#1113 Cold Wind Healthcare Whistleblower Bedside Nurse
"George" is an anonymous bedside nurse and CDE who provides insight on working with everything from egotistical doctors to his personal frustrations with the healthcare system. His voice and name have been changed to protect his identity.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:00
Hello friends, and welcome to episode 1113 of the Juicebox Podcast.
We are already four episodes into the new cold wind series. I hope you're enjoying it. Today. George has had type one diabetes for 25 years. He grew up going to diabetes camps and being involved with the diabetes community. One day he decided that he wanted to become a nurse. After graduating, he did four years of bedside nursing and a diabetic bedside renal unit. And that led George to become a diabetes educator. Currently, he does diabetes education full time in a large inpatient facility. Hello, and welcome to the cold wind series from the Juicebox Podcast. These episodes will feature physicians, nurses and other professionals who agreed to come on the show anonymously to share what they see in the healthcare profession. I've altered the voices of each guest so that they can remain anonymous and feel comfortable telling us what really goes on at their job. Just listen to how well the voice altering works.
George 1:12
My name is Beth and my oldest child has type one diabetes diagnosed in October 2020. My name is Beth and my oldest child has type one diabetes diagnosed in October 2020.
Scott Benner 1:24
If you work in health care, and have a chilling story to tell about your experiences in the healthcare field, contact me today. I'll get you right on the show. Your story does not need to be specific to diabetes. Nothing you hear on the Juicebox Podcast should be considered advice medical or otherwise, always consult a physician before making any changes to your health care plan. When you place your first order for ag one with my link, you'll get five free travel packs and a free year supply of vitamin D. Drink ag one.com/juicebox Don't forget to save 40% off of your entire order at cozy earth.com. All you have to do is use the offer code juice box at checkout that's juice box at checkout to save 40% at cozy earth.com.
This episode of The Juicebox Podcast is sponsored by touched by type one touched by type one.org. And find them on Facebook and Instagram touched by type one is an organization dedicated to helping people living with type one diabetes. And they have so many different programs that are doing just that. Check them out at touched by type one.org. This episode of The Juicebox Podcast is sponsored by the contour next gen blood glucose meter. Learn more and get started today at contour next one.com/juicebox. Okay, George, what's your background?
Speaker 2 3:03
Yeah, so my background? Well, first off, I've had type one diabetes myself for 25 years, I grew up going to different diabetes camps being involved in the diabetes community. And once I was getting ready to graduate high school, trying to figure out what I was going to do, I decided I wanted to become a nurse. And so that led me to nursing school. And after nursing school I did about four years or so of bedside nursing on diabetic renal units. So I saw a lot of interesting things there. And that was ultimately to get me to a place where I felt like I could be in a good spot to be a diabetes educator. So I went on and got certified as a diabetes educator. And now that's what I do full time on it an inpatient, large hospital. Okay, so that's kind of what to do. All right.
Scott Benner 3:53
Maybe these educator now. You see you've had type one for 25 years. 25 years? Yep. Okay. How old are you? You might be asking, yeah, I'm
Speaker 2 4:01
- So I was diagnosed when I was just turned five. Really? Well. In fact, I missed my fifth birthday party.
Scott Benner 4:09
As so many do.
Speaker 2 4:11
Yeah, right. I got I got sick. It was like the flu or something. And my parents had already you know, put a bunch of money down on a big like fun entertainment center place. So they're like, well, let's all your friends go to this and Oh, my God do it. Seriously. Yes. So they went to it. And it was fine. I opened my gifts at home but and sure enough, like for four to six months later, I'm diagnosed with diabetes.
Scott Benner 4:36
I think I like your parents on that. I think I like you know what, buddy, it sucks. But everyone else is gonna go you hang. Yeah,
Speaker 2 4:43
I mean, honestly, like if I think I'd probably do that. Now. You want to other people that you invited to have a good time that kind of your Red Sox, but it kind of is what it is. In that situation. There
Scott Benner 4:51
are three kids already. Wow, congratulations.
Unknown Speaker 4:55
Thank you.
Scott Benner 4:57
So we're gonna dig Again, and the these episodes are usually a little more direct than some of the other ones. So let me start first with being in the renal unit, what did you see there.
Speaker 2 5:11
So in the renal unit, it's a lot of really uncontrolled diabetes, that has led to like dialysis and kidney failure. So within that setting there, we saw a lot of people who were, you know, being started on hemodialysis or peritoneal dialysis. And when that happens, your insulin needs drastically change, you know, you could have been quite resistant to insulin for a while. And all of a sudden, because your kidneys don't function, you're ultra sensitive to insulin. Not to mention, it also stays around in your body for so much longer. So, one of the biggest issues I saw in regards to insulin and the kidney patients is that a lot of the doctors didn't know how to properly dose the insulin. It's just like when you go into a hospital, for the vast majority people, it's very generic. You know, you look at someone's bodyweight and go, Okay, they're low resistance, sliding scale. Oh, he's got a high eight, once he let's give him an aggressive resistance, sliding scale. And I'm sure for for some doctors, it might be more detailed than that, but especially with like, say, a resident, a new a new doctor, you're gonna get that a lot, right? So you might have a guy who's had horrible controllers, diabetes has a really high a one seat, maybe like, 14 15%. He's on dialysis, that changes everything. Right? You can't you can't just go in with the aggressive scales. And what would happen is we get these patients having these horribly critical low blood sugars when they're below 20. You know, I saw one time there was a lady that she had been my patient that day before and I happened to walk by her room, she was foaming at the mouth. And it was from low blood sugar. And we got her to come back. But it was that exact scenario there. Yeah, that just way too aggressive.
Scott Benner 6:58
I interviewed somebody more recently, who had to have, you know, didn't have diabetes, when they went into the hospital, had their pancreas removed, had diabetes when they woke up, and you know, needed insulin when they woke up, and they just didn't give her any. And the conversations between the nurses, she's, she looks back on now. And she's like, we're baffling. Like they didn't even like it didn't occur to the nurses that we just took their pancreas out. They need insulin now. Like it was on the level of, hey, we remove their heart, how come we're not pushing blood through her anymore? Like they just didn't even know it. And I thought to myself, like, I may have said out loud at the time. This can't be the first time they've removed somebody's pancreas. Like, how can this be a surprise? You know, but there it was, and it was so
Speaker 2 7:48
yeah, and we see stuff like that a lot. You know, honestly, with everything that's gone on in healthcare in the last couple years, like the pandemic, there's been such high turnover with nurses and doctors that, you know, you're you might have a charge nurse on the unit who's only been a nurse for like six months now. You know, and so there's your people, I think you're kind of getting into scarier situations. Okay. Because of potentially lack of experience, I think there's higher demands on doctors than ever before. Like, is that because of what why do you think I honestly think it comes down to profit, a lot of the times, you know, each individual doctor might not be thinking that way. But if you're a part of a big system, the system wants to make a lot of money. And I think that is pressure that's put on the doctors to be like, hey, you know, you got to see this many patients every single day. And when you start rushing care, you there's inevitably going to be mistakes. I don't think that every doctor is devious or wants to, you know, do something bad. Right? I just think a lot of them are so rushed, that they don't have time to sit down. They don't have time to educate themselves. And it leads to these horrible situations. And it scars these patients, you know, so
Scott Benner 9:05
you're saying that because they're pressured to see so many people, because the hospital is a private institution, it's trying to make money and it makes money by helping people with their health. And so to see this many people, you don't get the very natural experience of being able to stop once in a while or ruminate over something or go let me go find out about this before I you don't have those options anymore. You have to go go go go. No. And in fact, like I said, it's almost feels like a zombie apocalypse when you're walking through the hospital because nobody makes eye contact. People quite literally like we're almost running into each other because everyone's on their phone.
