#1013 Diabetes Pro Tip: Illness, Injury and Surgery
Scott and Jennifer discuss getting ready for a hospital stay with type 1 diabetes.
You can listen online to the entire series at DiabetesProTip.com or in your fav audio app.
You can always listen to the Juicebox Podcast here but the cool kids use: Apple Podcasts/iOS - Spotify - Amazon Music - Google Play/Android - Radio Public, Amazon Alexa or wherever they get audio.
+ Click for EPISODE TRANSCRIPT
DISCLAIMER: This text is the output of AI based transcribing from an audio recording. Although the transcription is largely accurate, in some cases it is incomplete or inaccurate due to inaudible passages or transcription errors and should not be treated as an authoritative record. Nothing that you read here constitutes advice medical or otherwise. Always consult with a healthcare professional before making changes to a healthcare plan.
Scott Benner 0:04
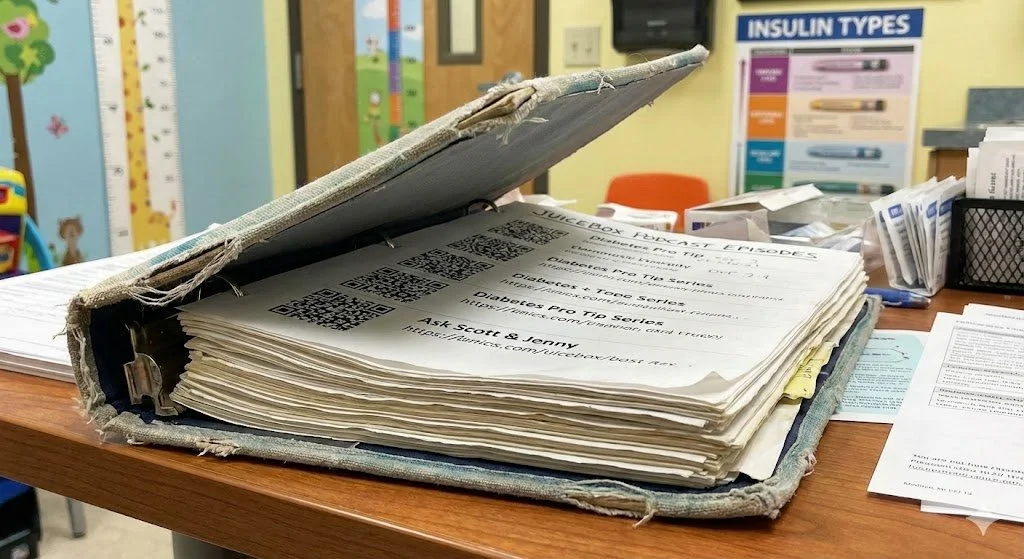
Hello friends, and welcome to the diabetes Pro Tip series from the Juicebox Podcast. These episodes have been remastered for better sound quality by Rob at wrong way recording. When you need it done right you choose wrong way, wrong way recording.com initially imagined by me as a 10 part series, the diabetes Pro Tip series has grown to 26 episodes. These episodes now exist in your audio player between Episode 1000 and episode 1025. They are also available online at diabetes pro tip.com, and juicebox podcast.com. This series features myself and Jennifer Smith. Jenny is a CD and a type one for over 35 years. This series was my attempt to bring together the management ideas found within the podcast in a way that would make it digestible and revisit double. It has been so incredibly popular that these 26 episodes are responsible for well over a half of a million downloads within the Juicebox Podcast. While you're listening please remember that nothing you hear on the Juicebox Podcast should be considered advice, medical or otherwise, always consult a physician before making any changes to your healthcare plan or becoming bold with insulin. This episode of The Juicebox Podcast is sponsored by assenza diabetes makers of the contour next gen blood glucose meter and they have an amazing offer for you. Right now at my link only contour next one.com forward slash juicebox free meter you can get an absolutely free contour next gen starter kit that's contour next.com forward slash juice box free meter. while supplies last US residents only. The remastered diabetes Pro Tip series from the Juicebox Podcast is sponsored by touched by type one. See all of the good work they're doing for people living with type one diabetes at touched by type one.org and on their Instagram and Facebook pages. This show is sponsored today by the glucagon that my daughter carries G voc hypo pen. Find out more at G voc glucagon.com. Forward slash juicebox. J Let's do a big Sick Day episode. And so I'd like to try if we can to get through sort of a regular sick day like you know, little beyond the sniffles the the flu a stomach virus, an injury like a broken bone or something I might have to take, you know, steroid for and then an actual surgery and have you where do I want to start? You've had a surgery pretty recently, haven't you?
Jennifer Smith, CDE 2:50
I've had multiple surgeries. I've had a week surgeries I've had I've been out surgeries. I don't like surgeries. But I've had them. Yes.
Scott Benner 2:59
So let's start there a because you got good information about it and be because Arden is going to have a cyst removed in a couple of weeks. So I'd like to hear about this. So let's start with something you were awake for. I guess also, like dental procedures would probably fall in this category a little bit maybe, maybe not,
Jennifer Smith, CDE 3:20
they could they would be a little bit different only because like a dental surgery if you're going to be awake for it like just a tooth removal or something like that. Usually, the awake component to it means that you don't really have to go in fasting or without any food in your system, you know, those kinds of things. If it were going to be a no now, they usually try to take all the wisdom teeth at once if they're going to do that. And oftentimes now I've heard a lot more people being completely put under my son was for wisdom tooth, you know, extraction, I didn't I my dentist said Your mouth is not big enough. You need to have your teeth come out, but there's nothing wrong with them as they come in, we're going to take them out. So as my teeth kind of came out and honestly my wisdom teeth didn't completely come through until I was well into my 20s and so they just took them out in office.
Scott Benner 4:25
I mean, I'm gonna make a note here to myself, because it has nothing to do with this. But my wisdom teeth extraction story is absolutely insane. And I will tell it at the end. So why don't we just made a note to myself. So okay, so if I'm just going to the dentist to have a cavity down or something like that. Not a lot for me to do probably handle things the way I normally do. You know, I guess
Jennifer Smith, CDE 4:49
your big thing to make sure is especially if you're new to having it done is and you've never had any like pain medication. No, you may experience a little bit of a higher blood sugar, potentially a stress component from having like the Novocaine. I mean, that needle is, it's scary, it's a scary looking needle that they're shoving in your mouth, right. And it doesn't feel very nice either, as they inject it several times. So for those of you know, those people who have never had this done, I, it's not very fun. And if you ever do have to have it fun, done, it's not a fun thing. But it could cause a rise in blood sugar because of a pain component, because you're just in a setting that's completely not under your control. So, but other than that, yeah, you shouldn't, you shouldn't have to go there fasting, or make any true adjustments to anything. You know, in the future, if you had a second surgery, or a tooth extraction or tooth work, and you knew what happened the first time, you could potentially look back, and maybe make adjustments like setting a Temp Basal increase, or taking a small amount of Bolus ahead of time to offset arise if you don't want it, or just correct after if you're not quite sure what's going to happen.
Scott Benner 6:07
Yeah, especially I'm thinking if, you know, if you're trying to, I'm not usually up for like, run high to avoid a low kind of situation. But if it's an hour, an hour and a half, and the dentist office, and it makes you comfortable, you know, let your blood sugar be a little higher for that. And then and then get at it. And because I guess too, if you're numb, taking in juicer gel or something like that could end up so you don't want to be in that situation be harder.
