meter that we use. Well at that point in time. You know, I
Speaker 1 10:42
mentioned it to my endocrinologist a few times, and they always said, you know, it's a very low percentage chance of that happening, so I really didn't give any thought to it. And I don't think it, I don't think it would have changed my mind at all. It wasn't a surprise when it happened, but it still hurt, you know, hurt a lot, yeah, I bet two years old, right? Yeah, two two years old, 11 months old. So, yeah,
Scott Benner 11:05
yeah. Arden was just two years old, and I recall it feeling like the promise of my life was revoked. If that makes right, you know what I mean? Because we were a young family, and things were, I mean, we weren't like, killing it or anything, but it was going well, and you could see that we were moving in the direction we intended. We had bought a very small house recently, and I was like, oh, you know, I grew up renting my whole life, and it's like, wow, we're like, we're doing it. You know what? I mean, like, we're getting out of the hole that somebody started us off in, and then that happened, and it felt like it felt like the hole we were in got thrown into a different hole, you know. So how about your wife? Do you think she ever even considered it?
Speaker 1 11:55
I don't think so. I don't think she thought about it at all like it wasn't on her radar. I think part of that's because I've been fairly well managed my entire life. So she only saw a few lows here and there, and didn't really, you know, partake in any of my care for it, because, you know, I'm an adult guy, and I can, I can do it myself. So
Scott Benner 12:13
do you have any hindsight on that? Should you have made her more aware of it?
Speaker 1 12:18
I think so. I think in general, people should do that more often. I think it's important for people to more understand, I think what's wrong with your significant other. You have any idea why you didn't? No, I talked to my mom about this recently and asked her about that, and she she said, I think it's just a guy thing, but I'm not even sure it's just a guy thing. I think it's people in general, because, you know, people are just worried about showing a weakness, yeah, and especially weakness like type one diabetes, where it's not visible most of the time,
Scott Benner 12:51
yeah, it's not, like, the it's sort of the invisible stuff, right? Like, yeah, like, that's why I think anxiety or mental illness is even harder to talk about, because you're like, there's an unseen thing that just tackles me, and I don't hear it coming, and I don't know how to get out of the way of it. And, you know, just once in a while, randomly, my blood sugar might get really low, and right, I could get into a situation where there's nothing I could do about it, and now I'm like, left open to hope that the world around me helps me and gets me back here again, exactly. Yeah, it's tough. Your father not share it with your mother. She
Speaker 1 13:27
did not really partake in any of his care, either, and he was very, very, very private about it. I would say so much so that my sister and I really had no clue or weren't very knowledgeable about how to treat him if he was low. We'd only seen it happen a few times, because he was fine most of the time. And I remember one time, you know, I got home from school probably early teens, you know, sitting on in my bedroom, Dorking around, and I hear my dad's truck pull up in the driveway, and I hear kind of a crash outside. I get up out of my bed, and then he comes stumbling through the door, you know, pale, sweating, shaking. I ran to the bathroom where the glucose tablets were at, and I grabbed one glucose tablet and took it out to him and made him eat it, and then like nothing was happening. So I poured him a glass of water and just dumped a bunch of sugar into it, and he drank that, and eventually he came around. But you know, that's all I knew how to do at that point in time. And it wasn't like somebody came to me and said, Hey, if he's low, do
Scott Benner 14:34
this right. It was more of just
Speaker 1 14:39
do what I thought was right, even though it wasn't enough at that point in time. And you were in your teens at that point, yeah, probably 12 or 13. It's a long time to live with somebody and not understand fundamentally what turns them back on. You
Scott Benner 14:52
know what I mean Exactly? Yeah, look at you, and you figured it out, though, right? Yeah,
Unknown Speaker 14:57
we figured it out. Yeah. Did
Scott Benner 14:58
that get you a puppy? An ambulance that day. Yeah, if you had a puppy out of that or anything, you remember,
Speaker 1 15:03
no, but, you know, I would say that my dad and I's relationship wasn't always incredibly close. And you know, he's not a a guy that's going to come out and say, Hey, I love you. He would say it in other ways, but after he kind of recovered from that low I had went back in my bedroom and I was like, crying, you know, sitting there because I was scared to death, yeah, and he actually came in and gave me a hug at that point in time. And that was, it's something that really sticks out in my mind. Like having a care when somebody needs you, kind of important. Well,
Scott Benner 15:36
you, I guess you learn that being there for somebody is a way to get life is the way to get love from them, right? Yeah, it's because. It's what other ways did you do? You think you were performing as a child that did not result in a hug?
Unknown Speaker 15:52
I don't quite understand what you're asking.
Scott Benner 15:54
I guess the question is, is like, did you do you? Can you look back and see that you tried other things? Did you try being good at sports and thought that that would make him say, I love you and give you a hug. Did you keep the house really clean? Did you like, were there other things you were doing that didn't result in a hug? Plenty, all of them. Yeah, all of them.
Speaker 1 16:12
No, it's, it's, I don't think I was a terrible kid, and I always kind of tried to take interest in things that he may have been doing, whether it be working on this truck out in the garage or working with him during summers. He owned his own business too, and would go work with them. My sister and I would he treated us well when we're out there, you know, paid us free lunch and gave us food and stuff that we wanted. But it wasn't like, oh, yeah, thanks. This is a enjoyable time. I really enjoyed spending time with you. It was on to the next job.