Speaker 2 9:41
Texting another doctor, another nurse about a patient. And it's like it there's just so much I think that pressure it's like go go go keep seeing patients that
Scott Benner 9:52
are they texting each other because they don't know and they think maybe this person will know over here. It's possible. I don't know for every case then that kind of funny though, like we get yelled at for using the internet to find out stuff like to do like, you know, sourced information, but now they're forced to source information to, oh, that happens all the time. Please tell me my doctors not googling my problem. Sometimes. I can't speak for your doctor. But I have definitely worked with doctors who are Oh, great. So, so we really are down to now like, you just have a prescription pad. And I don't,
Speaker 2 10:23
to an extent, yeah. And let me tell you this other story, too. Like, I had a patient where this was in the diabetes educator role. And he had a transplant rejection problem to an Oregon. They put him on high doses of steroids for a while. And so naturally, that raised his blood sugar's, he didn't have diabetes, he was in like the pre diabetes category. Yeah. But he'd never used insulin. So that's why they consulted me to teach him how to do insulin. The plan was for him to be on steroids for like two to three weeks. So he didn't need a long term prescription for insulin. Well, the doctor prescribed the Medtronic in pen. Okay, that's that smart insulin pen. Yeah, great pen, if, if you have diabetes, and you're gonna need it long term, but that's also not covered by insurance very well, especially in someone who doesn't have diabetes. So the family is kind of freaking out, they get their like, our insulin prescription is gonna be $1,000. And this is already after they're discharged. By the way, they're calling me and telling me this on the phone. So they ended up getting the prescription. And then the NPN doesn't come with insulin. It's cartridges that you load into it. And so then they have this $1,000 device that doesn't even have insulin. So I ended up calling the doctor that discharged, I'm getting the impression that she was in there a huge in a huge hurry. So she went back and ordered the intent again. So instead of I think kind of slowing down and being like, Okay, that was incorrect, I need to order something differently, ordered the infant again. And so the family gets stuck with this device they can't even use there's no insulin, they ended up going to an urgent care to get a prescription from another doctor for the insulin. And when they filed a complaint with the hospital, the hospital told them what it looks like the doctor wrote in her notes that she was ordering the correct device. And so the hospital basically told them, we're not giving you $1,000 Yeah, yeah, yeah, we're not gonna pay for the you know if that's on you guys.
Scott Benner 12:21
I have to say, too, and I think your point earlier, if you had diabetes, and got a prescription for an implant, I think it would be like a nominal amount of money. It would Yeah. And so they gave him a pen that didn't have insulin in it. That doctor meant to give him like a Novolog pen or something like that.
Speaker 2 12:38
Yeah. So the our standard is that the human log quick pen, okay. And so like, in my notes, someone's gonna need it. All right, please prescribe to a lot of quick pen with pen needles, right. And so if they just look at the bottom of the note, you could pretty much copy and paste what I wrote and turn it into a prescription.
Scott Benner 12:57
And then after having made the mistake, and you bring it to their attention, they do the same exact thing again,
Speaker 2 13:03
do the same thing. And I'm telling you, it's still happening. This particular doctor, it still happens. And so every time, you know, I tried to be polite, I'm like, Listen, this is not correct. And yet it still happened.
Scott Benner 13:16
Do you know the doctor aside of like, have these interactions? Do you know more about them?
Unknown Speaker 13:20
I do. Yeah. Yeah. I'm
Scott Benner 13:22
just gonna ask you like big dummy, like somebody you wouldn't? Where we at? I would
Speaker 2 13:27
say, I would not trust this doctor with my family's health.
Scott Benner 13:30
Okay. That's all trust me, that making this series has really enlightened me. I have not, I've not heard so many people say, I would not go to the place where I work to get health care. Yeah. And I don't know that. That means the next place is any better. And by the way, how many people now are just using urgent care to be the prescription pad? Well,
Speaker 2 13:53
and that's a problem too. That's another problem. Like, I'll see patients I'm like, Alright, so you're in with DKA? Do you have insulin at home? And like, well, I've got like, half a bio left like, Okay, well, who do you go to you for your, your normal prescription? I go, Well, I usually just, I come to the IDI like once a month. And then I got a new prescription for insulin. You have stuff like that happening, too.
Scott Benner 14:15
Yeah. I mean, there's a difference between having a report with a doctor going in and saying, Look, here are all my symptoms. What do you think? And they say, I think you need this and you go, I came to the same conclusion. I would like that if you could. But that's not what most people's situations are, their understanding around their medical needs, you could come in with a completely skewed idea of what's going on, especially in autoimmune, where so many things mimic each other to begin with. Right? And if we start getting into the point where like, any one with Google can come say, I think I need this. The doctor just goes Yeah, it sounds right to me. What the hell, you know, like, Oh, my God, we could stop now. George, we could just stop right now and I'd go this has been horrifying. And but there's more right? Well, then There's more. Yeah, the contour next gen blood glucose meter is sponsoring this episode of The Juicebox Podcast. And it's entirely possible that it is less expensive in cash than you're paying right now for your meter through your insurance company. That's right. If you go to my link contour next one.com/juicebox, you're going to find links to Walmart, Amazon, Walgreens, CVS, Rite Aid, Kroger, and Meijer. You could be paying more right now through your insurance for your test strips and meter than you would pay through my link for the contour next gen and Contour. Next One, test trips in cash, what am I saying, my link may be cheaper out of your pocket than you're paying right now, even with your insurance. And I don't know what meter you have right now, I can't say that. But what I can say for sure is that the contour next gen meter is accurate. It is reliable. And it is the meter that we've been using for years contour next one.com/juicebox. And if you already have a contour meter, and you're buying test strips doing so through the Juicebox Podcast link will help to support the show.
Speaker 2 16:12
A lot of the examples I've seen have revolved around finances and money. Okay. And so here's an example. Now, I don't think this doctor in particular was trying to make money. I think he had a pride issue, this patient, I see that for diabetes education in the conversation that comes up, but they don't have insurance. You know, a once he was like a 13 or 14, clearly they needed insulin, the doctor had prescribed homologue Atlantis, and that was going to cost them like 700 something dollars, and there's no way they could afford that. And so I suggested to the patient, hey, you know, Walmart has rely on brand insulin, we could do a similar version of this, and it's gonna cost you like 50 bucks for the month or so. And so they're they're like, that's awesome. That's we can afford that we can't afford the 700. Right? Well, I called the doctor. He was very frustrated. I called him. And prior to calling him I had paged and just giving some recommendations because that's, that's like my job. It's not to tell them necessarily what to do. But it's to give some guidelines and recommendations like, here's what I would recommend. And so I said to him, I would recommend that this patient is put on rely on brand insulin so that they can afford it. And he on the phone, he told me he's like, it is not your job to tell me how to dose and Sony hung up on me. And so I ended up calling him back. He listened to what I had to say. And he told me he's like, I spoke to the patient's daughter who's a pharmacist. And there's no issues with finances, it'll be fine. So he ended up discharging the patient. I gave the patient my my hospital business card and said if there's any issues, give me a call. Well, sure enough, the next day, I get a phone call. And they're like, we're panicking. We don't have insulin. We can't afford it. So I ended up talking to the doctor again. He told me to direct them to the hospital on call Doctor line to the Vic and tell him how to dose the rely on Brandon sloughed.
Scott Benner 18:07
That's all ego.
Speaker 2 18:09
I'm that's my impression. Like, if you knew this doctor, he is like, I'd say more of a he's he looks stylish. He is more popular among the nurses. That's why I got the impression that it is more ego.
Scott Benner 18:24
George handsome guy. You're saying to me? He's He's He's handsome. Yeah, he's in shape. To be in the gym. Maybe everything's going his way. Yeah, yeah. Exact better car than you.
Unknown Speaker 18:35
Oh, that's for sure.
Scott Benner 18:36
I say okay, so it's, uh, oh, wow. Is that a common thing?
Speaker 2 18:41
I do see the ego kind of getting away a handful times. Yeah.