Jennifer Smith, CDE 6:29
Exactly. Yeah. So it's it mean, in some things like that, it sure it's a little bit safer to potentially be a little higher, if it does end up rising. I mean, obviously, don't go in at a blood sugar of 250, just because you're scared. But if it rises up, you know, higher than you'd love it to be, again, an hour hour and a half of being too high, you can correct it after without worrying that things are going to drop too much. And you can't chew anything, then that's okay.
Scott Benner 6:56
So this is so funny, I'm going to ask you, when I say leave it a little higher, I have a number in my head, what's your number?
Jennifer Smith, CDE 7:03
Let's say a little higher would be like 180 ish. Yeah,
Scott Benner 7:06
I might be insane. Actually. It's like, I was like, he could comfortably be 35 ish in there, I don't want to get crazy, that thing starts drifting to 160, I got a fight with it, then you know. But the point is, is wherever you feel like you can keep the control. And if you're real stable, that could just mean like dialing your Basal back a little bit to just let your blood sugar kind of come up a little bit, you might not have to eat something to make it happen. Okay, so that's simple. Now, moving on to the kind of the next step of it. Wisdom teeth knocked out cold. Now, I do know this from my son, if you get a good doctor, you're only under a very short time. But when you come back, you are not in any shape to make decisions. drink, eat, my kids said some crazy stuff on the way home from that doctor. And then even once his head cleared out, which I have to admit, didn't take too long. He's bleeding, his his mouth is packed with gauze and everything. So I guess we're in are we in that situation, now we're better high than low,
Jennifer Smith, CDE 8:12
it would be better than to be I mean, again, in that case, you know, if you went into that surgery to be put out and your blood sugar was nice and stable, let's say 120 even, it should for the short amount of time of that type of a procedure, it should remain stable, or it might climb again, from the stress on the body. In the aftermath of that, though, again, it would definitely be better to be a little bit higher than you're typically running. And again, I'm not saying like 180 200 High, obviously, you could correct to bring that down safely. But if you're running like 140 Leave it i that there is no detriment there whatsoever at 140 You know, as long until you can take something in or start to eat, or, you know, whatever the dentist told you for when you could start to eat again. I mean, even with my wisdom teeth being taken out one at a time, I think there was I think I had two taken out the first time it was a bottom and it was a top wisdom tooth. And I remember a couple of days of like just soft it was you know where the chewing component just was not pleasant. So having a plan of action to just like any other sick day kind of thing, having some things ready to go especially if you're an adult and you're taking care of yourself. You know having some soup or some broth or some jello or yogurt or popsicles or even ice cream or whatever it is that you can tolerate soft enough don't have to chew it that you can get something in.
Scott Benner 9:46
I think that I think that my as I'm thinking about this happening for Arden next year, probably my plan would likely be higher, not so high that it could get away from you higher but control And then if it tries to move, just kind of keep tamping it back down a little bit like so that you're in the power position, right? It's not out of control high. So that you're, you're going, Oh, geez, I have used a lot of insulin here. And it's not low, just you know what it tries to come up, push it back down, like, play, play that game for a little bit. So you've got the level you're looking for, but you're still reasonably in control of what's happening. I put yourself in a power position there, I think that's happened to handle it.
Jennifer Smith, CDE 10:25
That's correct. Considering the fact that as we've said before, the littler incremental adjustments sooner mean less insulin sitting there to potentially dump you down to low later. And then a setting where you can't actually take anything in, whether it's a mouth surgery, or this might even move in to kind of like stomach bugs or those kinds of things where you may not be able to take anything in or not quite sure when you can take anything in. It's it's certainly better to nudge little by little rather than take this big walk being adjustment and then you can't eat anything to offset.
Scott Benner 11:01
Yeah, I think bumping is the nudging is the way to go. That's i So as I'm considering it right now, for the first time talking to you. And when artists wisdom teeth come up, I think that's definitely what I'm gonna do. I'm gonna shoot for 140 in that range, take your advice over my advice, maybe more like 141 50. And then just keep knocking it down. If it's if it tries to run away, basically, just kind of keep tripping it as much as it tries to get up, I don't know.
Jennifer Smith, CDE 11:29
And find out ahead of time what her favorite soft or cold things are, so you can have them ready.
Scott Benner 11:34
Well, yeah, the pre like, you're gonna have to prepare, right? Like you're gonna hate. This is not something you're gonna want to think about after the surgery is over, you're gonna want this stuff
Jennifer Smith, CDE 11:41
like parking lot of the grocery store while you run in and be like, What did you want to get in her mouth is full of gauze. And she's like,
Scott Benner 11:49
I can't get her to pick food when she's not sick or injured. Like we were at the grocery store yesterday. I'm like, you just grab a couple snacks for lunch, whatever you're looking for. I don't know, you decide. And I said, How about those? She goes, No. And I went, Well, how are you going to tell me the side? And then I say something? He told me? No. I was like, what if I grabbed something that cheers if you show it to me, I'm gonna say no, if you bring it home, I'll eat it. And I went, Oh, that's a reasonable understanding of your psyche. I was like, Okay, great. So I did anesthesia impact at all.
Jennifer Smith, CDE 12:19
So some people, myself being one of them, not only do I have experience with surgery I've experienced with anesthesia, not my body doesn't like it. So again, if you're going into something where you've never had any anesthesia whatsoever before, just be aware that it can cause some like, post operative nausea. Many people get a little bit like woozy headed, I myself just don't tolerate it at all. I talked to the anesthesiologist ahead of time, I say, you need to load me up with whatever tools you have. Because I will probably throw up on the nurses when you get me awake. And there's only literally been one time that I had a I had a hernia surgery and umbilical hernia. And, man, if I could carry that anesthesiologist around in my pocket, if I ever needed surgery again, and his little toolkit of medications, he used post surgery, I was golden. I didn't feel horrible. I mean, you know, normal, but not like nauseous, whatever. So anesthesia can cause some nausea. So just be aware of that. If you know that's an issue, again, talk to the doctor about it ahead of time, there are many different kinds of medications they can use to stop that. And it depends, you know, on post surgery, sometimes they'll try to get you to nibble or drink a little bit of something in the post op when you're you know, recovering waking up. You can also be really really woozy, like in and out of like waking up and then getting really drowsy again and that it takes for everybody it takes a little bit of time to wear off. Usually in a post op setting. They'll probably have you in recovery for at least an hour. It could be longer than that, depending on how you seem to be doing. So it's I've always brought somebody along who knows how to look at my pump, how to potentially do a finger stick for me even though the nurses there could definitely do that for you. So my mom has come to a couple of my surgeries. My husband was there obviously for both C sections that I had. So it's really really really advantageous if you've got a go to person to be there after
Scott Benner 14:43
so funny. I alluded to this while we were recording recently, but you I have a question that's on the tip of my tongue. And if you would have paused I would have asked what you said. I'm like, one of us doesn't need to be here. I'm afraid it's me. So I was gonna say Did you wear your pump? And yes, you know, how did you take control of it? What did you do? So, as long as you were coherent, you were doing it?