Scott Benner 16:42
Do you do that as a father? Do you tell your kids that you enjoyed spending time with them? I
Speaker 1 16:48
try not to do things that happened with my relationship with my dad, so I try to spend time with my kids. I try to instill that I love them all the time, give them hugs all the time, and I'm there, I'm the primary type one caregiver in our house, so we have a lot of connection that way. And our daughter, she takes advantage of all this and always wants to go to the grocery store with me, because she'll know that I'll buy her a candy when we check out. So
Scott Benner 17:20
buddy, isn't it? Like, I just realized that you're talking like my son full knows that I love and care about him, and so if I said to him, like, I'm doing, I have a project this weekend, I was like, Hey, I'm gonna be working on something this weekend I can use your hands for. And he goes, I'm probably busy. And he wasn't. It wasn't shitty. It was just like, No, I'm alright. And I realized now, like, if he, if he was, like, running around, going, I hope that guy loves me, he'd be like, Yeah, Dad, I'll help but instead, he's like, No, thank you. I mean, you do see people manipulate people that way. You know what I mean and that. But that's not what your dad was doing. Your dad was just closed off. Yeah,
Speaker 1 17:57
and I think you know he was, he was 69 when he died, so he grew up on a farm, so it's all about work. That's just kind of his life revolved around. Was working? Yeah,
Scott Benner 18:09
I hear you like, Get up, do the thing. I did the thing. It means I love you, because I'm working hard for you. I didn't leave you, I didn't quit my job. I don't drink during the day, like I'm doing the things I'm supposed to do. It's weird that people can't see the whole picture. They just, they get focused on one, like, aspect of it, and like, I'm doing a good job with this. So right? That means I love you. And you know it, come on the other day I my son's back. Like, he left, he finished college, and he went worked a job for a whole year in another city. He was, like, across the country and gone. And then he said to us, like, I've gotten as much out of this job as I can. If I want to move up, I'm going to have to take a different job, you know, I want to come home and reorient myself and look for work again. And so we said, Fine. And he had saved, actually, very proud of him. He'd saved a bunch of money while he was working. And He came home, and he's home now, and it's, it's the end of March, he's been here for three months, and every day I see him educating himself and applying for work, and, you know, talking to people and making connections, and he's doing all the things he should be doing. And I think every day, God, I hope this kid has some success here, like, I don't want this to drag on for him, because, you know, it might get a little, you know, might get a little bit of a bummer after a while. And then my next thought is, I hope he doesn't get a job, because he'll leave. I just took a second yesterday and I said, Hey, I want you to know that every day I see you, I think, Oh, I hope this works out for Cole today. He's doing a good job. It's going to work out for him. It's coming. I'm sorry if he feels badly about it, I said, but man, my next thought is always, I hope you don't leave right? And like, we didn't hug or cry after that, there was no commercial. And then we came back to the Hallmark Channel and, like, talk some more. Like it was just, like, that was it. And he didn't say much, and we moved on. But I know he knows, yeah, and if he doesn't, Jason, I don't know what to do. You know what I mean? Like, I wouldn't know how to. Adjust it like I wonder if your dad thought
Unknown Speaker 20:01
he knows, and then you
Scott Benner 20:05
were over there going, I wish someone would talk to me about this once in a while. It's interesting. Do you ever talk to him about it? No,
Speaker 1 20:13
not really. He wasn't much of a much of a talker. You know, I kind of see that coming from his side of the family too. It's like my grandma is the same way and his dad was the same way. Really didn't talk about it. It was it's rare on that side of the family for somebody to say, Hey, I love you, and hey, come give me a hug. It's kind of weird now with our kids, my wife and I's kids, when we go see great grandma, my grandma, they always insist on giving her a hug, you know, before we leave and say goodbye. And it's, it's heartwarming to see that, and I can kind of see that tear in my grandma's eye whenever that happens,
Scott Benner 20:50
yeah, I wonder if she's thinking, this is what we should have been doing, yeah, yeah. That's, feels like it's too late, but it's not for her, right? She's getting a
Unknown Speaker 20:58
little bit of it, yeah. Okay, so
Scott Benner 21:02
why were you so well managed? If your father wasn't and also wasn't teaching you about diabetes,
Speaker 1 21:11
I think it came down to seeing him not treat himself well. There was a few times, like growing up, where he would have lows in the middle of the night, and the ambulance would come, I would know nothing of it, like no one told me about it, until many years later that you know, the ambulance came. Paramedics came and took him away because he was low and my mom couldn't help him. And after hearing like those stories, that kind of made me want to do better, because I knew it could be avoided with a little bit of effort. Yeah, and also, when my sister was diagnosed, she was diagnosed me, like a year before I was she struggled really hard with it too. That also kind of made me say, this is a my mom. I can't rely on my dad to do this. This is this is me. I have to do
Scott Benner 21:59
it. So you did your sister figure it out? Uh, she wasn't
Speaker 1 22:05
nearly as bad as my dad was with it, but she definitely struggled. She struggled with burnout quite a bit, and she kind of saw the opposite of my dad, you know, she saw the lows or heard about the lows and didn't want to be low so she kind of rode, you know, 131 4150, a lot of the time.
Scott Benner 22:27
Is she having any trouble now?
Speaker 1 22:31
No, she's she's pretty healthy. I don't think she has any any side effects from type one at all. So when
Scott Benner 22:38
you were figuring it out for yourself. Did you ever go to her and say, like, did you try to trade war stories or tips and tricks, or did that not, was that not a thing you guys did together? That
Speaker 1 22:51
really wasn't a thing. I think the one thing I do remember she got moved over to Humalog before I did, you know before that, it was regular, NPH, and when she got moving over to human log, she told me, Oh, this is, this is great. Like, you know, you can actually take it at 15 minutes before you eat. And so then that was, like, the one thing, that tip that she gave me that I actually followed and moved on and enjoyed it, you know, I liked that part. But other than that, we didn't, we didn't
Scott Benner 23:20
really talk about it. Were you close in other ways or not particularly,
Unknown Speaker 23:24
not particularly, yeah,
Scott Benner 23:26
just the girl boy thing, yeah, I
Unknown Speaker 23:28
think so yeah.
Scott Benner 23:29
Did that change as you were adults?
Speaker 1 23:31
I'd say it did not change much until our two boys were diagnosed. Okay,
Scott Benner 23:38
then she fell and then comp, then
Unknown Speaker 23:41
it changed. Yeah,
Scott Benner 23:42
does she have children?
Unknown Speaker 23:45
No, she doesn't. Okay, not biological.
Scott Benner 23:48
Do you so what do you think happened inside of her when she saw your children get diagnosed? I
Speaker 1 23:53
think she saw, you know they were so young when it happened. And you know she loves them dearly. So when she sees something that she struggles with, happened to them. I think it kind of opened up that door. Do
Scott Benner 24:05
you think people realize that when their siblings show affection to your children, like when your siblings show affection to your children, that it's probably the affection they have for you, but it doesn't come out because you grow up together,
Speaker 1 24:20
you would agree with that, yeah, for sure. Really something.
Scott Benner 24:24
And if you are very affectionate, you don't feel like you have to get it out some other way. So interesting, right? Hey, cultural, religious, not cold this. But where does the way that your family interacted? Where does that come from? Do you
Speaker 1 24:40
think? I don't think it's cultural, I don't think it's religious. Why it happens that way? I really kind of attribute it to just our family histories. Like neither side of the family is very, very much out there saying things like, you know, hey, I really appreciate you. I love you. It's more on my. Mom's side. It was a lot of getting people, joking around with people, and my dad's side was very, very, don't say I love you. Get the work done. What were their backgrounds? What do you mean by background?
Scott Benner 25:15
Irish, German.