Scott Benner 18:45
So basically, all the things we see in regular society. People don't know how to leave that at the door to go be a doctor Sometimes. Sometimes. That's correct. Yeah. So this person has a financial issue. You've taken the time to understand it. Yes. Founder a fix for them. Which I hope by the way people know that rely on insulin is just Novolog. repackaged, is that correct? They
Speaker 2 19:07
do have Novolog Novolog rely on brand to be 72 bucks for that overlong. What I was doing with this patient was NPH and regular
Scott Benner 19:15
you were going that far. I'm sorry. So you were doing the the original T that's such a confusion, rely on Novolog. And there's there
Speaker 2 19:23
and it gets really confusing because they're all called no Overland. So Novolin are no violent and no violence. 7030 You know,
Scott Benner 19:30
I spend most of my life thinking who names this stuff? Right? You know how you can't confuse red and blue? Because they don't sound different. They're like, you know, I mean, like conventional blue and blah, like and I'd be like, Oh, which one is that? It's like, it's fascinating that nobody can figure this out. It's like when they build web pages and then they don't use them like Did no one try this website before they put it out as terrible. Right, right. Yeah, like think a little bit but anyway, okay. So there's dickheads that are doctors to you're saying Oh, yeah. Okay, well, there we go, then you
Speaker 2 20:03
have to highlight, I gotta highlight some really good doctors real fast, like, yeah, I've got, I got a friend and he's like the sweetest guy alive. And he'll, he'll actually be like, You know what I'm gonna spend, I'll see if less few less patients, but I'm gonna spend 2030 minutes with the patient and actually figure out what's going on, figure out if I need to call on specialists. And you know, I talked to the patients, and they're like, We absolutely love this doctor. And so you can see that that is what, on a personal level, that's what works. It's not this corporate this, see a bunch of people will be having an arrogant doctor. That's not what works. But that's that's kind of the way I feel like our society has pushed it a little bit.
Scott Benner 20:43
Is it possible that some of that arrogance is just maybe it's self loathing? Maybe they're like, I know, I'm doing the wrong thing. But this is what I got to do.
Speaker 2 20:51
It could be and I think there's also a part that if you are confronted with saying, like, Hey, you might be doing the wrong thing. What if you have done that 1000 times with someone else, right? You have to admit to yourself, I could have potentially harmed 1000 people to get to the realization that I was doing this wrong. I see. Oh, so you could be that pride of like, it's better for me just to bury my head. Put up that that wall, then for me to have to confront the reality, potentially. Have you ever heard
Scott Benner 21:21
my episode called listen to the doctor, where the endo comes on? And just flat out admits that the podcast changed how they help people? Oh, I did hear that. Yeah. I've never been prouder of a person I've never met in my entire life. You know, so cool. Yeah, just just she just said, like, I listen to the podcast, and I, I started doing things differently. And it's helping. And then she told me, she basically told her staff, they had to listen to the Pro Tip series. That's great. And some of the other podcasts, but then some of the re the rebounds she got from some of them was that guy on that podcast is Doctor bashing. And she said, he's not bashing you. You're just not doing the right thing? And he's saying? Absolutely, yeah. And I was like, wow, like, what a what a great person. Like, that's, yeah, that's the doctor you're looking for I made a mistake, you know, or I could have done something differently even, it doesn't even need to be a mistake could have just been best practice at this at a time. And now it's not any longer.
Speaker 2 22:16
You know, I had a diabetes educator, and this person does not have diabetes, just I'll preface it like that. Not saying that you have to have babies to be a good database educator at all. But I think in this case, that would have helped this person's perspective. She told me that I needed to be careful listening to this podcast, because it wasn't coming from. Like for you as an example. You're not a doctor, right? Doctor, I'm not anything. As you guys like, you should be really listening to like peer reviewed, you know, episodes and podcasts and stuff like,
Scott Benner 22:52
go right to sleep. Listen on that app, but go ahead. Yeah. So I thought that was hilarious. Well, one of the nicest things anybody's ever said to me is I do so for people who are listening who don't know, I do an episode I do management episodes. I guess I'll say it here. Like I'm the father of a child with type one. That's really all I am. My daughter's had type one diabetes, since she was two. And she's got she's going to be 20. This year. Her a one sees between five two and six to for like a decade now. And she doesn't have any diet restrictions. And a long time ago, writing a blog, I realized that I had a system that it wasn't confusing, and it was easy. And if I did these repeatable things, that I got repeatable results, and I used to write about them online, and I got, you know, feedback from people say, hey, this stuff really helps me. Thank you. Great. And then at some point, people stopped reading. And it was a weird shift in society. But people were like, why? If they can say it to my ear? Why am I using my eyes to read it? I'm like, Okay, fair enough. So I started making a podcast, which became incredibly popular. Yeah, if I had to guess, I think it's popular because it's entertaining. It's real. I don't have the ability to talk down to you. So I can't do it to begin with. And I fundamentally understand insulin and how to use it in almost a complete way. You know, but moreover, I have a way of explaining it, that is very digestible. And, and a lot of people a wide berth of people have shown that they understand the podcast and that it works for them. Yeah. And I'll just a second that. I
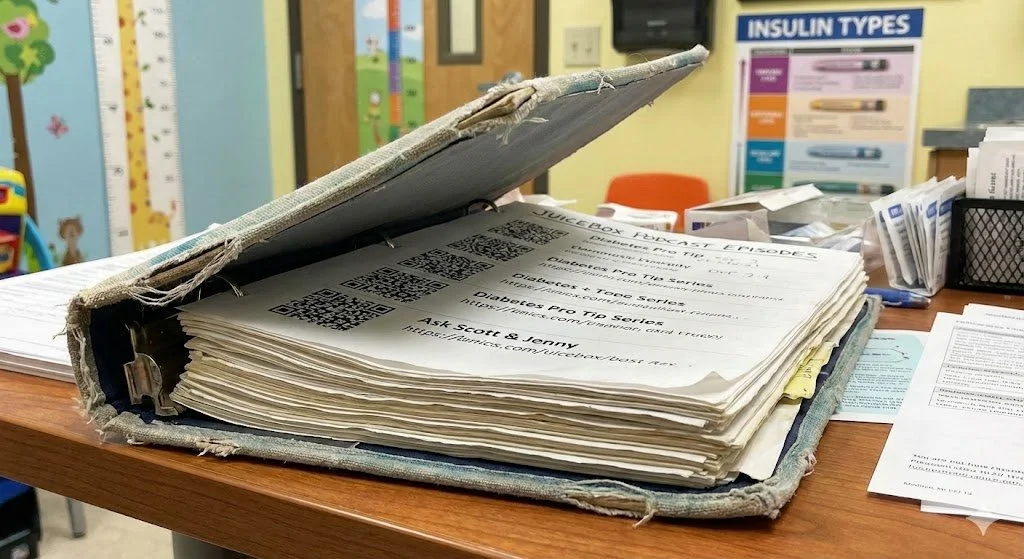
Speaker 2 24:29
mean, it does work. Oftentimes, in the inpatient setting, I only get to see someone for like a day, when I would like to really see them probably first three or four days in a row to make sure they're understanding everything. The way it is, I get consulted, typically, one to two days before they're getting discharged. Yeah. And so you have to pack everything and as much as possible, they're overwhelmed. That's why I always tell them about this podcast, especially at the beginning series. It's like, it really has changed people's lives. I've had emails from people saying like, Hey, I listen to that podcast and I feel like I really understand it though. It's, it's cool. So you're doing a good thing or without a doubt,
Scott Benner 25:03
you're very kind. And I appreciate that very much. But the thing here is like this podcast now has over 15 million downloads. Yeah, okay. And we interview people have diabetes, talk to doctors, you know, talk to people in industries, make pumps and that kind of stuff. But moreover, it's popular, because the information doesn't exist anywhere else. Like, if you're a physician listening now, and you're pissed, because there's a guy with a podcast, who's helping people, and you're not, you made the world that I succeeded. Like, if it wasn't for you, I'd have a different job. Yeah, I'm filling a void, you know, and so yeah, you know, that's the funny thing. Like sometimes when I get like that, oh, your doctor bashing, I'm like, You did this. Like, I didn't do this. I figured something out for my daughter. And then I saw that other people needed it. And then I figured out a way to talk to them to they could pick it up, because I'm not blowing my own horn here. But I don't get to sit in a room with people. I don't know their background. I haven't heard their story. And yet, I figured out a way to speak to them, that still helps them. And if I could do it, you have a nice car and you're handsome, and abs, like why can't you figure it out? Like you don't I mean, you went to medical school and all. So you'd think you could figure it out? If I could figure it out. I barely got through high school, George. And I'm not even kidding. The day I graduated, I was like, get the fuck out here. Really? All right. Yeah.