Jennifer Smith, CDE 15:09
Correct. As long as I was coherent I was doing it's also really an ahead of time for any type of surgery. I mean, again, like a dental all kinds of things. Dentists could probably really care last as long as things are okay and controlled when you come in. They may if they know you have diabetes, they're definitely going to ask when you come in are your sugars, okay? Are they control? Are you feeling well, you know, whatever, they're not going to know anything about telling you to do or dial back or dial up or anything that's a dentist, people, doctors, though, will be more involved will be more involved. And they think it's really important thing to talk ahead of time,
Scott Benner 15:49
right? Because they're as a default, gonna just err on the side of I'd rather see your blood sugar be 300 for the next couple of hours, they're always going to feel that way. They don't really want to be managing your blood sugar. I really don't. Yeah, I've seen this now in multiple people in my life type two type one, you know, all the way down to my my friend Mike, who was in a, you know, in a coma at the end of his life. And they nobody would nobody? Gosh, I don't want to say they care. They didn't care. But it was a problem. They they weren't prioritizing, I guess, you know, it was a
Jennifer Smith, CDE 16:24
secondary issue. Yeah.
Scott Benner 16:26
They think of it that way.
Jennifer Smith, CDE 16:29
They're they're concerned. I mean, from the medical standpoint, in fact, if you don't address the fact of staying on your pump, and keeping your CGM on and whatnot, as long as you can keep them on, there are some medical procedures that include machines in the operating room that could potentially require you to be off of your products, just from a machine. I guess, interference standpoint, there may definitely be some things, there may also be length time of a procedure or a surgical procedure that determines you need to be on an insulin drip versus being left on your pump. So you know, those kinds of things, there is a definite difference. But for shorter lived surgeries. If you go in with your team, and you talk to them, and you say hey, you know, you know that I'm on an insulin pump. If you've got backing of your Endo, you can have your endo write a letter of approval for you to remain on your pump and your continuous monitor through the surgical procedure. Your doctor may even include in it, you know, glucose levels, we've, we've discussed, she or he will come in with a glucose level here to here, she or he will have a temporary Basal adjustment set, many doctors are a lot more conservative than you need to be for surgery. Many doctors will say dial the basil back by 50%
Scott Benner 17:52
just seems like a lot, again, which is a lot.
Jennifer Smith, CDE 17:55
And for most people again, there are the rare people who have a drop in blood sugar from that stress impact and whatnot. But it's not common. It's more common for stress to cause a rise in blood sugar. So, you know, dialing basil back kind of goes back to some of our other episodes about like testing things. If you're going into surgery, first thing, they will usually have somebody with diabetes on insulin, have surgery first thing in the morning, they will not push it into the later afternoon or the evening, mainly because they'll want you to come in in a fasting state. And it's easiest to get that in the morning for somebody with diabetes. They're in lies, do you know that your Maysles are doing what they're supposed to do? If you've got time?
Scott Benner 18:45
Well, yeah. Can you imagine to you're going to need to be fasting for a procedure at 8am and you wake up and your blood sugar's 45. What are you going to do? You know, you're gonna have to do something. And now you're gonna have to show up at the hospital and say, I drank juice this morning, and then they're gonna Bucha back out again and you have to reschedule. So, alright, that makes sense to so conversations ahead of time with doctors. I'd like to control my own insulin pump, I can do it when I'm on, you know, when I'm not capable. I've got a person here to help me. Here's a letter from my endocrinologist outlining you know, some of my goals for my blood sugar's that they'd like me to be able to stay on my devices. If I'm MDI, I don't want to be on a, you know, on an insulin drip, I want to, I want to inject my slow acting, you know, the way I always do, and probably having a little bit of, I don't know if charting is the word or records to be able to show the doctor like, look, here's what I do. Normally, I feel confident I can come in and accomplish this correctly is probably important
Jennifer Smith, CDE 19:45
because it eases their ability to also chart and say, you know, this is the plan of action. This is where you know this patient's glucose levels, they're controlled, the insulin doses are here. The glucose levels are huge. Willie here, this is where they came in the morning of the surgery, even showing them. I mean, every surgery I've gone into they've all the nurses have been fascinated with the continuous monitor. They've been fascinated with it. What happened
Scott Benner 20:14
to art and when she went into the emergency room for that belly pain, and you and I talked that they actually, yeah, and the other nurse who was way in charge, super confident and competent. And she, when she saw that thing, she's like, This is amazing. And I was like, Yeah, right. And she's like, alright, well, you know, what do you want to do? And I was like, I, you know, it was that moment. And I said, Listen, I'm not trying to be like, I'm not, you know, I'm not blowing a horn here or anything like that. I'm like, but my daughter is a once he is incredibly stable. On the lower side, her blood sugars. And I showed her like, this is her blood sugar for the last 24 hours. And like, I am completely confident that I can keep her blood sugar here. And if I can't, could we just do it? She's got an IV and right, you could hear you could hit her with, you know, yeah, with glucose. dextrose. Right. And so that actually happened, we were there for so long that they did have to run dextrose. And it was really interesting to watch, because it took forever to hit, and then it jacked her up. But if you gave her any insulin at all, it went right away in two seconds is very, very interesting to watch how it works. But when going into that scenario, right away, I mean, after we were settled, like I didn't run in the door yelling, she has type one diabetes, and we're gonna take care of it. Like, you know, after we were settled, you know, we were there for a little while. I'm like, Hey, listen, here's the situation. We'd love to stay like this. And that, to be honest, she seemed thrilled to let us do it. It almost felt like, well, then I won't have to do this. So perfect. You know, it was a little bit of that. And okay,
Jennifer Smith, CDE 21:44
that's actually for the most part, what I've actually what I've experienced, there's almost like you, you can't physically see it, but you can see it because with diabetes, we've become very intuitive to other people's like, what you can see them thinking you can like hear their gears going right. And every time I've come in for a surgery, I can almost like see the nurse let go. Their shoulders like relieved. They're like somebody has control of this. And we don't have to worry about I mean, they will, they will ask where your glucose is, if you do a finger stick or look at your CGM. Report it to them make sure that they know and are aware of where things are going. If you didn't at all make an adjustment to your insulin doses or take anything, make sure to note it to them so that they can chart it. Because it becomes part of the medical record then. But yeah, I mean, my, the my first child when he was born, we knew it was going to be a C section. And so we came in planned everything. And the nurse anesthetist who was there during the C section. She actually at that point in time, I had the receiver yet for my Dexcom. Right, I was still using it. And I she was holding it because my husband was like, you know, with me, obviously. And she was amazed by it. She kept like, she's like you changed again. He's like, that was 81. Like, yeah, it'll give you a new number every five minutes, right? Yeah. But she was like she was so just enjoying watching. She's like, this is a really steady line. And I was like, Yeah, that's what happens when your insulin is dialed in the right way.
Scott Benner 23:32
So you know, to your point, I'm recalling a conversation I had with a nurse in a hospital setting. And we talked about this. And she told me that one of the things she dreads the most is running up on somebody who really, you know, doesn't have a firm idea of what they're doing. And she's like, but that but it's, they feel like it's working for them. Yeah. And then you feel like you're in the position of explaining to them like, Oh, this isn't okay, this should be more like this or more like that. She's like, No, that's not my job. And you know, and they don't take it well, and they're already under stress over a lot of other things. And now here you are in the corner of the room going, Oh, by the way, you don't do a very good job of taking care of your diabetes, here's what you should be doing. She's like, it's not the right time.