Speaker 1 25:16
There's a bit of Irish in there. Last name is wierman, so you know, it's about as German as you get. I think that's Irish, and German is incredibly interesting.
Scott Benner 25:26
My mom's parents were German, and you're describing them, you know what I mean? Right? It's interesting. Okay, all right, I got it. Well, how do you manage today? And is that different than how you manage before your kids got type one?
Speaker 1 25:43
It definitely is. Today I am using loop. Both boys are using loop, and we're using human logging those in those pods, using Dexcom g6 that all happened because of the boys when Wesley was first diagnosed. He's our oldest boy. I was still MDI and using human log. And Atlantis, the human log was in a pen, of course. And when Wesley was first diagnosed, 10 years ago,
Scott Benner 26:15
yep, you know, I don't think Dexcom was really a thing. Then, was it a thing 10 years ago? 10 years ago. Arden is 10. She had one then, yeah, you just didn't know about it yet. She
Unknown Speaker 26:28
four, maybe. Yeah, I
Scott Benner 26:30
don't that. I don't remember which one it was, but it existed, yeah, and you were MDI till you were 35 Yep. Okay. And doing well, or just, okay,
Speaker 1 26:42
um, a one Cs were right around six most of my life. Yeah, that's good. And I don't think a lot of that was, there was definitely a roller coasters, like it was, it was probably a roller coaster ride up until I got the Dexcom. Okay,
Scott Benner 26:58
you were always like, chopping down highs and stopping lows. Yeah, so your standard deviation probably was off, but you weren't tracking that right. Yeah, couldn't see it, yeah. How do you see it? Interesting, and doctors told you you were doing great. There was no ever
Speaker 1 27:13
a one. Cs were always good. And blood sugars, you know, on paper, when you tested four times a day, looked good. Yeah,
Scott Benner 27:24
if you test at the right time, everybody, you just have to, just have to catch your blood sugar in the right spot. They have a right before, right before you eat, yeah, yeah, yeah. When you're when your blood sugar is falling because you're hungry and and you've used too much insulin at the last meal, and you test and you're like, Oh, I'm 89 I'm really doing great at this, not really thinking if I didn't eat now, I'd be 60 soon. Yeah. What a flawed system. Okay, so what happens, man, when they're diagnosed, do you just go, this isn't good enough for them, or, like, what makes you dive in and and get the rest of it?
Speaker 1 27:57
That's a really good question. I don't remember the exact epiphany moment, but it probably centered around seeing something on social media, and when we dove in, like with Wesley, like we dove in, it was as soon as I kind of figured out what the Dexcom was like, our doctor had mentioned it to us, but, you know, I had done many, many years MDI and just a tester and did fine stuff like, well, what is this technology like? Is it? It's nothing, right? But after seeing online, on social media, you know, seeing what the Dexcom could do, and then what I really saw was the Dexcom g4 attached to a cell phone and night scout and being able to see numbers remotely, I think that's what kind of made me dive in. Yeah. And then after that, it was like hardcore diving in.
Scott Benner 28:56
And so what does he start with? A pump, a CGM or how long was he MDI?
Speaker 1 29:02
He was MDI for maybe a year or so, year or two, okay? And a lot of that had to do with because he was using such little insulin, like none of the pumps OmniPod could not deliver, uh, insulin in small enough amounts at that point in time, right?
Scott Benner 29:19
And that's the same thing that happens to a lot of people. They're like, well, just do shots. Because meanwhile, the shots are, they do a unit at a time. And, you know, if you have half unit noodles and your kids small enough, that's still not enough or small enough. So it's interesting how we were
Speaker 1 29:34
doing, we're doing like you were doing, you know, seeing how much you could, like, pull back a quarter of a unit. Yeah, we did that for a long time. Had syringes that could do half units, and then ends that could do half units, okay,
Scott Benner 29:46
and then probably about the time you're figuring out a pump for Wesley, then your next son is diagnosed. Yeah,
Speaker 1 29:53
we had moved across the state, and I was still doing business, you know, in our Old Town. It's about two hour drive away. I was over there for a meeting. Wife had called me and said, uh, she had checked Cooper's uh finger, because he had went through his diaper the past couple of days, and that morning it was super heavy. And she said, Well, I checked his finger, and it was like, you know, 450 you know, at that point in time, my heart just dropped, and I said, you know, why don't you guys? I'll call my mom and I'll have her come over and pick you guys up and drive over to where I was at, because that's where our other boy had gone to, the endocrinologist at over university of Iowa Hospitals and Clinics, which is, you know, our best hospital in the state for type one. And said, Hey, drive over here. While you're driving over here, give him, like, a quarter a unit of insulin to bring him down. And that's what happened. He came over, and family came over, and we went through that hell all over again, yeah,
Scott Benner 30:56
so soon after the last time too. The thing is, Jason, that's not why you're on the show. I just wanted to get I just wanted to get your background so for everybody, so they knew who you were and what you're living through. But you really wanted to come on today to talk about something completely different. So why don't you express to everyone why you're here? Well, last year, which would be
Unknown Speaker 31:23
January, ish, 2023 my dad and mom. Type
Scott Benner 31:28
one diabetes can happen at any age. Are you at risk? Screen it like you mean it. Because if just one person in your family has type one, you're up to 15 times more likely to get it too. So screen it like you mean it. One blood test can help you spot it early, and the more you know, the more you can do. So don't wait. Talk to your doctor about screening tap now or visit screen for type one.com to get more info and screen it like you mean it.
Speaker 1 31:58
Both got covid. My mom was able to, you know, to kind of maintain she didn't have very bad symptoms. But my dad, because of his type one diabetes and his health history, because of type one diabetes, we should probably talk about that slightly here. I think most of his life, his a one Cs were, you know, 1011, 12, just because of poor management, yeah, and that had a significant impact on his his health. Like he was a healthy guy. If you looked at him, he's tough guy, skinny guy. He had quadruple bypass. And then probably 10 or 15 years after that, he had like four mini strokes, and everything kind of went downhill after that. And after the strokes, he kind of felt worthless, but didn't get around much, didn't try to rehab much, because, you know what? What good was he if he couldn't do work type of thing? What kind of work did he do? He was an electrician. He had his own electrical business, and then he also worked at a company that makes gigantic industrial valves. Okay? He was a hands on person that got down and dirty, right? And you describe him as robust,
Scott Benner 33:16
but with a one sees in double digits, exactly. Yeah. So it's funny as you're trying to talk about his physical characteristics and his health, what I really thought was, I wonder if he would have told you he loved you, if his blood sugar was lower, that very well could be, yeah, I wonder if he would have had more mental clarity and and and seen things differently.