Speaker 2 26:28
But yeah, I mean, just real fast along those lines. I think so many people, especially our society, we put such a high level on academic intelligence. And that's just one level. I mean, you're a people person. Right? So you've got a high, I think, a social and emotional intelligence. And that's why this is helpful,
Scott Benner 26:48
right? It's not hard to help people, right. And by the way, let me say this, you're there anyway, you got up, you got dressed, you went to work, you're doing something wants to do the right thing. How would that be? You know, like, I mean, what a crazy fucking idea. Like, like, I'd be. You're already there. You're, you're functioning. But that's not specific to medicine, by the way, right? I know people who work in big industries, where people are being paid crazy money, and they'll spend more time trying to look like they're working than it would take to actually do their job.
Speaker 2 27:20
I know, I know. It's just it's just said that money is a lot of the time the big motivator, and I had a doctor, he wasn't an endocrine fellow. And he had prior been a pharmaceutical sales rep. And one day in passing, we were just talking briefly. And he thought this was funny. And I thought this was horrifying. He said, You know, when I was doing the pharmaceutical sales, I will just tell the patient whatever I needed to, to make sure that they'd get on that drug. But I don't believe that at all. Yeah. And I'm like, Are you kidding me? I
Scott Benner 27:53
can't wait. By the way, if you've used to sell pharmaceutical stuff, and you're a scumbag, and you want to come on the show, and talk anonymously, go ahead and contact me because I'd love to talk to you, too. I had a people will find an episode in this series with human resources professional. And the things that she told me she had to do in 25 years, all wrapped around finding ways to fire people who used up too much money because of their medical conditions. That was pretty horrifying. So Wow. Yeah. So let's hear more stories like this. And by the way, you've said this a couple of times, and I'd like to echo it. I don't think all doctors are are what these examples that you're giving? I probably overwhelmingly, that's not the case. Right? But if enough of them don't care, and enough of them don't know. And enough of them are busy being scored by their hospital need to keep their score up in order to get a bonus or not get fired or whatever is happening. Then your chances of walking into an institution and getting somebody who's on your side and knowledgeable. Go down. Right? And it doesn't mean that everybody's getting poor care. But a lot of people are right, you know, it this is this model that we've kind of created. It's driving good doctors away. Oh, sure. Like, one of my my friends at the hospital, he was, you know, I'm not gonna say his name. But he was actually listed as one of the top endocrinologist on your website. He just he left the hospital
Speaker 2 29:28
and went to a private practice in it in a different state. Yeah. And I was asking, like, where are you heading out? And he goes, Well, one family but you, I just need to get out of this place. And it's like, the pressure they were putting on him. He had essentially no life. Outside of the hospital. He told me that he was still doing patient prescriptions and all that stuff up to like 10 o'clock at night. Yeah, after working probably 10 hours on top of that, right. Yeah, right. Well, yeah,
Scott Benner 29:56
I mean, it's just obvious. Let me ask you a question. I I came under the impression my mom who's now passed, but a couple of years ago, was diagnosed with cancer. And the initial surgeon that diagnosed or would not do her surgery, which by the way, somebody else later did and gave her two more years of life. By and good years, bye bye. But the doctor wouldn't give her the surgery, the initial one. And I came under the impression that if she died, he would get nicked somehow in a scoring system that hurts him at work. Is that a real thing?
Speaker 2 30:35
I don't know. Personally, I wouldn't doubt it. I can't speak to that personally, though.
Scott Benner 30:39
But I got if a doctor knows about that, come on, and tell me about it. Yeah, I mean, I
Speaker 2 30:44
do know we have markers for everything. Right. I mean, everything's exam tracked everything like, like, are we washing our hands enough? Like there's there's people who are secretly watching everyone at the hospital? Keeping tally? It's like, oh, you know, he didn't wash his hands when he went in. And that's a tally. So there's there's things for literally everything. There's markers for everything. Hospitals have secret shoppers. Oh, without a doubt. Yeah. Oh, my gosh, about that. Yeah. And I know that because they signed me up to be one of them for the handwashing things.
Scott Benner 31:14
You're in charge. Now. George, go ratchet. And
Speaker 2 31:18
like, I don't I don't like I don't have to do this. Alright. Well, if you want to get the if you want to get the exceeds expectation on your performance, you need to be doing extra things. Oh, yeah. Yeah.
Scott Benner 31:27
So exceed, don't just be a nurse do something more. And by the way, rat on Patty over there, and let's get her out of here.
Speaker 2 31:34
Right. So stuff like that, you know, and listen, I did. When I was a floor nurse, I noticed that we had these snacks that were labeled as diabetic snacks, and it sounds like 12 grams of carbs. So I'm like, okay, cool. Well, then I'm looking inside the pack. And it says there's like, there's like, three packs of crackers. There's like a small apple. There was cheese. There was like, cashews like, those are mini bagel. And then I'm looking at the label from this company. It says 12 grams of carbs. I'm like that is so far.
Scott Benner 32:03
That can't be possible. Yeah, the apple off the apple is 12 grams of carbs. Right. Exactly, exactly.
Speaker 2 32:08
So I contacted the company. And I was like, and they're like, Oh, we noticed that this was inaccurate. But we'd already shipped out like 1000s to the hospital. So we're probably going to change it for the next one. So I got the got that all squared away. We had labels that fix the card count on it. And for that year, I just gotten meets expectations on the review. And I was like what I thought this was kind of bumped me up a little bit. And they said, No, you have to do something that's going to significantly save the hospital money to be able to get there exceeds expectations. Yeah,
Scott Benner 32:43
why don't you go run the parking during your break? Yeah, right. Yeah, go go park people's cars, do a little bit of that, you know, valet yourself a little, maybe you'll make some tips be fantastic. Right? When
Speaker 2 32:53
I was at this other hospital, it was the time where I wanted to make that transition into diabetes education. And so I put a proposal together, like pretty much what it would pay that kind of stuff. And they told me that they wouldn't go for it at the hospital, because it's not a significant return of investment for the investors of the hospital. So they have they elected to get new MRI machines that year, instead of hiring a diabetes educator, which I suppose in a sense, you're losing business, he talked to me because I tried to make sure that you're not going to have to come back to the hospital, right?
Scott Benner 33:28
But they said, Well, I'll buy a machine that we can build more we can build that that machine builds better than George does. That's basically the message
Speaker 2 33:35
Yes, well, that's the thing too, because I'm paying on a salary. So if I see one patient, I pay the same. And I if I see 11 patients on pay the same, I can't build because I'm an RN. They said that I basically a dying breed this role is a dying breed. Because we can bill you can hire a nurse practitioner or a physician assistant who can kind of do similar things, but then Bill, the patient for more money, essentially. Oh,
Scott Benner 34:00
so the idea is that they'll make nursing irrelevant because they can't bill for because the way the system is set up.
Speaker 2 34:07
Yeah. So the Florida is though they'll they'll still be there no problem. But like a specialty roles. So like, diabetes educator, so because I'm an RN, BSN RN, CDC, yes, that role is probably going to not be as popular to be hired at least because I can't bill. Okay.