Jennifer Smith, CDE 24:16
No, not at all. In fact, I when we went in for my second son's birth, you know, management had already been established endocrine and my MFM team had already written Jenny will manage, if she's unable her husband is here, he can help her manage, she will remain on her pump, et cetera, et cetera. And the nurses were really really surprised by that because they had had a woman the week prior, come in on a pump. And they thought she knew just like, you know what everything I was saying. They said, Okay, we need you to dial back, you know your rates by this much blah, blah blah because she didn't come in with a plan of action herself and This woman, unfortunately, literally didn't even know how to button push on her pump. So I don't I don't know the whole story other than the fact that the nurses and the doctors were like, well, we you can't safely we cannot allow you to stay on your phone. And so she was so excited. She's like, so glad you know what you're doing. Like this was the scenario we had.
Scott Benner 25:19
I hope hopefully, that'll this will give the confidence to other people to make these kind of like pre planning decisions to. Okay, so let's, you know, injury. And I only have one example. But Arden got hit really hard in the kneecap with a softball bat at softball ones. And her blood sugar began to rise almost immediately after the pain hit her and stayed up for the better part of 18 or 24 hours, she needed a lot more insulin now. You know, I don't think there's a lot to say to this other than there was an impact coming from her body that required more insulin, and I gave her more insulin. But that's Is that is that a hard and fast rule that paying put your blood sugar up in constant pain can hold it up? Or is that that's person to person? I would imagine to? For the
Jennifer Smith, CDE 26:05
most part, yes. I mean, as as kind of just a blanket statement. Yeah. For the if you're in pain, and it's considerable pain, blood sugar's will be higher. If the pain ebbs and flows, you may find a little bit of kind of a drop down as things feel much better. And if it starts up again, maybe between pain medication or whatnot, it may start to escalate again. So So yes, pain, pain is a horrible thing. You know. And that's actually one of the things that I in having had two births. The management of pain, post delivery, was, most women's insulin needs fall dramatically, after they deliver child and placenta and everything, and all those pregnancy hormones are gone. But after a surgical delivery, like a C section, or a more traumatic delivery, potentially, you may actually see that the stress of that, and the pain that you're in, could leave those glucose levels higher requiring more insulin, despite the pregnancy hormones being gone. So that's kind of a similar example. You're swapping
Scott Benner 27:17
the hormones for the pain. Right? Right. And I did see with Ardens needed when pain issues only taking Advil, but when it worked for she needed less insulin. And then at the end of that Advil if I if I didn't overlap it correctly, then she'd start to go up again. Okay, well, I just wanted to hit that. But now we're gonna, we're gonna jump into the like, the illnesses, you know,
Jennifer Smith, CDE 27:38
yeah. What Can I Can I comment on one thing, of course, prior to illnesses, as we've been talking about, like, planning for surgery, and all of those kinds of things, if you do have a plan of action, and you know, you'll be going into the hospital. The other things to definitively know is your length of stay for that, okay, because you do have to plan ahead for how much may you need to bring along as far as supplies, right, especially if you're on a pump. If you're on a CGM, you want to make sure that you have enough that you don't have to either send somebody home, the hospital will not have anything to help you out with your pump supplies,
Scott Benner 28:18
they're not going to offer you an omni pod, if you know,
Jennifer Smith, CDE 28:20
they're not going to they you know, I mean, certainly they've got glucose glucometers in the hospital, they've obviously got insulin, if you're really stuck on your type of rapid acting insulin for another example, and you've got something planned coming up, make sure to bring your insulin to the hospital with you, you may have to give it to the nursing staff, they may have to hold it in in the medical area with your name and label on it. But otherwise, you're kind of going to be at liberty of whatever's on formulary at the hospital and it could be the kind of rapid insulin either you've never used, or maybe it just doesn't work as well for you.
Scott Benner 28:56
Do you ever? Have you ever had an experience yourself or spoken with somebody who's had the experience where they go into the hospital, the hospital wants to leave their blood sugar higher. The people say I don't want that. But the hospital resists. And then the person sort of Mission Impossible style gets insulin to themselves because I've heard that from a lot of people. Like I had to I had to hide my pen from the nurse like that kind of stuff. Now that
Jennifer Smith, CDE 29:25
I'm sure she wouldn't mind me answering it because ginger who I wrote my book on type one with Yeah, you know, she is she is an MDI. She takes multiple daily injections. She doesn't use an insulin pump. And her first delivery. That's what she had to do because the nurses were like, We don't want to I don't know what they told her to take her insulin dose down or up by so much that ginger was like, that's gonna kill me. She's like, you can't do that. And so yeah, she had her like insulin pens in her room with her and When the nurses weren't in the room, she just dosed herself. Now, am I advocating for that as a health care professional? No, I'm advocating that you talk to somebody. But you know, what if in the case of the question that you asked if they're just leaving it, like so much higher, detrimentally higher than would be healthy for healing. I would advocate for bringing in like, a patient advocate asking the hospital to bring somebody into the room to talk with because there has to be a safe work around that. You're being safe in the hospital staff knows what you're doing, but that you're doing what you know is better for you.
Scott Benner 30:42
You know how this always happens. Because it happens in so many different walks of life in and around diabetes and separate over to, especially at school, by the way with, like how people take care of their children at school. There's this idea institutionally, this is how we do it. And when you come in and say, hey, that's really cool. I'm glad that works for people. I would like to do it like this. No, no, no, this is how we do it. But no one remembers why this is how we do it. Right. Like and it really is. It's the meatloaf story. You know, it's it's that I ever told you the meatloaf story. I've said on the podcast, it's here I'll do an abridged version of it. Mother and a young girl it's a pot roast actually mother and a young girl and making a pot roast. Mother gets out the pan cuts the ends off the pot roast, puts it in the pan sticks it in the oven. The daughter says Why did you cut the ends off the pot roast? Mom thinks for a second says I'm not really sure that's how my mom made pot roast. So they find the grandmother asked her grandmother says I don't know. You're gonna have to you know next time you're at the old age home, find my mom and ask her why. So they visit the old age home they find the mom she's 100 years old and all curled up in a ball. Great Mom, do you remember why we cut the ends off the pot roasts? You know, when we make them? And the old lady thinks and thinks and she goes? Oh yeah, I had a really short pan. Right? You know? Exactly. So. So you don't know why the hospital's saying what they're saying. You don't know why the school is saying what they're saying. And sometimes you just have to be reasonable, like you said, and talk and say, I get this is what you normally do. But hey, this is what we do. And look how well it works. Couldn't we? Couldn't we find a middle ground here? Correct. The problem is sometimes that communication breaks down because of I mean, I know on my end, when I would break down for me in the past, it's always emotion, like, you know, you're very emotional and you feel like oh, you're gonna, you're gonna ruin my kid's life or something like that, or you know, you're gonna hurt somebody and you feel and then you start wrong. And then before you know it, you're arguing. And so you have to really, you gotta come at it from a real calm place. But But that's, yeah, I'm not advocating anybody doing that either. I'm just saying that the number of people I know who have done that is more than I can count on my fingers. So something that kind
Jennifer Smith, CDE 32:50
of goes along with that, too, would be sort of an emergent type of setting where you come to the hospital unplanned, like an emergency room, right? Really important thing is that you if you can, if you're awake with it, or somebody who's with you can advocate for you. It's not odd for them to want to disconnect a pump, right? Do not let them disconnect your pump. Say that like more forcefully or whatnot. I mean, if you are with it enough, do not let them take your pump, right? Because they don't You don't know. I mean, emergency department personnel. They're, they're great clinicians, but they see a host of things like trauma problems, issues, whatnot, they are not schooled in insulin pump management, they're not. So that's a really, really important one.