Speaker 1 33:37
Very well could be. You know, kind of mention that, like, after he kind of switched from MDI the majority of his life over to OmniPod five, he seemed to take a lot more interest in type one, and he seemed to soften up a bit, and as a 1c, had dropped down to like, seven, yeah, plus
Scott Benner 33:58
he had something to focus on again, and a thing that he needed to be good at and learn and, you know, right work at. Yeah, it's interesting. Listen, there's a chameleon sitting behind me in a cage right now, because my kids grew up and I don't have anything to take care of. So I got very like, stir crazy very quickly, just trying to take care of all you guys wasn't quite enough for me. I was like, I needed something alive in front of me to, like, work on and study and and, you know, figure out what it needed. So, oh, all right, well, did that give you some time with him? I'm gonna say no. You know, my dad's
Speaker 1 34:35
the type of guy that would if you needed work done. He was there immediately. So we had an old house at that point in time, and he would come over frequently to kind of help me with things around the house and share His love with me that way. And even after he had a stroke, his first stroke, like we had a huge windstorm roll through town, and it like knocked over trees all over town, and our big tree and our. Backyard. It fell over, and he came over even, you know, suffering the consequences of a stroke where he can't move half his body very well with chainsaw. And we're, you know, chopping the tree apart and taking it down. And he was just trying to do his part, you know, trying to help me and the family. Yeah, wow. Well,
Scott Benner 35:21
I mean, listen, clearly he loved you. He just didn't, yeah, yeah. He just didn't say it the way you were hoping for, right? But look, look what it did for you. You're really open with your children and your family, I bet, with your wife too. And you know, don't worry, that'll slingshot the other way, and your boys will be quiet, strong men who won't say anything to anybody. You'll just bounce back and forth through all of eternity getting back to your dad's health. And really the reason you wanted to be here, you know, your note to me is very simple, just that, you know, talking about hospice care and type one diabetes and being older with type one was something you want to talk about, and I know we don't talk about it enough. So I'm very interested, what, what was the, you know, what was the course, what, what happened? So after, after, my
Speaker 1 36:11
dad was in the hospital with covid, he was there for the probably a week or so, and just was not getting better, and we didn't go see him. So I was just talking with my mom over the phone, because I didn't want to get covid. Yeah, my mom had said, you know, this is not looking good. You know, I'd call him every day, talk to my mom every day. And my dad really wasn't able to talk while he was in the hospital doing this. He had his OmniPod five on. He's working great. And my mom said, you know, he's not eating much, and he's got a super flat line, and it's like at 100 all day long, all night like, well, that's great, but we need him to eat. You know, kept saying we as soon as you can, you gotta probably get over here and after his, after his 10 days of being quarantined, my wife and kids and I went over there and saw him, and he's just kind of laying there, kind of comatose, not really knowing what's happening. He'd look at us every now and then, but quickly, you know, close his eyes and just go back to sleep.
Scott Benner 37:10
The hospital staff, because
Speaker 1 37:11
he was on his OmniPod five, they would not deal with that like they wouldn't touch it or interact with it. So my mom had to do all the, all the stuff on it, whenever something would happen, she had to change the pods, enter carbs, if he was eating anything, or do any corrections. So she was left in charge of that because the hospital staff refused to be involved, refused to be involved with it. And they also wanted to know, you like, how much insulin he was getting for different things, you know, whatever. If he feed some crackers or whatnot, they wouldn't know how many, how much insulin he was getting for those crackers. You know, it's kind of hard to say to my mom, you know, you can't really tell him how much insulin he's getting because the algorithm is algorithming. It's doing its thing, right? So they had no clue or idea on how to deal with a pump in that setting, probably
Scott Benner 38:03
Jason. They probably don't understand how to deal with it out of that setting, either. But yeah, yeah, we'll learn about that here shortly. Yeah, and they, and they weren't interested. The bigger, the bigger point is, is that they're not interested. They're going to chart what they need to chart, but like, they're not going to touch it. They're not going to learn about it. That's not going to be a focus for them. When you said he was kind of comatose, like, this is after 10 days with covid, after his quarantine period, yeah.
Speaker 1 38:30
Like there towards the end of the his covid stay for 10 days, like he just would not recover and kept sleeping more, just laying down more, not sitting up much, not opening his eyes, not talking.
Scott Benner 38:43
What did you think was happening at that point?
Speaker 1 38:46
Part of me, you know, was hoping that he would make it through and be able to, you know, return to somewhat normal life where it was at that point in time. But the other side of me knew that this is probably his last, last little bit of life that he's going to be spending in this hospital. Yeah.
Unknown Speaker 39:04
How long ago was this?
Unknown Speaker 39:05
Just last year, January, okay,
Scott Benner 39:07
did you cognitively understand that his heart attack and his strokes were from from high blood sugar support management? Yes, okay,
Unknown Speaker 39:15
like 100% All right. So
Scott Benner 39:17
you know, there's still other things happening inside of him that are also being impacted by that, and have been for decades, and now, exactly I know this comes along, and it's stressing every system, right? You know, what did you mean by? I'll find out more. What happened next
Speaker 1 39:32
after his 10 days, it kind of deciding shortly after that that they're going to call in hospice care, because, you know, he's struggling to breathe, he's not eating, he's he's not he's not trying to live. The hospital staff decided to move over to hospice care, and my mom said, Yes, that's, it's, it's his time, like it's going to happen. So let's go ahead and do that. And once they moved him over to hospice care, you. They, you know, stopped all medications besides morphine and that unfortunately included insulin. Stopped giving him insulin after his last pot expired, and really didn't take any care or concern about his blood sugars. At that point in time, they would check his blood sugars, but you know, it'd be every three four hours, and there's no response to the high blood sugar until I showed up at the hospital.