Scott Benner 34:26
Yeah. Okay, well, alright, let's take a breath. Fine, everything's fine. Don't worry. It's all going to be okay. Good luck with your AI app is going to be your doctor in 10 more years.
Speaker 2 34:42
I wouldn't be surprised. You know, it's aI kind of freaks me out in some ways. In some ways. It's kind of cool. But I my brother in law, he's really big into it. And he's like, watch this. He's like, he highlighted an article that he read about diabetes meal plans. And then he put it into one of those aiops and said, Give me a diabetes. his meal plan that's easy for me to follow. And it's like, a minute spit them out before meal plan. And I'm like, I'm looking over it. I'm like, wow, that was that was kind of accurate. Oh,
Scott Benner 35:09
you want to hear something crazy? I have episodes that are called the math of Basal insulin math of this math of like insulin carb ratio and blah, blah, where we just have a conversation about how to do it, but in nope, at no part during the episode to somebody say, step one, take your weight step to do this. Like it's not like that, right? It's just a flowing conversation. And I've fed my own audio into my AI and said, How do you figure out somebody's Basal insulin? And it tells you? Oh, that's crazy. Yeah, from the conversation. So, but my point is, is that at some point, you're gonna sit down and tell something, this is how I feel. And it's gonna give you some possibilities, and then put you on the phone with a virtual doctor. Yeah. And you're gonna get an answer like that. And, you know, whether that ends up working or not, who knows? Right? What I'm hearing from you. Is that any conversation about how do we help the patient? How do we keep them healthier? is met with that doesn't make money. And so, you know, there's no answer here. Because money rules, money. Let me say something for people who may have some hope left. Everything's about money, or power. That's life. I'm sorry. You know,
Unknown Speaker 36:23
it's like the big three, I
Scott Benner 36:24
will say sex, money, power get perfect. The handsome doctor, if you don't need your nursing asked to tell him what to do. George like, he's a doctor. Yeah, ladies love me. I'm just here for the I almost said something I shouldn't say. But I feel like, that's it. Like, if you want to know why something's happening, it's a power move. It's a money move. Something to that degree. Now, not your personal life. I'm sure your mom is not making power, although some people are probably I don't know, my mom's doing. But like, you know, like, I'm sure the people you love are not doing that to you. But when you get out into the world, and you hear anything, if the first question you're not asking yourself is why are they saying that? I don't understand you as an adult? Yeah, yeah.
Speaker 2 37:07
So you know, yeah, and that's a big thing I tell my patients too, is, you know, you have to be able to take what I'm telling you process it and look it up for yourself to, I don't want people to take me 100% At my word, we're not giving them the information. It's, it's reliable information. But I want them to get in the habit of Hey, you look into this kind of stuff for yourself, too. You know, don't don't just necessarily take somebody's specifically straight up their word for that, that Yeah. And that's how you get like informed decision making. You
Scott Benner 37:39
have to, that leads into a completely different problem, which is that most people don't want to do that. Or they're not conditioned to do it, or they don't have the bandwidth to do it. They don't have the intellect to do it. There's a lot of reasons why people can't just pick up that baton and keep running with it. And making this podcast has taught me that. I'm not judging anybody. But there are countless reasons why people don't do well with their health. It's not the simple stuff that a bro podcast would tell you, like, you just ain't trying hard enough. Like you don't need like, it's not. It's not like, stop eating. Like, it's not like that, you know what I mean? Like most people are not just, I don't think that there's an overweight person in the world who's got a fistful of food, that's not good for them, that just is going I don't care about me. That's not how people think they're making decisions for a myriad of reasons that you don't know. And when it comes down to this diabetes stuff, you start them off with bad information, they have a bad situation, they either get incredibly scared of insulin, or, or something else happens and they do this throw, throw it up to God thing. They're like, Oh, I guess this is my life now, and, and whatever is gonna happen is gonna happen. You're ruining those people's lives. And it's needless, because if you just explain to them how to use insulin, and make sure they understand, they're going to have a better situation. But that's not what's going to happen ever. What's going to happen is that people are going to continue to make bad decisions that don't help people, because of, you know, preconceived human stuff. And this just keeps happening. I guarantee all those people in that renal unit that you were talking about at the beginning. Yeah. If I take most doctors to that unit and point to them and go look at all these poor people are gonna go out it's their own fault should eat better and exercise. You know what I mean? Yeah,
Speaker 2 39:29
that's, that's, that's the attitude. You know, I'm just blown away. Like, when I see patients, I try to see a blank slate every single time. And I'm not perfect. I mean, I'm a human. Obviously, I'm not perfect, but like, everyone is so different. Like yesterday, I saw a guy and he'd been dealing with high blood sugars and really bad low blood sugars. And so I just, I took some time, I was like, Hey, so what's going on? Tell me about your regimen at home. And he goes, Well, I take Lantis in the evening time, and I take insulin for my meals. And I said, okay, but tell me what insulin you take for your meals. And he goes, it's called 7030. And so he was taking 7030 mix to try to cover his carbohydrates. And that's like 70% of it is an intermediate acting like 12 to 14 hour insulin. Yeah. So it's no wonder that he's doing that. And then four to six hours later, a blood sugar of 20. Yeah, but I think, and he told me he's had diabetes for 15 years, and no one's ever told him. That is what he told me. It's 2023. How can that be possible? If you have someone who comes in the room very quickly, and the guy goes, Yeah, I mean, I take my long acting Lantis and then I take my insulin for my meals, if that's all they hear, and they'll take the extra second to go, okay, but clarify for me, what insulin Are you taking at the meal, right? Then you get into a situation, they're gonna say in the notes, okay, patients taking, you know, insulin with meals, consult endocrine, to figure out why he's having the lows. Yeah.
Scott Benner 40:57
It's funny. You were just told the problem. But you've went by it so quickly, that now you're going to start looking at 1000 other things. This happens all the time, by the way. Yeah, with diabetes. I've learned from making the podcast you say to somebody, Hey, how's your agency? And they go, it's good. Yep. And in the beginning, I went okay. And I just would move on from my interpretation of good, right. But it didn't take me long to say what is good mean? Yep. Because once they say that, you go, Oh, well, that's not good. Like, Greg, we're not going to call that good. Are we like your spiking in the 250s? And I'll say, but it comes back down. And I go, Yeah, but that's, that's doesn't have to go like that.
Unknown Speaker 41:35
Yeah, sure. Exactly. Yeah.
Scott Benner 41:39
Yeah, well, so when you're problem solving, the way I always think is, you need people to say the rest of the sentence, absolutely. Be clear, use all the words explained to me what's happening so that I can look at that and go, No, you know, what turns out, you're using the wrong hands on, hey, 15 years ago, you fix this guy's problem? Yeah,
Speaker 2 41:57
you know, and another thing I wanted to highlight real fast. So I do insulin pump trainings. Also, in the last year been noticing that there's been a trend of patients who should not be on pumps are being assigned pumps or given pumps. And what I mean by that is that that, obviously, there is a level of understanding that has to go into using an insulin pump. And if someone barely understands the concept of insulin, is not able to handle the technology, it's probably a good indicator that they shouldn't be started on a pump in that moment. And so that I'll get to the insulin pump trainings, it gets into really kind of scary situations, because then I'm expected to have this person start on the insulin pump. And then I'm, I'm worrying that they're, they don't even know what insulin really even does, you know, it gets these horrible situations like I've had, recently, there was a couple guys that were hospitalized because they didn't understand how to use it even after training and follow up. And I do have to say, I pin that one down on the doctor, because that was a poor assessment on their part to even say, Hey, you're you should be on an insulin pump.
Scott Benner 43:07
So it's back down to the core of why the podcast is popular because I explain to people how insulin works. Right? That's it. Yep. I had somebody telling me the other day, that my explanation of a tug of war for a meal Bolus is like the greatest thing that's ever happened to them.