Scott Benner 33:49
And these are emergencies that aren't the top end of the emergency, like if you're really injured. You know what, these people are going to try to keep you alive. You stopped thinking about your insulin pump now, but like that, that kind of stuff. But yeah, in moments where you're cognizant, it's, it's a weird thing. Like, why would you give over the control of your insulin pump to somebody just because you broke your toe and you're in the emergency room now? Correct? This doesn't make any sense.
Jennifer Smith, CDE 34:12
Okay, that's also the benefit of having a
Scott Benner 34:15
medical alert. Look at Jenny is wearing her bracelet, don't you? Oh, it's
Jennifer Smith, CDE 34:19
always on. I think actually, I glued it closed. Because I've lost it. It comes from American medical ID by the way, it's they do a great job. But my clasp had come like it unsnapped twice already. And I've had to reorder the same bracelet. So now it's glued closed. Like they would literally have to cut it off of me to get it off.
Scott Benner 34:42
I was gonna joke that Jenny is making side money by mentioning American medical bracelets on the podcast, and then she said it broke twice and I thought well, that's probably not what they want people to hear.
Jennifer Smith, CDE 34:52
Class I'm quite sure that it was, you know, my fault of catching it, whatever. It's just Yeah, it's so See, it's funny, because when I went into the hospital the last time for my kidney stone, it was not fun. It was a whole bunch of extra visits and whatnot after, but I told them I was like you. They wanted like all jewelry and like everything removed, and I was like, well, you're gonna have to cut it off then because it's glued together. And the doctor was like, Okay, well, we'll just put some, whatever it's called, like, coal ban, or KBN or whatever around it, and he's like, you're fine. We'll be
Scott Benner 35:29
fine. Oh, there you go. There's Jenny's had diabetes for 30 years, and she's wearing her bracelet now. Don't you all feel bad for not wearing yours? I don't even think Arden has one. So I'm feeling particularly bad in the moment. Oh, I'm sorry. You know, it's funny. It's when she gets older. Like, then I think of it like right now she's with somebody constantly. Who knows she has diabetes. It's you know, but it's those other moments. I guess it's the ones you can't plan for, you know,
Jennifer Smith, CDE 35:58
I've got a lot of friends who have gotten tattoos actually, you know, type one wrist tattoos. I've actually got a good friend in Michigan who she even talked to some EMTs. And she asked specifically about her design so that she could know from a medical perspective, would this be visible enough? Would this be recognized as a medical ID and whatnot. So there are some beautiful designs that are out there? I just have never one day gone that route. I have a tattoo but I just don't have a tattoo on my wrist.
Scott Benner 36:34
are we sharing where your tattoo is? Or no,
Jennifer Smith, CDE 36:36
it's on my leg. Okay.
Scott Benner 36:38
I have a couple of tattoos. I have one at the top of the crack and right now I'm just kidding. It's on my shoulder and one of my shoulder and one of my mine aren't that cool though. Maybe they are I don't know. I've had them for so long. That sometimes I look in the mirror and I see it and it startles me the one on my shoulder happens with on sometimes like what is on me. And then I realize that 25 years ago I got a tattoo and I don't I don't see it because it's behind me. Anyway, okay, so So let's start with the easiest version of a sick day right like a cold sniffles a cough like something that doesn't you know morph into something worse, just something that is you're under the weather. How does that does that always present with your blood sugar the same way it for you personally. The remastered diabetes Pro Tip series is sponsored by assenza diabetes makers of the contour next gen blood glucose meter and they have a unique offer just for listeners of the Juicebox Podcast. If you're new to contour, you can get a free contour next gen starter kit by visiting this special link contour next one.com forward slash juice box free meter. When you use my link, you're going to get the same accurate meter that my daughter carries contour next one.com forward slash juicebox free meter head there right now and get yourself the starter kit. This free kit includes the contour next gen meter 10 test strips 10 lancets, a lancing device control solution and to carry case but most importantly, it includes an incredibly accurate and easy to use blood glucose meter. This contour meter has a bright light for nighttime viewing and easy to read screen, it fits well on your hand, and features Second Chance sampling, which can help you to avoid wasting strips. Every one of you has a blood glucose meter, you deserve an accurate one contour next one.com forward slash juice box free meter to get your absolutely free contour next gen starter kit sent right to your door. When it's time to get more strips, you can use my link and save time and money buying your contour next products from the convenience of your home, it's completely possible that you will pay less out of pocket in cash for your contour strips than you're paying now, through your insurance. Contour next one.com forward slash juice box free meter go get yourself a free starter kit. while supplies last US residents only touched by type one has a wide array of resources and programs for people living with type one diabetes. When you visit touched by type one.org Go up to the top of the page where it says programs there you're going to see all of the terrific things that touched by type one is doing and I mean it's a lot type one it's school, the D box program golfing for diabetes dancing for diabetes, which is a terrific program. You just click on that to check that out. Both are caused their awareness campaigns and the annual conference that I've spoken at a number of years in a row. It's just amazing. Just like touch by type one touched by type one.org or find them on Facebook and Instagram links in the shownotes links at juicebox podcast.com. To touch by type one and the other great sponsors that are supporting the remastering of the diabetes Pro Tip series touched by type one.org. When you have diabetes and use insulin, low blood sugar can happen when you don't expect it. GE voc hypo pen is a ready to use glucagon option that can treat very low blood sugar in adults and kids with diabetes ages two and above. Find out more go to G voc glucagon.com. Forward slash juicebox G voc shouldn't be used in patients with pheochromocytoma or insulinoma visit G voc glucagon.com/risk.
Jennifer Smith, CDE 40:45
For me personally it does, I've found that just the typical sniffles I'm not really feeling bad, I'm just feeling kinda like stuffed up or something. Typically, I don't see any change in my blood sugars whatsoever, I don't see any change in my insulin needs whatsoever. It's not really until I start feeling sick, where I might feel a little more fatigued, tired kind of rundown, like I could go to bed like at 8pm instead of 1030. You know kind of thing that I like a good thing for me to know that I really don't feel good is that I just don't want to work out because I typically do something every single day for a workout. And if I really would rather like skip the gym, I know that I'm really not feeling great. But blood sugar wise, I've already I already know that I'm not doing great because I'll see an incremental creep excuse me, I usually need about 20 25% more insulin with something that's got me kind of just not feeling the best at all
Scott Benner 41:49
right so with Arden when she has the regular just sick day sickness she needs her blood sugar's are so easy to control those days. I don't like it not, not like I'm coughing and My chest hurts, or there's, you know, snot flying out of my nose or something like that. Just when she's a little under the weather. Her blood sugar's easier. Now maybe if I really delve into that maybe she doesn't eat as much during those days. But like there could be another reason that I'm wrong about. But I have heard people say, you know both ways I need more, I need less. And so for this right? Hydration really is got to be step one, in probably all of these right? You have to stay hydrated, keep food in, you know, as best you can. So you don't get into one of those deficits where you've got a bunch of insulin going and there's nothing inside of you and you drop quickly, is kind of morphing that from just a regular sick day to a slightly more sick day where you're under the weather, maybe have a bit of a fever is the biggest fear. What if I need to eat and I can't or what if I get sick to my stomach and my stomach empties like what do you think of the biggest fear around being sick as being
Jennifer Smith, CDE 43:00
I would say it's more the it's not like the congestion, the nasal the bronchitis, the ear infection, that's usually not, it's more the bugs that hit the digestive system that are the fear for most people, high blood sugars. Most people will realize that they need more insulin, whether they're just throwing insulin and correcting because they're staying high or they actually intuitively are like, oh, I need to bump my basil up. I'll use a Temp Basal here because I obviously I'm just running across the board. Hi, that's not so much the worry, it's more the Gosh, I really don't feel very good things could be coming out one or both ends and nothing really seems to be sitting well or you have consistent enough nausea that you can't really do more than a sip every hour. Yeah, those are more of the bugs that worry people. So I mean, there are there are some kind of hard and fast rules, you know, if your blood sugar is on the lower end declining or dropping, and you can catch it ahead of get being too low. You can if you're using an insulin pump, set a Temp Basal decrease about 80% for about two hours. So if you're really nauseous to the point that you can't take anything into stop that drop off, you can decrease basil enough again before you actually are too low to stop the drop and sort of curve you off until you could get a little bit of something usually extreme nausea doesn't last like nine hours at a pop. It kind of ebbs and flows through a stomach bug. So you know, at some point you can get in something even in the case of honey, you can put put honey in the gum and sort of just massage it in. You don't even have to swallow it but some of it does start to get absorbed in You know, through the mouth. So it's funny.