Scott Benner 40:33
So I've watched a hospital manage my mom to the end of her life. So if once they decide you're not coming back from this, they start removing all the things that keep your body going. And it's interesting when you're when you're older and you've been sick for a long time, you don't think of it that way while you're alive, and you're going like this, pills for my blood pressure, this pills for my you know this, and you know my lipids and this is happening, and what you really, like, begin to understand in that time is that you have been artificially kept alive for so long. Like you weren't gonna die, like, if you stop taking all your medication and doing all the things you're doing, you weren't gonna, like, just shut off, but the end of your life was going to be sped up without your heart medication or etc, whatever else you're taking. And then it's such a weird feeling when someone says we're going to discontinue those things. And you think, but those are the things that are keeping her healthy, right? And then you're like, oh, even though I knew this is what we were doing, I didn't know this is what we were doing, right? Like, we're gonna take away all the things that are keeping, keeping this person alive, and to to to hasten the end of their life. You're trying to get to it faster, because it's just seems cruel to, you know, if, if the end is the end, and they're struggling, or, you know, why? Why would you keep that going any longer than you had to? Right? So you get to that situation, but the taking away the insulin, and you not live with it like, what is that about there in
Speaker 1 42:11
my eyes, from, you know, being type one myself, from my, from my point of view, like a high blood sugar is insanely uncomfortable, especially when you get up to like, 400 or 500 you know, you get that, that thirst sensation that's unquenchable, like you have to drink something. In my eyes, when he was in hospice, you know, they wanted him to be comfortable. You know, they're shooting him full of morphine to make him comfortable, a little bit of insulin to bring him down to a normal, somewhat normal level would make him more comfortable. I don't think it's like a blood pressure medicine or something like that, that you know you don't feel it when you take it. You don't feel the results of it. You're not going to be uncomfortable if you don't take that medication for a day or two days or three days, but if you're doing multiple days or multiple hours without insulin, and that blood sugar is, you know, 400 500 600 that's incredibly uncomfortable, yeah, and I don't think anybody really thinks about that. I don't think the hospital staff thinks about that. I'm not even sure if his doctors thought about that. And I would be curious as to, like an endocrinologist thought on that, like, Is that comfortable? Is it something that should be dealt with? Yeah,
Scott Benner 43:29
but he was on morphine, right? Yep. So do you not think that they were just trying to hasten things by removing the insulin? I don't think
Speaker 1 43:39
that crossed their mind, like them, thinking of DKA wasn't on their radar.
Scott Benner 43:45
And did you speak to them about that, or was that just your feeling? I
Speaker 1 43:48
spoke to them about that adamantly, and that kind of explained my point of view, and we finally got them to come in and just give some small correction, small corrections throughout this last few days and kind of get them down to a moderately okay level. But it was hard. It was really, really difficult to get them to do anything. And when they decided, you know, hey, we're going to do something, well, we agree to giving him insulin. You know, it took him two, three hours to come back in with the insulin to give it to them. It was really slow.
Scott Benner 44:25
Can you describe your state of mind during this time?
Speaker 1 44:28
I was extremely pissed off, because I'm used to, you know, I'm used to dealing with type one diabetes like now, like you deal with it now. You don't let us sit you don't, you don't do that. And just seeing how slow the process worked, there it was infuriating.
Scott Benner 44:47
You think you were mad because you couldn't help your dad, and you were looking for a way to help him. Yes, yeah. Did they ever say to you were mad? Edging the end of his life. Now we're not going to give him insulin.
Unknown Speaker 45:02
Yeah, that was their their perspective on it.
Scott Benner 45:06
What was yours though? Like, you knew that was happening. Were you okay with this? The what, what was being done?
Speaker 1 45:11
I wasn't okay with it at all. Like, I just can't, like, even, even if he was on morphine and out of it, not really aware of what was going on around him. I can't imagine your body not saying to you, hey, you're really thirsty, your mouth is really dry right now, and you might have a headache, you might feel like you gotta puke, you might feel all of these things, but you can't do anything about it, because you're you're locked in this bed, and you're locked inside your body, right, just sitting there, and you can't do anything about it.
Scott Benner 45:43
Were you okay with the idea that he was dying like, like, and that the plan was he was in hospice now to get to the end of his life, or did you think he should be fighting
Speaker 1 45:53
after seeing him in the hospital, after he kind of had his quarantine from covid, like, I knew that it was coming, like I could see it coming. I think kind of, I made it a little bit easier to deal with, but I still didn't want him go through that process and suffer from type one diabetes still.
Scott Benner 46:12
Yeah, okay, so that's really the aspect of it. Like, not that you're okay with his passing, but you're okay with what we're doing. I know what we're doing. He's he's gonna pass away. We're managing towards that. But just like emotionally, psychologically, you couldn't stop taking care of his diabetes,
Unknown Speaker 46:29
right? Yeah,
Scott Benner 46:32
you know. Why do you have any thoughts about it? You go to a therapist. Anything? No,
Speaker 1 46:37
no therapy. I just listened to that episode of the podcast with the therapist on it. So that's mine. Oh, yeah, sure. I'm
Scott Benner 46:43
sure she'd be thrilled that that's your therapy.
Speaker 1 46:47
Hey, the ground, the grounding method helped me tremendously. So thank you for recording that episode. Oh, did
Scott Benner 46:52
it really? Oh, that's fantastic. Yeah, good. I'm glad. Oh, you're stuck in this conundrum where the plan is we're going to take away my dad's stuff. He's going to pass away, but I can't let it be as his insulin. So did you, you talk them into giving it to him eventually?
Speaker 1 47:06
Yeah, we, we talked to him. I really had to push like my mom was, you know, out of it. She had just recovered from covid and dealing with, you know, her husband passing away, or in the process of passing away, she was just kind of there, nodding her head, agreeing with everything, and not necessarily always remembering what she agreed to. But I finally convinced her to say, we really need to do something about this. Can you please ask, you know, the hospice care people and the doctor or nurse whoever to come in and let's talk about this. You know, I kind of, when they came in, you know, I kind of put my foot down. I said, you know, having a blood sugar this high is not comfortable, um, and you guys want them to be comfortable, so we're going to do something about it. And, uh, eventually, you know, that, they said, okay, and then, you know, three hours later, they come in and do something about it.
Scott Benner 47:59
Yeah, it's tough, because they don't get very assertive. But, like, they could have made the argument that DKA could could help him pass away, right? It's such a weird thing, like you're turning the body off, you know what? I mean? Like it the person's dying to begin with, and you have all these artificial things in place to keep that from happening. So they take them away. It's interesting. They must have seen you must have been really pissed, I guess, is what I'm saying. Yeah, you must have scared them into doing it. And they probably thought he's going to die one way or the other if we give him this insulin or not. So let's just make the family happy and do this. Yeah?
Speaker 1 48:32
And that's kind of like my point of view on hospice, is that, yeah, make make the patient, the person dying, happy or comfortable, and you gotta make the family comfortable. Also, they gotta be comfortable with the process. Him suffering from high blood sugar along with dying wasn't something that I was willing to really compromise too much on,
Scott Benner 48:55
yeah, well, and you didn't. So after you got the insulin, what happened afterwards? They keep managing the insulin he wasn't obviously eating where they and they took his intravenous or his IVs away as well, right?