Unknown Speaker 43:25
Oh, it's phenomenal. Yeah, that's a great example.
Scott Benner 43:28
Again, you know, I came up with that in my living room right. Now. I'm not reading a medical book, or you know, and I'm not, I'm not giving myself a ton of credit. I always just put you know what it is, I'm realizing talking to you. I was put into a situation where I was asked to help a person. I think I've been clear about this. In the past, I was talking to a very young mother. And it was clear to me that she had dropped out of high school because she found herself pregnant. And she was literally waitressing. And her young kid gets diabetes. She's struggling. And she's online looking for help. And no one knows how to help her. And someone points her to me and says that guy, I'll explain it to you like this is before the podcast, right? Like, it's probably just writing a blog back then. And I take my time. And I let her call me on the phone. And I let her tell me her whole story. And which, by the way, for doctors, interestingly enough, I've learned their whole story is not that important. Like, like, the details are important so that you know what they're doing, so that you can guide them well. But people have this desire to tell a bigger story. And I understand that on a personal level, but I get where doctors could be standing in a room going as part doesn't matter. Like, you know, you like I get that that happens because I've had it happen. But she explains your story. I assess who she is, as best I can. And I give her my best explanation about how to set this kid's insulin up. And she has the bravery to say I did not understand what you just said to me. And I had a moment where I thought I've just explained this to her are the best way I know how. And I was at a crossroads. I was either going to tell her I'm sorry, I can't help you. Or I had to figure something else out. You know? And in that moment, I said to her, I don't even know where it came from George, I really don't. I said, you know, have you ever been in a tug of war, like at school, you know, with a rope, and there's a flag in the middle? And she said, Yeah. And I said, Okay. Well imagine on one side of the rope is insulin, and on the other side of the rope is like food and carbs. And like all the things that make blood sugars go up. And she goes, Okay, and then I just restyled it. And she said, I get it. Thank you. That was it. I get it. Yeah. And then I spent time in my personal time, I have stood in this room, when no one's in my house, and said that out loud to nobody 25 times. Until it until it's a story, I can tell them. You could come up to me on the subway smack me in the side of the head point a gun at me and say, Tell the tug of war thing? And I'd be like, Okay, have you ever had a tug of war? Like, I would boom, go right through it. I wouldn't miss anything. A doctor can do that, too.
Speaker 2 46:06
Absolutely. Yeah. And you know, that's, I once I heard you explain that in another podcast. That's a common example. I use that with my patients to tug of war. It you're right, it makes people understand it. That a lot. A lot of people need those analogies to to understand these more complex topics, pictures.
Scott Benner 46:21
That's it. At the end of that, that story, as I'm standing in front of you like pulling on my own hands left and right to try to make the point about a Bolus. I go now imagine this, and I flip my arms from east to west and north south. And I think and I say, Now look, the insolence pulling down, and and the carbs. They're pulling up, and they're in a fight. And when neither side wins, that's a flatline on a CGM graph, and you should see people's faces go, Oh, my God, I got it. All right, just like that. Scott, who barely got out of high school, not that I wasn't smart enough. I was lazy. Let me be clear. Also, I was poor. And I was at work. Most of the time, I wasn't really working on high school. You know, I used to leave school in the middle of the day to go to a job at a sheetmetal shop to make $15. Like, I'd sneak out and not come back. And my boss would be like, aren't you supposed to be it's called like, as short a time clock need money?
Unknown Speaker 47:15
Right.
Scott Benner 47:16
Anyway? I'm sorry, we got a little off track there, but not really like so what exactly? Is there are effects that people on the ground? Can do? Or is it too stacked against them? A fix as in like for the providers or for the patient? So already it's too it's too confusing of a question, right? Because it's not it's not that simple. Right? Like, well, it's
Speaker 2 47:39
not it's not as simple. Yeah, I think I think if you want to just a straight answer the fix is you have to remove the straight business model of healthcare, it needs to be about actually helping people. And I think if we can get back to that, and get back to not having to force doctors to see X amount of patients a day to be getting good marks, rather, it's more of the the quality versus the quantity, I think. But the the issue is, and this is a huge, it's a deeper topic, but the way our our culture is, and I'm coming from the the US, we don't have a healthy culture. Yeah. And everything we do is like disrupting our endocrine system. And so that's fundamental. And we need to start the the foundations, the building blocks, and re teach people what is actual health and nutrition. And that will keep people healthier, out of situations where they're having to be in the hospital all the time, which would then mean that the doctors aren't having to see crazy amounts of patients in a day. So to answer your question, it's it's complex. I don't think there's just a straightforward way to fix this.
Scott Benner 48:53
So all we really have to do is take the money out of food and medicine and everything will be fine. Why don't we do politics at the same time while we're fixing the world? Right, exactly. Yeah, yeah.
Speaker 2 49:03
But if I could, if I could leave people with one thing I'd say, not necessarily rely as much on the sounds bad relying on the system. So if you can do things at your home, like making some of your own foods, maybe have a little garden, you know, things like that. That's going to be a starting block to getting you into a healthier lifestyle. Wow.
Scott Benner 49:25
Yeah. So no one's coming to help. I think so. Yeah. I listen, here's the other side of it. I wouldn't want people to be sitting in their easy chair tomorrow. Gone, ma'am. My shoulder stiff, My chest hurts, right? I just listen to that podcast. They said doctors aren't going to go to the hospital. Running yelling scream, My chest hurts. My arm hurts. So I think it does take it down to what I have noticed. Is that the bread and butter stuff, the stuff that happens all the time. hospitals aren't credibly good at managing?
Speaker 2 50:01
Absolutely. Yeah, you break your arm, absolutely run to the hospital, they're gonna fix you up really nicely, right? Yeah,
Scott Benner 50:07
I've seen that for sure. Like, as soon as you start adding variables, then then it gets a little dicey sometimes. And then all these other little things that we're talking about come into play, like when my daughter was in the emergency room, you know, a few months ago. And I watched them, I said to the nurse, I'm like, well, we want to do this. And they were like, Well, the doctor won't like that. And I said, I don't care. I was like, go, go, let's do it. I can't without asking the doctor. And I said, well ask the doctor, you know, I saw a fear on her face.
Speaker 2 50:35
Right, right. Because yeah, you know, you get I've been on the other end of that I've been a nurse talking to the patient where the patient is like, can we just do this, go ask the doctor, you know, and I ended up asking the doctor, and he's like, why are you calling me this is not an important thing. Just use the order set. And you're like, well, there's no order set. And as a as a as a nurse, you are taught that like, you follow the doctor's orders, you don't you don't do you don't become a rogue nurse, and just be like, Well, I'm gonna do this and this on my own, you got to get the doctor to sign off on it. Right? And maybe that means for a type one, it's like, Hey, can we do insulin to carb ratio? And maybe the doctor doesn't know how to even do that. Right? And the doctor is like, no, he's type one, he'll he needs six units with his meals. That's what he needs. Yeah,
Scott Benner 51:19
you don't realize how much of how people answer you is only based on what they understand, not what you're saying. Yeah, and,
Speaker 2 51:27
guys, I was gonna say, in that specific scenario there. Because I always tell my patient, I'm like, Listen, this is what the doctors recommended to you, it's your body, you can make the choice if you're going to choose to take the medication or not. Right. So you could, in theory, say I'm going to refuse six units, and I'm only going to accept four units. That's not me, that's not the nurse going over the order set, like you couldn't be like, I'm gonna take eight units. Well, the order is only calling for six, the nurse could not do that, that will get you in trouble. But if the patient says I only want four units, you're not breaking the order, because you're not going over the order. You could give the four units and then call the doctor and say, Hey, listen, this is what the patient wants, I
Scott Benner 52:13
wanted you to be aware that he didn't want the full six units. That's how you could handle situation. We know how difficult that is for people, though, right? Like, of course, the entire doesn't happen. It doesn't happen. Yeah, the entirety of the problem I see with people who have had diabetes for decades. And then. So what happens is that a long time ago, there was, you know, managing diabetes was not some exact science. And then that gets taught to people who have diabetes, and that colors, their personal life with it. But it also gets taught from doctor to doctor, and then that colors how care goes. And so like, and so nobody has a good answer. A lot of people are having problems. But they can't break the cycle, because nobody has the nerve to look at their doctor and say what you just said, like, I don't really want to do that. That doesn't sound right to me. And the real unintended consequence of that is that you kind of damned people to live an entire life, with their guts on fire, because they know they're doing the wrong thing. But you told them to do it. So they're doing it, like they're actually screwing themselves or hurting themselves on purpose. But they won't stop because you the person in the white coat with a fancy card, told them not to do that. And so they're just listening to you blindly. Right? Yeah.