Scott Benner 45:02
So you just described exactly how I help Arden sleep in really long. So on a Saturday if she you know, she goes to bed late and or she's been really exhausted all week or something like that this Saturday is going to be one of those, like, she's got a lot going on this week, and I know she's gonna sleep in. There's a moment, like in the in the beginning of the day, the six o'clock 789 o'clock hour, it's like a 50% decrease in her insulin. And that keeps her at 90, right. But if she starts power, sleeping into that 10 o'clock, 11 o'clock, 12 o'clock, I sometimes have to go down to like an 80% decrease, just because everything in her body that could possibly keep her blood sugar up, is gone. Now it's just, it's really gone. She's been asleep for 12 hours, you know, 10 hours, it's really gone. So I've learned that I can't take all the insulin away. Because if I do that, she's going to jump up or be really high two hours after she wakes up or something like that. So you have to leave some in, but almost not enough for it to impact the moment at all, just for to help overall. And then from there. It's great. I mean, the idea of the honey in the cheek, something that doesn't make it to your stomach, because the lining your mouth is really absorbent for things. So your cheeks under your tongue, right? Yep, that kind of stuff. So you can get sugar in there without actually swallowing? I'll tell you, I'll tell you two in a panic situation, if you don't have anything even table sugar, you know, you can dissolve sort of in the saliva of your mouth and leave it there. Yep, yeah, there's a lot of ways you bet, you're going to have to get creative unless you're planning to head right, and you have sports drinks that you can take these kind of micro steps off of throughout the day, you know, but all we're talking about here is, is maintaining that balance with the extra variable of your stomach maybe being sour or incapable of holding the feet, right?
Jennifer Smith, CDE 47:04
When it comes to also prepping similar to other illnesses and whatnot, kind of, you know, like the discussion about mouth surgery, just prepping and making sure you've got some things on the shelf in your house, kind of, if it's popsicles that you always keep in the back of the freezer that have a sticker on that say, don't touch unless, you know, sick days, Sick Day stash, or whatever it is, there's actually a really good electrolyte. It's not pre mixed, it comes in like one of those little two, not tubes, but like packets, kind of like Crystal Light, almost. It's called Drip Drop. That one works really nice. I think each packet, if you'd consume the whole thing, it's only about like nine or 10 grams of carb. But the nice thing is that it's got the electrical light component to it too, for replacing what might be coming out. Yeah. So just some options.
Scott Benner 47:54
It's very dense with what you need to and I know about it for completely different reasons. But when Cole was recruiting for college, he got stuck at this three day event in August. And it was like 115 degrees. And he was playing baseball for three days in a row trying to you know, it's like, look at me, someone take me on their damn team, you know, but he was downing Pedialyte throughout the day to stay in that. So it is really impactful.
Jennifer Smith, CDE 48:22
The other component to stomach bugs and adjustments would be if you are able to take in a little bit usually because of stomach bug means that you're not absorbing well. Digestive leave, we really expect that you're probably absorbing only about 50, maybe 60% of the carb amount that you might be taking in one don't Bolus until you know that it's going to stay down. So in this circumstance, you're not doing Pre-Bolus thing at all. You take the food in, you make sure it's going to sit there, it's going to stay you Bolus only for about 50% of what you actually consume. This is a survival situation, right? It's a survival. And again, if you see it coming up sure that's where that like little bump nudge, kind of with a little bit more, maybe a little bit more whatnot, but be conservative to begin with. Because stomach bugs don't last long. They're not like the common cold five to seven days, maybe even 10 days. Usually stomach Bugs Are Gone within about a 72 hour time period, you may still have decreased absorption for days after you're feeling better. So don't don't think it's odd that you might be dropping a little bit low when you're back to eating what you consider normal food after meals. It might just be that your digestion is just not up to par yet. So
Scott Benner 49:37
if you're a person or a parent of someone who is prone to stomach issues, is having a prescription on hand for So Fran or something like that. Is that a good idea? Like something like an anti nausea medication? Yep. We'll talk about that.
Jennifer Smith, CDE 49:52
There's another one that's over the counter. It's called Emma trawl. e m e t r o l I think it comes in a lot. Little white bottle has got a rainbow on it. That was something that the, my second, my second wisdom tooth extraction, the dentist actually recommended for me for nausea, so and it seemed to work really well. So.
Scott Benner 50:17
So if I'm on MDI and I have this illness coming up, how do I cut back my, my slow acting insulin? Is it a percentage do you think? Or where do I start
Jennifer Smith, CDE 50:28
to, you know, it again, in the circumstance that you wake up in the morning throwing up or you know, just not feeling the greatest and you're taking your Basal dose in the morning, you can adjust it absolutely. And you can take it back by 10 20% as a starter. If it's really considerable nausea, and you're not really sure that you're going to take anything, and you may cut it back even a little bit more than that, and then just cover with boluses of your rapid insulin, if you are riding higher through the course of the rest of the day. But don't take an additional dose of your long acting insulin from what you missed. From the initial dose to make up don't just wait the next time you need
Scott Benner 51:12
to know. So you know, when you're talking about taking care of kids. I mean, anybody who's a parent who's had a child is sick, you realize, you know, for sure, like everything in your life stops, right? It worked doesn't matter. You know, the television show you really want to watch tonight disappears out of your life, you know, the weather doesn't you're you're keeping your kid alive. But But what if I'm an adult, and I'm alone, right? I'm living by myself and I have type one diabetes. I'm sick, and I'm exhausted. And I know I am going to fall asleep and stay asleep. Like, what what do I do before I fall asleep because that kind of illness you see people sometimes 10 hours, they're out like a light, right? And it's the kind of illness in the in the stress on your body. You might not wake up if you have a problem. And you don't want to be in that scenario. You don't even want to wake up with an extremely low blood sugar. I can imagine having a 40 on top of a stomach virus, right? It's gotta be horrible. I'm guessing. So do you do you ever? I mean, how long have you been married? You ever lived alone? Like, what would you do in that scenario? Would you?