Speaker 1 49:09
Yep, yeah. They took all that away so they would just come in, you know, every however many hours in between, checking his blood sugar, coming back, you know, 3040, minutes later, to give him a small correction dose. And of course, you know, I agree with, agreed with them, that we shouldn't try to bring him down to a normal level, because he can't eat or drink anything at this point in time. So it's just try. Hey, let's use them close to 200 so they they'd come in quite a bit, quite a bit, quite frequently after that, and just give him small correction doses.
Scott Benner 49:43
How long did he? Did he last after that?
Speaker 1 49:48
So he was in the hospital like a total 25 days. 10 of those were heavy covid stuff, and then 15 of those were two. Kind of all downhill from there, type of thing. Yeah, and I think it was in hospice care for probably just shy of a week.
Scott Benner 50:07
How were you there all the time? Or how did you guys manage the that?
Speaker 1 50:12
No, we weren't there all the time. We went over there. That's a like an hour drive from our house to where there the hospital was at so we drive over every day and see him, because we know we have three kids that are still in school at that point in time, yeah. So we had to kind of maintain a somewhat normal life. And you know, my dad being the workaholic guy, he would have agreed with that. He would have been okay with that, okay
Scott Benner 50:38
with it. He would have been like, what are you doing here? Staring at me. Yeah,
Speaker 1 50:42
that's that. That's exactly what he would say, yeah,
Scott Benner 50:46
make some money. Help somebody. Yeah.
Unknown Speaker 50:48
Help somebody. Do
Scott Benner 50:49
something. How they're going to know that you love them if you're not working exactly? Oh my gosh. I have nothing but sympathy and and respect for the the process. I can tell you that in my mom's hospital room, at one point, I sort of just went to a corner where I wasn't in her sight, even though I don't know that she could have seen me to begin with, and I don't know how to explain that, I silently screamed and gritted my teeth so hard I thought they were gonna break, because I was had come to the realization that there was nothing left to do, right, you know, and that was a terrible feeling for a person like myself, you know, who you know seems to be minded towards caring for people to begin with. And you know, just as her son and, you know, and my brothers were there and I, I had grown up in a very hybrid situation where I was parenting my brothers and their brother at the same time. So now we're, you know, now we're there, and I'm in my 50s, and my brothers are, you know, in their 40s, and I still feel like, on some level, those are, they're my like they need me to say something or do something, or be something, and at the same time, I'm having my own very personal, you know, experience. And it was, it
Unknown Speaker 52:08
was very
Scott Benner 52:10
upsetting. Is not the right word, but I thought I was going to break my teeth while I was silently screaming it through my chest, is what was happening. Yeah, you know, it's just maybe, I mean, I don't see how anything's worse than this, you know,
Speaker 1 52:25
yeah, it's a it's a weird trip to uh, lose a parent. It's uh, it's just something you don't, you can't know about until it happens, right?
Scott Benner 52:35
It's not something you can prepare yourself for. So if it happens to you too early in life, I can see where it would really just get to you in a different way. And even though I was 50 and had lived through my kid getting diabetes and all the other things that had happened, I do think I was more prepared for it because of that, but I'd say that when it's over, your perspective levels up again. And I thought I had some pretty high perspective from living through type one diabetes, and, you know, every day realizing that a little too much of this at the wrong time. And you know, that could be it like, even last night, I'm still trying to adjust Arden's insulin back properly, because she's using that. GLP, yeah, and she got into the mid 50s last night at like, 130 in the morning, and I let it go for a couple minutes, and like, she's not seeing this, I texted her, and she didn't answer me. So I got out of bed and I walked into another room so I wouldn't wake up my wife. And I called her just to arouse her and get her awake. And she texted me, and I said, Hey, just like, drink a half of juice. But in those couple of minutes, like the couple of minutes where you're like, she'll be okay, she's low, but she'll be okay, okay, she's not taking care of it, like, she's not waking up. I'll wake her up. I woke her up. That's good. She drank something. I see her blood sugar coming back up. That whole time is only like, 10 or 12 minutes, you know. And in that time, like, standing there with my phone in my hand, I thought everything in my house looks so normal right now, like everything looks like every other day I walked downstairs and let the dogs out while I was doing this, like, but is Arden gonna die right now? Like, you know what I mean, like, and I don't think about it that way, day to day, but last night, I was probably just the right mixture of woozy, a little asleep, a little awake, where I didn't, you know, manage myself that way. And I thought, wouldn't it be weird if, like, everything was so normal in the world, and she just disappeared, and you know what I mean? And and then i She's like, texting me. She's like, I drank it. I'm like, Okay. And then I was like, Yeah, she'll be fine. But a lot of people don't live in that space, you know, and so I thought I had some pretty massive perspective about what's important in life and what were to focus and those sorts of things. Then my mom died, and I thought, Wow. I didn't think I was going to be able to level up. But here it is, I hope. Nothing else terrible happens, because I'm good with where I'm at now, as far as perspective, I don't need any more, you know, but I don't know. Maybe more will come. Still, Jason, I'm not sure. Yeah,
Speaker 1 55:10
something that similar thing happened to me too. Like, you know, the past year my dad's health, it's just been terrible, and watching him kind of start falling down that ladder ramped up my anxiety. You know what really kind of got my anxiety really wound up is thinking, what, what if I get low and I die? Or, what if I get low and crash the car and die? Who's going to take care of my family, like, who's going to be there for them? And that's a it's a hard, it's a hard thing to think about. Do you think you're
Scott Benner 55:42
examining your mortality in that, or do you think you're reacting to the idea that your father's gone? Because you know before that, if you would have died, he would have taken care of your family.
Speaker 1 55:52
I think it was just it's amplified by him having these health issues and seeing him being the guy that if you needed something done, you call him at that point in time. You know, I wasn't able to call him anymore because he couldn't, couldn't do these things for us anymore. So it's kind of like I'm stepping up into that role.