Speaker 2 53:39
And that gets back to the whole? Well, if I've told them the wrong thing, 1000 times, I have to admit to myself that, yeah, I've potentially harmed 1000 people. And that's, that's a really hard thing to come to a realization to as a doctor, but I do think that some of my, the best doctors, I'd recommend, have looked at their practice and said, there's things I didn't know in the beginning and unfortunately, may have led to harm to some people. But now I do know this. And so I'm not going to go back to the way it was I'm going to go to the way that I learned to help and how to help people. Here's a difficult question maybe, that you may not know the answer to but sure, maybe you also might know the answer and not want to answer it. I'm not sure. But how much of not wanting to pivot has to do with liability. If I admit if I admit I doing it wrong, that I am admitting I heard, I heard somebody before then I think as long as you were practicing within the policy guidelines, you'd be okay. You're covered. You're covered. So, right. You know, you see a patient with type one diabetes, it's not going to the policy is not going to say specifics like okay, they need this much insulin. It's going to say a type one diabetic needs a long acting insulin and a short acting or rapid acting insulin with their meals. So if that's what you've been prescribing, maybe it's not the right way to prescribe it, but that's what you have been prescribing, you would be okay to then transitioning back. You know what, no, no, no, I need to go to a place where they should be. They should be like counting their carbs. Yeah. And being being aware of that, that I don't think they would get in trouble for that. Now, if they were if they were practicing with something completely outside of a policy, and then they admitted that to themselves, you would be potentially liable, right? Yeah.
Scott Benner 55:24
Here's the question. How pissed Do you think that organizations that exist now doctors, organizations, nurses, organizations, diabetes educators, like there's, there's big organizations that represent people they have? You know, you can go to conferences, and etc? Like, how pissed Do you think they're going to be that people like you were speaking up about this? Or do you think that quietly, they're gonna be like, thank God?
Speaker 2 55:48
I think there's gonna be some people who are thankful. I do think that some will be upset, though, for sure. Because I think if someone's not in the mindset of willing to change, and they're stuck in the old way of profit, profit business, well, some of the things that I'm saying, would lead to better diabetes care, which had been less interactions with the hospital. So less profit,
Scott Benner 56:10
even though that your work is in diabetes, like the things we're talking about apply across the board to other disease. Yeah, yeah. And, and issues, right, like, you're not saying anything that's like, this is super specific to diabetes, like, there's probably a lot of different care ideas that are following broken models and, and things of that sort. Right. And
Speaker 2 56:30
that's why I think you get some people who end up doing like a private practice, and say they, they won't accept insurance, you get into that situation, because a lot of times, the insurance companies dictate things about your appointments, right. As an example, we know some some midwives that do home visits. And if they were to accept insurance, the insurance told them that they could only have 15 to 20 minute appointments, but their whole practice is built around the fact that they're having hour, hour and a half appointments with their patients. Yeah, you know, and it's the same thing for other practices, other health areas, it just kind of sucks, it does, because the cost of everything is so high. So we need our insurance, to do things. But I think oftentimes, for people who really want to take back their health, they almost have to go outside of that. And that's, that comes at a cost.
Scott Benner 57:19
When Arden was my daughter was done being a child and had to move on to an adult endocrinologist, we looked around, but in the end, we went with basically a concierge doctor, and then we, you know, put some money aside to pay, you know, the, the bills, and then we have to submit it to our insurance. And then the insurance does reimburse us to be perfectly honest in a way that it's it's very affordable to do. It's not it's not actually a problem. And I know that wouldn't be everybody's situation pulling the money together to begin with, and we're having insurance that would reimburse, but, you know, the first time that I took her there, I said to her, and I'm like, You want me to go with you for the first appointment? She's like, okay, yeah, that'd be good. And because we, you know, three months earlier, we were sitting in a room with, like, you know, apple trees on the walls and stuff, and we're together anyway. So we go in, now you're in an adult situation, we're seated at some comfortable chairs with a, you know, a table in between. And there's a pad of paper there. And Arden just says, what is that? And the doctor says, oh, it's in case you want to write something down while you're here. And I thought, Oh, brilliant. Yeah. How many times you walk out of a doctor's office going? What do you say? What do you say, you know, and even that, like how was that because you know, those pronounce that the system gives you are mind boggling. And yeah, they're bad. That not helpful. Yeah. So she's like, Yeah, so I'm sorry. Just little little stuff that that takes time. And then from there, there was a point during the conversation, which is really what it was, Arden was having a conversation with a doctor as her first meeting with her. And, you know, like, there was a moment when I thought, are we taking up too much time? Like, oh, gosh, like, does she have to go? And I said, I'm sorry, are we here too long? Because no, no, you have an hour. And I was like, oh, okay, well, thanks. And then we got through a lot of other stuff that you wouldn't normally get to, and she got to hear more stories, and you know, anecdotal stuff about art and that she could she was taking away notes about and now when you talk to her, she's like, Oh, I remember that. Or didn't we talked about this a while ago. Let me go look, and then boom, I listened to what happened in real time on the phone. My doctor calls us, I don't know how to say this. Like, I want to be a little obtuse. It's so out of the ordinary. But Arden needed a medication recently. And it was a Friday evening. And the doctor, we were on the phone on a Friday evening at like 730 And she's going she's just chatting it through. You can hear there's people in our house like she's just you know, she's chatting it through with us. And she goes, Oh, you know what, I have a sample and And she goes, you can come to the office on Monday and she goes, Oh, you know what, though? It would be great to start it on the weekend. And I said, Yeah. And the next thing I know, I swear to you, I'm on the phone in the car, and I get a text. And it's from my doctor. It's her home address. And she says, we'll be up to about 11. That was that. I drove to her house, and she handed it to us on our front step. Wow. And I was like, This is what it must have been like a 1950. Without the texting, right. So you know, that's a person who cares about you. And it's not being rushed around? And you know, I mean, anybody listening to this, you're not getting that anywhere else. So no, that sucks. And I'm not saying that a hospital doctor, the hospital should be texting you their home address. Like it's obviously. Right. Yeah, right. But a tiny bit of that concern might go a long way. I'll leave this here with you. And then I'll let you wrap up, you know, this podcast doesn't just help people. It's actually a successful business. Okay, so all I did was say to myself, I'm going to help people. And if it makes money, that's great. And if it doesn't, I don't care. I never once focused on it being monetarily successful. But now it is. Because it actually helps people. And it's Yeah, I don't know that you can't do that. Do you know what I mean? Like, like, I want to help people. And like, I don't know, a Maserati. I'm not trying to say that, George, you don't eat meat, like, but like, we pay our bills. And you know, my wife works too. It's just not a single family, like, like structure, like for finances. But I am not in a pressure situation where I have to go find another job. I can actually help people and, and buy food. So it looks great. Yeah. But maybe that's not everybody's goal, I guess. Sure. Sure. Yeah. And you have to evaluate your goals and whatnot, too. But can I ask you, nurses? Yeah, just ethically? How many of them? Do you think we're like, I want to help people. And how many of them? Do you think we're like,
Speaker 2 1:02:06
I heard that pays. Well, I think the vast majority of nurses went into it saying I want to help people. Excellent. Because quite honestly, I knew it paid. Well. But there are so many other things that I could do to make a lot more money than what I'm doing right now. I mean, for goodness sakes, like you could recently I was like driving down the road. And there was like a fast food restaurant saying, hiring at like 21 bucks an hour. You were like, I can like fries. And I was like, when I got hired as a nurse. And this was not even, like 10 years ago. Yeah, it was, I got paid 27 bucks an hour. That was after going to college for four years getting passing the NCLEX. And so like, I think nurses, honestly aren't probably paid as well as they deserve. Okay. And so I think if you're a nurse, you're generally going into it because you want to help people.