Jennifer Smith, CDE 52:17
I've personally never lived alone. I either I went from my parents to having college roommates, to having off campus college roommates, too, then I think I lived alone for about a month between my college roommates moving out graduating and then getting married to my husband, your husband
Scott Benner 52:36
should take a lot of comfort in the fact that your face did not go Oh, geez, I do have to get divorced. Isn't that what Scott saying? No, no. Jenny has to fly. You look very comfortable.
Jennifer Smith, CDE 52:50
I've traveled alone. Right? You know. So in that circumstance, too. There are always like safety pieces. You know, when I when I travel alone, I actually set my CGM alert for a little bit higher over in the overnight time period, just because I want to know sooner than if my husband was sleeping next to me, because he's usually the one that hears it before I do.
Scott Benner 53:14
I got hit the shoulder last night. Don't you hear that? And I'm like, no, because I'm sleeping. She's like, it's beeping I was like,
Jennifer Smith, CDE 53:22
but for those living alone, I think some some strategies. Again, this would be a staying safe, by being potentially a little bit higher is actually better. So if you know that you are just like Dawn and you are out and you are gonna go to bed and you may not be up for the next 1012 hours. Just set a Temp Basal decrease. Or again, if you're going to bed at night, and you know that wake up in the morning at six o'clock is probably not going to be until 10 o'clock because how horrible you feel. Maybe you take your Basal insulin injection dose down a little bit. You know, I mean, there's safety things. Yeah, you may wake up higher than you want to be. But it's in this scenario of being alone. That would be the safer case. I mean, I'm not advocating obviously for waking up at 200 or 300, or whatever. But yeah, you wake up at 180 instead of waking up at 100. You know what, at least safe?
Scott Benner 54:19
Well, I mean, the idea is to get through this unconscious time period and back to back to conscious safely. That's what you're shooting for.
Jennifer Smith, CDE 54:27
The other component too could be you know, setting alarms on your phone, or setting an alarm clock in that time period just to wait I mean as much as you want to sleep in need the rest because you don't feel good. If you really are worried because you already took your Basal insulin and you can't adjust it now or you're getting to that point of just needing to lay down and you just had a meal and you're not quite sure what that Bolus is going to do for you. Set an alarm,
Scott Benner 54:55
right? Yeah, I mean, everybody should have an old $8 windup alarm clock they can pull out of a drawer right and send across the room so that you can't just reach over and touch snooze on your phone. Yeah. And, and get out of it that quickly. Okay. Well, that's, that's really, I think we're finding a lot of good ideas here. So real quick medications around illness, cough medicine, you know, they make some without sugar I guess or I could Bolus for like
Jennifer Smith, CDE 55:21
they do. It's called diabetic tossin. Diabetic tussen. That's what it's called.
Scott Benner 55:27
They really should just call it diet Tostan. But all right, I mean, I'm not a PR department over there.
Jennifer Smith, CDE 55:33
It's cough syrup that doesn't have any sugar added to it whatsoever does the same job but doesn't have any, you know, glucose raising component to it.
Scott Benner 55:43
Chris Rock in his stand up, it was like, rub some testing on it was that my mom used to say, Rob, so it was that? I don't remember figure out I'll figure that out. Okay, so diabetic Causton. What about is there? I mean, steroids. Steroids are going to push my blood sugar up the entire time they're in the body, right?
Jennifer Smith, CDE 56:04
Correct. Yes. And the increase can be considerable, depending on the dose. So injected, injected steroids, like a cortisone injection into a joint or something like that, those will cause considerable increase in blood sugar, definitely within the 12 hours after, you're going to need an increase at least 50%. Many times people see 100% increase. And then that that increase will last for a couple of days until the dose from an injection sort of starts to dissipate. I mean, the impact of it stays within the body, but the impact of the actual let's call it you know, cortisone, or whatever else has been injected on what other kind of prednisone or whatever it might be, it's going to dissipate enough that you're going to see the need for that increase in in Basal dose come back down. I, you know, it's, it's not odd to see 100% More 150% More Basal dose, especially, many people who are also paying close enough attention will often also need an adjustment down in their insulin to carb ratios, their correction factors. A, as far as oral steroids, depending on the dose, and again, on a potential hard stop or a taper of the dose. Most often, those are people who have like a bronchial illness, and they have like a background like asthma or some other type of lung condition that the doctor really wants to attack the illness to prevent pneumonia or something else, you know, progressing. Those types will usually again, increase the need significantly, and the insulin to carb and the sensitivity factor will need to be adjusted.
Scott Benner 57:59
Okay. And to medications that may have a side effect of nausea, you should be careful about if they want you to take them with food, give yourself a chance to not show up, you know, not make yourself nauseous when you when you might need to hold something down. I want to double back a second to the idea of an alone adult or even a kid whose parents, you know, might feel like it's slipping away. Like, when do I it's so funny to ask this question, because we spent some time talking about the fact that hospitals don't seem to particularly you know, value, like your blood sugar that much. But that wins the moment when you wave the white flag and go to the hospital. Like Like when am I like, you know, not that you should be running every time you're sick. And by the way, I feel terrible. Because some people get sick more frequently than others. I can count I can count on two hands. The times both of my children have been ill. Arden doesn't get sick much at all. Which by the way, too, for those of you who do, what a horrible joke that is from nature, right? Your immune system was strong enough to beat the crap out of your pancreas. Can't make bronchitis go away. Right? Yeah, like whoa, come on, man. But But So when do I like what's the Mendoza line for when I think I better get the professional help. And why do I want to do that? Like what is it I'm avoiding?
Jennifer Smith, CDE 59:18
That kind of comes in and I know we had a whole discussion, an episode all about ketones and how to look at that and whatnot. But that kind of brings that into the picture as far as blood sugars and or hydration. And if you are ill and you're really not feeling good check ketones. You know, because in the case of moderate to high ketones, those often especially if you are not feeling well and you can't get enough hydration and fluids in you may very well need to go to the emergency room. In that case, it's just and your blood sugar's may not look like high enough To say, Well, gosh, I This is really bad I have to go to, you know, to the emergency room or the hospital. But if your ketones are at that moderate high level, you definitely need some help clearing those or you're going to be in trouble and IV would help with that, right? Is that IV would help with that, because they're not gonna make you down a whole bucket of water via your mouth, because I have could put an IV in and they're going to push it in through your vein, because if
Scott Benner 1:00:27
you could, you would, too. And and I know I know that because and I think I've told this here before, but Arden woke up one time with should have bent cannula, one bent cannula, and like 14 years is amazing. But she will come it's pretty. She woke up with a higher blood sugar. She was nauseous. I tested her ketones. They were high. And I said to her, I'm like, Look, here's your options. Now she wasn't sick. Like, you know, I mean, shouldn't have a stomach vise. I said, you pound this water down. I crush you with insulin. And you promise me that you can eat something to stop the fall. Right? Like and or we're going to the hospital. And and she's like, and she took a bottle of water for me and Arden is I've mentioned this here before she's a princess slipper. When she drinks water. It's like, Oh, little bit a little bit. She took that bottle of water. And she pounded it all down. And she was like, is that good? And I went yeah, you can sit with the next one, you know, and we got like three bottles of water in or over two hours. We made a big Bolus. She, her blood sugar broke, and her ketones began to fall. And we caught it with a little bit. We caught it with something. And that was it. It took us three hours to not go to the hospital. But she was willing to do it. And it was hard. She told me later that drinking that water was incredibly difficult because of the pain she had from the elevated ketones. Yeah, she was she felt very nauseous from it. Obviously, she wasn't sick. But yeah, at some point, there's going to be a safety issue, please don't get to the point where you're calling an ambulance, you know what I mean? Like, like, you might have to give up at some point. Right?