Scott Benner 56:12
Yeah, it's me now. There's nobody behind me anymore, right? Yeah, the way that happens to me is I imagine everybody I've ever been related to, standing in a line at a cliff. They fall off the cliff as they die. And then my mom, my mom went off, and I was like, Oh, I'm next. Like, there's no one in front of me in this line anymore, right? You know, that was the thing that got me. I was like, there, you know, it's my dad and my uncle and my aunt and like all these people, even though I wasn't even that close to them, like all these like all these people, like, I felt like if they were alive, I was going to be alive, because age and chronology, you know, etc, even though that's completely ridiculous, I'm sure the guy standing on that bridge in Baltimore didn't think they were going to die right before that, yeah, but um, but in my mind, that's always what comforted me. I'm like, there's more people to go before it gets to me. And then my mom, my mom passes away. And I'm like, there's no one left standing between me and the edge of this cliff. And, yeah, that's when you start doing things like, you know, trying to put away more money, and talking to your kids about stuff that you're like, they're probably like, Why the hell are they explaining this to me, like, that kind of stuff, you know? Yeah. And actually, it's funny, my dad left my mom, and I can look back and see that he was planning it for a while. And the one way that I really like, like, this kind of touch point for me is I was like, I don't know, I was 12, and he drugged me into the basement one day to explain how the fuse box worked. And, like, I remember the time thinking, like, this is cool. My dad and I are doing something together, you know what I mean? And like, trying to understand the fuse box. And I felt like I did understand it. And I was like, Oh, cool. Look at me. Like, there's they were the old screw and glass ones, you know. And, well, you know, your dad's electrician, like, and I was like, Oh, wow. And then I look back some years later, and I think, oh, he was just explaining to me how to take care of the house because he was going to leave. And I don't know that it's any different with dying, except maybe you don't plan to die, you know what? I mean? Yeah, yeah. So, yeah, I've
Speaker 1 58:16
been, I've been slowly doing that, like, ever since I started really feeling that anxiety, like slowly dropping those little hints or knowledge on my wife, like, you know, if you need to take care of this with loop, this is where you should go and look at it. You want to look at it? And she'd say, No, of course, but,
Scott Benner 58:34
but you're thinking, look at it, in case my body explodes and I'm not, unexpectedly, that's right, yeah. Now that's, uh, how are you making out getting through that anxiety?
Speaker 1 58:45
Well, you know, after learning about the grounding method from the juicebox podcast, subscribe, turn downloads on that stuff. I that that episode on grounding, I probably have listened to that 10 times. No No kidding, I've kind of picked out things within that, those grounding methods that kind of really helped me, and I've gotten pretty good at making it happen quick when I start to feel that anxiety, come on. So, you know, I can usually just look at something, and I kind of start describing it in my head. I would feel how it would touch, how it would feel when I touch it, what it smells like. And it kind of calms me down to a point to where I can let my mind move on to something else.
Scott Benner 59:29
It's episode 913 it's called the 54321, method. And it's just Erica, who's the a licensed marriage and family therapist who she has type one diabetes for like forever, like over 30 years, and I have her on to talk about this kind of stuff. It's where I like, where we pick a topic, and then normally it devolves into me talking about how I feel. She and I did this, this grounding method. What is it? It's five things. You can see
Speaker 1 59:59
we're. Things You Can that's, it's like, see, touch, you know, feel them, something, those five things, just to get your mind to focus on something else. And they and I really, I just kind of picked out of those methods, just like, What things would feel like if I were to touch them, just the general shape of things and things like that. That kept that really helped me.
Scott Benner 20:00:21
Yeah, the 54321, method involves identifying five things. You can see, four things, you can touch, three things you can hear, two things you can smell, one thing you can taste. And by doing so, it shifts your focus from anxiety provoking thoughts to a present moment.
Speaker 1 20:00:36
And it works for you, huh? It most definitely works for me. That's very cool. Well, it's
Scott Benner 20:00:40
a shame you're not gonna have any more kids, because I think we could have got a Scott out of you, for sure, but I
Unknown Speaker 20:00:49
would have named him Dave, go with it. Yeah, you
Scott Benner 20:00:51
know what, honestly, would have been the way to go. Well, I'm grateful that that it helped you. I wish you knew. I wish you guys all knew that most of what the podcast is is the thoughts that I have standing in the shower in the morning. And I think I bet you people would want to know about this. There's no production meeting or anything like that. Nobody's telling me what the like do or say. I just one day I got it in my head. I was like, I heard about this method. I watch people do it. I thought, boy, that makes sense. And then I listened to some people online talk about it. I was like, Wow, this helps a lot of people. I'm going to ask Eric if she knows about this, and like, really was the extent of it, and to hear that it made it all the way to Iowa and to you, and that it was valuable for you while your father is passing away and and you know, afterwards, it's very heartwarming for me. So I appreciate you sharing that with me, because, you know, day to day, it just feels like I sit in this room and click on things and, you know, and talk and make sure this thing's in front of my face when I do it. That's right, yeah, but to know that it actually works out, like I'm working on something now for the podcast, for like, later, it's a lot of work. Like, I'm not gonna lie to you. It's like a lot of me sitting here and talking to myself, I'm not gonna tell you what I'm planning yet, and it's hard. It's hard to get the energy up for it. It's hard to have an engaging conversation by yourself in a room, one of those things, like, anybody that can do that. I have a lot of respect for stand up comedians like even get feedback, you know, from a crowd. But even though you can make the argument that they're on their own up there, but I am not getting any feedback, so I have to kind of imagine how you feel while I'm doing it. And I slowed down on that project because it's just such a slog. Yeah, you know, you saying this to me, honestly, will help me get energy up to to finish it up and get it out to you guys. It's a ton of I almost curse, but it's a ton of I'm gonna curse anyway. It's a ton of work, and I don't get any like, nobody at the end of the day is like, you're doing a good job, or try harder, or do this differently. I just, I'm like, on my own to figure out what it is anyway. I appreciate it very much, and it'll be helpful to me. So thank
Speaker 1 20:02:59
you. Yeah, well, keep, keep taking showers, Scott, and keep coming up with good ideas. Well,
Scott Benner 20:03:03
hell if I stop taking showers. We have bigger problems than the podcast falling apart, right?
Unknown Speaker 20:03:09
Keep taking showers.
Scott Benner 20:03:12
Oh, my God, Jason, you just named the episode. Yeah, there you go. Well,
Speaker 1 20:03:17
we need you to keep coming up with good ideas. And I'll, I'll keep, I'll keep posting in the Facebook group. Try and help people and help you come up with ideas. You're definitely doing, like a real job. You gotta think of like all those like podcasters, YouTubers, these jobs didn't exist 10 years ago. Yeah. So it's hard to, I think it's hard for some people to say that what you're doing is a job, and you deserve compensation for it. You definitely do, and I think you're doing a fine job of it. And thank you. You know, top of the game, type of type of job, and I think you deserve to be paid. And however you get that money? You get that money?
Scott Benner 20:03:54
Well, I'm not human trafficking people like P Diddy, allegedly. So Right?