Scott Benner 1:03:01
You don't think it's a thing that like, kids coming out of high school kind of blind blindly believe like, oh, it's it pays well,
Speaker 2 1:03:08
I'm sure there are some people like that. And hey, you know, if there's roles in the nursing field that pay insanely well, like, I know, I've got some people, some friends that are like single not married, they do travel nursing, and they make a ton of money doing that, right? For the standard nurse, she wants to maybe have a family and be in one location, you're not paid as highly as you think you would be. Nice. I'll just leave
Scott Benner 1:03:33
it at the icing. Okay. Does it attract people who don't belong in it?
Speaker 2 1:03:37
I think there are some people who definitely don't belong. Yeah, but I think the vast majority of nurses I work with, they probably do belong. But what I also say is the way everything is set up, it's almost inevitable that you're going to be jaded a little bit, whether that's to people's humanity, you know, that there's just things that happen that you kind of feel jaded. You know, I know after four years of doing bedside, I did x, I wanted to get diabetes experience across the spectrum, I wanted to see the worst of the worst before I started doing the education role. I remember I would come home and tell my wife, I'm like, Man, I just felt like a drug dealer today. You know, I feel like I'm feeding people's addictions, really? And so there. Yeah. Because, you know, and then it gets back into some of the patient satisfaction stuff, which is hospital profit. You know, pain is what the patient says it is. So I could be having a conversation like this with a patient and then he goes, Oh, yeah, you know, I got my morphine, you know, four hours ago. You know, I mean, 10 out of 10 pain now. And it's like, whoa, 10 out of 10 pain means you're not even having a conversation. You're basically in tears, but we're having we're joking around. Now, it's because the patient said that. He has that I have to give him the medication. Wow. People are going to be jaded, I think and you have to be pretty strong to be a nurse. I'd say. Yeah,
Scott Benner 1:04:55
I'd like to point out I guess this is a good time to point out that I know you're dealing with Apple two, and they're all the foibles that come with humanity as well. And it's not like, you know, it's not Mr. Rogers coming into the, into the ER, every five seconds, and everyone doesn't have best intentions and maybe they, you know, anywhere from seeking drugs to, you know, having treated their body terribly for 30 years, and now they're here and they're like, Yo, fix it. Like, that's not how this works. Right? Yeah, I take that point as well. I'm not saying that your actions are gonna fix humanity. I'm just saying, like, you have, like, you're, you're in control of the thing you do. Right, right. And speaking specifically about diabetes, but really thinking more holistically about about all kinds of disease sets, like, the path you put someone on, is the path they stay on, generally speaking. And so I've been making this point a lot. But if you're seeing somebody on the back end, in an ER, just remember that this is the end of a long path that also started with a doctor. Yeah, you know, and that person had a great opportunity to put them on a path that would not have ended them up in your ER, however, many years later, you know, so somebody's got to start doing the right thing if we expect anything to change.
Speaker 2 1:06:16
Absolutely. Yeah. You know, I, you said something in other podcasts where it was more or less like something that a doctor's says, Could haunt someone like the rest of their life. And even if it's just a little backhanded comment, and I see that too, you hear patients, you know, saying, like, I was diagnosed, and the doctor told me that I because I'm so overweight. That was the only reason I got diabetes, eight out, and then of course, they lose the weight, and maybe they still have it. And so they're just thinking the rest of their life that they're a failure because they were overweight. George,
Scott Benner 1:06:49
listen, most problems are because people don't communicate well. So that's so true. Yeah, sure. Just it's because you go find that person one day, and I bet you they're like, I just meant like, eat better. Like you don't mean like, yeah, exactly. I wasn't trying to shame you into feeling that way. But it done now. Like, you know, where are you going? I do a diary. About like, I use we go V I've been using we go V since March. It's December now I've lost 4040 pounds is like fundamentally changed my life. Every week, I sit down at this microphone for about five minutes. And I talk about the previous week, I shoot my week over and I shut the thing off. And about every 35 minutes, I put it out as an episode, right? Yeah, so I sit down last week to do what's going to be the last one of this episode, episode eight or nine, I forget. And I started talking about my week, which was I went shopping because I needed new clothing. Because I've lost weight. And before I know it, I'm crying in front of this microphone, remembering how terrible it felt to be a little fat kid shopping for clothes with my mom, and how much I hated going shopping and how I used to take it out on my mom. And now my mom's dead. And I can't even can apologize to her. You know, like, and I'm like, so that's that 45 years later, okay. And like, if you don't think as a doctor, you can't say something to somebody that if they were being honest with themselves, 45 years now would break them down into tears, like you're out of your mind, you know, like, like everything. And it doesn't mean that you're responsible for every way everyone feels. But there are big ideas that you could you could hit that would give people a better chance. And I'm not saying my mom did anything wrong. I'm just saying stuff sticks to you. And in ways that you just don't, you might not even recognize but that's colored my life in little ways. I only wear dark clothing. Like from my waist up. I'm very cognizant to just wear dark clothing from my waist up. My daughter took me out. And she's like, Here, put this on us. Like, I won't look good in that. And she's like, No, you will put it on. And I was like, okay, like so I was stuck having to be a good dad. So I put the shirt on. And then she pushed me in front of a mirror and I thought oh, this does look good on me. Like hot like she helped me like immensely, but I lived my whole life thinking oh, that's the wrong color all look fat in that. Oh, man. Yeah, you know, and so like, anyway, you say something to somebody. And you don't even mean anything by it. And there it is. But I'll tell you right now if I thought deeply enough, this has got something to do with elastic band of jeans that my mom made me buy. Because she was like, we can't keep buying you new clothes. It's too expensive. So here get these that stretch. Wow. And it just stuck with me. Like really? Really? And she What was she she was getting broke and she couldn't be buying jeans all the time. Right? Right. What was the real answer? Stop giving me a gallon of lemonade every day to drink and a bag of chips and like macaroni for Dinner and a giant pot like that. Yeah, but she didn't know. Right? That right. But here we are all these years later. So I don't know, George, you were really great. I appreciate this. Is there anything we haven't said that you you want to make sure we cover? No,
Speaker 2 1:10:14
I mean, I made I had a little list of things I want to send them we hit them all so good. That's
Scott Benner 1:10:18
excellent. I really appreciate you doing this. You know, we're gonna keep you anonymous, and do our best to change your voice so that nobody can even tell it to you. And I think you you really help people today and I appreciate you doing this. Yeah,
Unknown Speaker 1:10:33
I'm happy to have been here. Absolutely. Thank you. Yeah.
Scott Benner 1:10:45
A huge thanks to touched by type one for sponsoring this episode of The Juicebox Podcast. Check them out on their website touched by type one.org or on Facebook and Instagram. Aren't started using a contour meter because of its accuracy. But she continues to use it because it's adorable and trustworthy. If you have diabetes, you want the contour next gen blood glucose meter. There's already so many decisions. Let me take this one off your plate. Contour next one.com/juicebox The episode you just heard was professionally edited by wrong way recording. Wrong way recording.com.
If you're not already subscribed or following in your favorite audio app, please take the time now to do that. It really helps the show and get those automatic downloads set up so you never miss an episode. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!