Jennifer Smith, CDE 1:02:06
This kind of, it kind of brings into it. A component of like nausea in pregnancy can be a very considerable thing for some women, especially in early pregnancy. So if you have significant enough nausea, and you're not literally able to take things in, or you've gotten to the point of actually vomiting, because of the significant nausea, it's always better to try to go and get at least IV hydration so that you don't run into an issue of ketones. Even though blood sugar levels may not be elevated in that circumstance. You could develop ketones mainly because you're just not keeping anything in. And that's very, very, very bad in pregnancy.
Scott Benner 1:02:57
Can I ask you a question? And I don't usually put you on the spot for this because it's a question about how to do the podcast. When I put this episode out, I was thinking to put the ketone, defining ketones right with it. You see them as compact these are companions to each other. Okay, absolutely.
Jennifer Smith, CDE 1:03:12
That's a great idea.
Scott Benner 1:03:13
We'll definitely do that then. This is usually the time where I say Is there anything I didn't say that I should have said
Jennifer Smith, CDE 1:03:20
the only thing I would say is for all of this the biggest thing comes from like my years with Girl Scouts be prepared. Okay, great to be prepared. And one of the best things I can recommend doing is having you never know when you're going to have to run out the door to like an emergency like situation right or even in the case of I know this is an illness specific but this is like just being prepared like you have to run out of the house because I don't know your stove is on fire. I mean, if you have a diabetes emergency bag packed get a backpack or red backpack cheap go to Target or wherever get one put in it. All of the things you could potentially have to take with you quickly out of the house. It'll be a lot easier in a an illness emergency especially especially somebody has to take you out of the house right? If you got stuff packed to go at least you know you've got you know, a set change and extra test strips and batteries and whatever they're all in.
Scott Benner 1:04:29
So a Jumanji situation when giant vines and lions are going through your living room and you really need to get out. You want to be able to grab this bag. Correct and at least have it packed somewhere and no, it doesn't have to be hanging by the back door chasing you through the kitchen. We're very mean in that movie. Hey. I know Robin Williams and now now people are like Robin Williams wasn't in that movie. That was the rock. How did you confuse those things? And who is Robin Williams but there's been two Jumanji movies so young people please leave me alone. I want to close As by saying that as we were talking, I was proudly struck by how much of what is normally spoken about on the podcast translates very well to this idea of sick days. That, you know, obviously, there's heightened scenarios, but that the tools you use really aren't much different. You might use different ones in different times than normal, but, but it's not like. And the reason I say this is because when people are trying to figure things like this out, I oftentimes see them believing that there's some extra special knowledge that they don't have about diabetes that applies only to the day you're sick. And I still think that one of your greatest diabetes tools is common sense. And so I think that, you know, we obviously broke things down a lot more granularly here, but it's still the tools. It's the Pro Tip series, you know, applied slightly differently. So right, um, I thought this was really terrific. I appreciate you doing this. And we talked so long that I can't ask you to define Lada so I'll do that next time. Okay, so that you can go I will say thank you. You're welcome. I want to thank assenza diabetes for sponsoring the remastered diabetes Pro Tip series. Don't forget you can get a free contour next gen starter kit at contour next one.com forward slash juicebox free meter, while supplies last US residents only. If you're enjoying the remastered episodes of the diabetes Pro Tip series from the Juicebox Podcast you have touched by type one to thank touched by type one.org is a proud sponsor of the remastering of the diabetes Pro Tip series. Learn more about them at touched by type one.org. A huge thank you to one of today's sponsors, G voc glucagon, find out more about Chivo Capo pen at G Vogue glucagon.com Ford slash juicebox. you spell that GVOKEGLUC AG o n.com. Forward slash juicebox. If you're living with diabetes, or the caregiver of someone who is and you're looking for an online community of supportive people who understand, check out the Juicebox Podcast private Facebook group Juicebox Podcast type one diabetes, there are over 41,000 active members and we add 300 new members every week. There is a conversation happening right now that would interest you, inform you or give you the opportunity to share something that you've learned Juicebox Podcast, type one diabetes on Facebook, and it's not just for type ones, any kind of diabetes, any way you're connected to it. You are invited to join this absolutely free and welcoming community. I hope you enjoyed this episode. Now listen, there's 26 episodes in this series. You might not know what each of them are. I'm going to tell you now. Episode 1000 is called newly diagnosed are starting over episode 1001. All about MDI 1002 all about insulin 1003 is called Pre-Bolus Episode 1004 Temp Basal 1005 Insulin pumping 1006 mastering a CGM 1007 Bump and nudge 1008 The perfect Bolus 1009 variables 1010 setting Basal insulin 1011 Exercise 1012 fat and protein 1013 Insulin injury and surgery 1014 glucagon and low Beegees in Episode 1015 Jenny and I talked about emergency room protocols in 1016 long term health 1017 Bumping nudge part two in Episode 1008 teen pregnancy 1009 teen explaining type one 1020 glycemic index and load 1021 postpartum 1022 weight loss 1023 Honeymoon 1024 female hormones and in Episode 1025 We talked about transitioning from MDI to pumping. Before I go I'd like to share two reviews with you of the diabetes Pro Tip series, one from an adult and one from a caregiver. I learned so much from the Pro Tip series when our son was diagnosed last summer. It really helped get me through those first few very tough weeks. It wasn't just your explanations of how it all works, which were way better than anything our diabetes educator told us. But something about the way you and Jenny presented everything, even the scary stuff. That reassured me that we could figure out how to deal with us and to teach our son on how to deal with it too. Thank you for sharing your knowledge and experience with us. This podcast is a game changer 25 years as a type one diabetic, and only now am I learning some of the basics, Scott brings useful information and presents it in digestible ways. Learning that Pre-Bolus doesn't just mean Bolus before you eat but means timing your insulin so that is active as the carbs become active, took me already from a decent 6.5 A one C down to a 5.6. In the past eight months, I've never met Scott. But after listening to hundreds of episodes and joining him in his Facebook group, I consider him a friend. listening to this podcast and applying it has been the best thing I have done for my health since diagnosis. I genuinely hope that the diabetes Pro Tip series is valuable for you and your family. If it is find me in the private Facebook group and say hello. If you're enjoying the Juicebox Podcast, please share it with a friend, a neighbor, your physician or someone else who you know that might also benefit from the podcast. Thank you so much for listening. I'll be back very soon with another episode of The Juicebox Podcast. Jenny Smith holds a bachelor's degree in Human Nutrition and biology from the University of Wisconsin. She is a registered and licensed dietitian, a certified diabetes educator and a certified trainer on most makes and models of insulin pumps and continuous glucose monitoring systems. She's also had type one diabetes for over 35 years and she works at integrated diabetes.com. If you're interested in hiring Jenny, you can learn more about her at that link.
Please support the sponsors
The Juicebox Podcast is a free show, but if you'd like to support the podcast directly, you can make a gift here. Recent donations were used to pay for podcast hosting fees. Thank you to all who have sent 5, 10 and 20 dollars!