Unknown Speaker 20:04:00
So you're just taking money from OmniPod and Dexcom and cozy Earth. And
Scott Benner 20:04:05
I'm older, so I'm still slightly embarrassed to be a podcaster, not embarrassed, but like, there's a little piece inside of me that's, like, you don't really that's not a real job. Like your dad, it's your dad would think I'm doing a weird a real job. Yeah, yeah. And my dad, you know, it's funny, my father, while not an electrician, did all the electrical work at the rubber molding plant that he worked at, like so your dad and my dad were pretty similar people as far as what they did for a living. He worked in an industrial situation, big, heavy machines that it was his job to take care of and keep them running. And then when that, when nothing broke, they would just point him to the floor, and he'd go work on the floor. And, you know, like he was the maintenance supervisor. But I also, there were days he came home where he just, you know, he did the grind too, like he, you know, they put him in front of a machine and said, you know, make 10,000 of these things come out of here by the. End of the day. I think if I would have told my dad, you know, that I'm gonna do this, I think he'd be like, What do you mean? Like, you know, like, go do something. Like, go work on something. My mom never understood exactly what I was doing. Like, she was older by the time I was really at it, and she's just like, she knows I talk to people, like, through the internet. Like, that's basically what she understood about it. And I think my kids make fun of me because I feel like I have a 12 year olds job. Like, you know, like, it's funny. Like, to older people, you're not really working, and to younger people, they're like, oh my god, are you and are you on tick tock right now? Like, I get notes all the time. Please stop doing this. Like, or they'll send me, they'll send me links of myself, like, trying to get people to listen to the podcast. Like, don't do this ever again. I'm like, and I'm like, look like, if you can get people to listen a different way, like, let me know what it is. But right now, this is how the world works. And you know, I'm stuck standing in front of a light, talking into my phone, telling you that episode, whatever came out today, and you should check it out. Yeah, anyway, I appreciate you very much. Is there anything we didn't talk about that we
Unknown Speaker 20:06:07
should have? I don't think so. I think we, we hit the hits all the bases. Aaron got him. Yeah,
Scott Benner 20:06:12
well, I'm so glad you said keep taking showers, because I was like, I was down to, like, using the word hospice in the title. And I was like, Oh
Unknown Speaker 20:06:19
God, no one's gonna listen to that.
Scott Benner 20:06:23
Just gonna be like, No thank you. Not on a Tuesday, but it's just very important conversation. Jenny said to me the other day, we were doing a just a pump. I think we did, like a pump and CGM overview. I think we did, that's how much I do this. And during that, she said, Are we going to talk about, you know, older type ones and how these, none of this technology is made for their fingers or their eyes, you know, or their ability to work on stuff? And we, you know, we talked about it for a minute, but like, there's not much to talk about. Like, because what are you saying to a pump company like, go make something for a person at the end of their life, and they're gonna say, oh, they'll get somebody to help them with it. Like, we can't just make a product for that small number of people, but it's still a big deal. Like, you know what I mean? Like, you're gonna get older one day and your fingers are gonna shake, and, you know, if you're lucky, they're just gonna shake. And how are your eyes gonna be? And how are you gonna understand that? Could you understand? Do you think you could have taught loop to your father, absolutely not, yeah. So you know, when that becomes the standard of care and algorithm, like, how do you, I mean, he made out okay on OmniPod five, though, right?
Speaker 1 20:07:32
Yeah, he, he did. But I think a lot of that had to do with my mom helping him his like, I think a lot of that comes down to his mobility, too. Like him being an electrician for the majority of his life, his hands were beat the shit, yeah, so they could hardly register when he touched a touch screen. You know? That thought he was dead already, and so she had to do some of the button pushing for him when it wouldn't work for him, and he didn't have the dexterity in his hands to put pods on. So she had to do that for him. Yeah. So it kind of, you know, shows that some of these things are need to be taken into consideration with an aging population, or a population that doesn't have the that mobility or ability anymore. Listen,
Scott Benner 20:08:20
I worked in sheet metal from the time I was 16 until I was in my 20s, and you know, it wasn't even that long, and the skin on my hands is still like, it's hard to put into words, like I haven't done a real job in a long time, and my fingers are still very dry all the time. Stuff slips out of my hands a lot, if that makes sense or not, but whatever Spider Man has, I have the opposite, you know, and it's I was always touching, you know, this is back before people paid attention to things. My hands were like, we used to wash our hands and paint thinner.
Unknown Speaker 20:08:53
Great, yeah, my dad did that, yeah,
Scott Benner 20:08:55
you know, of course. Like, how do I get this grease off me quickly so I can go eat lunch? Paint thinner, yeah, you know. And then they finally came out with that soap that scrubbed it off. And, you know, you're like, oh, wow, look at the advancement here in my life. I'm not using paint thinner anymore to clean my hands. There are still days I think I'm just gonna wake up with lung cancer one day and I don't smoke or bleed, an unhealthy life at all. But I worked in that place long enough I'm like, hopefully it's not going to get me. But, you know, I don't know that it can. I mean, I worked in the industrial situation before people were like, you know, wear your personal protective gear.
Unknown Speaker 20:09:33
They were right, yeah,
Scott Benner 20:09:35
I made $5 an hour.
Speaker 1 20:09:38
Well, maybe that's why, man, that's why you have your good podcast voices from breathing in all that you shouldn't be breathing in.
Scott Benner 20:09:43
Wouldn't that be great? The thing that propelled me at the end also got him. We'll need somebody to write that on my tombstone. Anyway, Jason, nothing like talking about death with a with somebody at 9am this was great. It was Yeah. I really did appreciate though, and I appreciate you. I imagine you know that, but thanks very much
Unknown Speaker 20:10:04
for doing this. Yeah, no problem. It was a pleasure.
Scott Benner 20:10:07
Hold on one second.
Did you know if just one person in your family has type one diabetes, you're up to 15 times more likely to get it too. So screen it like you mean it, one blood test can spot type one diabetes early. Tap now talk to a doctor or visit screen for type one.com for more info. Arden started using a contour meter because of its accuracy, but she continues to use it because it's durable and trustworthy. If you have diabetes, you want the contour next gen blood glucose meter. There's already so many decisions. Let me take this one off your plate. Contour next.com/juicebox a huge thank you to ever sense CGM for sponsoring this episode of the podcast. Are you tired of having to change your sensor every seven to 14 days with the ever since CGM, you just replace it once every six months via a simple in office visit, learn more and get started today at Eversense cgm.com/juicebox, hey, thanks for listening all the way to the end. I really appreciate your loyalty and listenership. Thank you so much for listening. I'll be back very soon with another episode of The juicebox podcast. The episode you just heard was professionally edited by wrong way recording, wrongway recording.com
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!